Introduction
The beach chair position (BCP) is typically used during shoulder arthroscopic surgery due to upright anatomic position, ease of examination under anesthesia, and arm being positioned away from the anterior portal (i.e., no need to reposition or re-drape to convert to an open) [
1]. However, risks include significant hypotension, which can lead to cerebral hypoperfusion and neurological complications; cerebral ischemia, cranial nerve neuropraxia, pituitary apoplexy, and cardiovascular collapse have been reported [
2345].
Shoulder arthroscopic surgery can result in severe postoperative pain; however, combining general anesthesia with an interscalene block (ISB) or a single use of ISB provides effective postoperative analgesia [
6]. Vasoconstrictors, usually epinephrine (5 µg/ml or 1 : 200,000), are frequently included in local anesthetic solutions to decrease vascular absorption, thereby allowing more anesthetic to reach the nerve membranes, improve the depth and duration of anesthesia, and provide a marker for inadvertent intravascular injection [
7]. However, absorption of epinephrine into systemic circulation can increase blood pressure (BP) and heart rate (HR).
This study determined the effects of epinephrine mixed with ropivacaine for ISB on the hemodynamic changes related to BCP.
Go to :

Materials and Methods
Study design
This was an Institutional Review Board (IRB) approved retrospective study that included all patients undergoing shoulder arthroscopic rotator cuff repair surgery in our center between March 2013 and August 2014. The starting point for the study was chosen based on completion of a new operating room for arthroscopic surgery, as all shoulder arthroscopic surgeries were performed under the same conditions by one surgeon, and anesthesia was induced by one anesthesiologist-team. The IRB waived the requirement for informed consent due to the retrospective nature of the study.
We divided all data into three groups: 1) only ISB, 2) I+G (general anesthesia after ISB without epinephrine), and 3) I+E+G (general anesthesia after ISB with epinephrine).
We compared HR and mean blood pressure (MBP) among the groups.
An electronic medical record system, used in our center since 2011, recorded all vital sign data automatically in 5-min intervals. The vital signs were always checked before ISB, which was set as the initial time to collect vital sign data every 5 min for 30 min.
Exclusion criteria
The data exclusion criteria were cases that received only general anesthesia without ISB, cases in which continuous ISB was used, and cases with missing vital sign data.
Anesthetic technique
Patients were premedicated intramuscularly with 0.2 mg glycopyrrolate 30 min before transport to the operating room. Electrocardiography, non-invasive blood pressure monitoring, pulse oximeter, bispectral index (BIS) monitoring, and capnography were used to monitor the patient's vital signs. The BP cuff for non-invasive blood pressure monitoring was routinely placed on the non-operative upper arm. A plasma solution was administered at a rate of 10 ml/kg/h.
Initial vital signs were checked after all monitoring instruments were attached to the patient. Ultrasound (MyLab 25 Gold; Biosound Esaote, Indianapolis, IN, USA)-guided ISB was performed after the vital signs stabilized. Ultrasound was used to confirm the proximity of the needle to the nerve. Only 20 ml of 0.75% ropivacaine was injected into the interscalene space in the I+G group, whereas the I+E+G group received 100 µg of epinephrine mixed with 20 ml of 0.75% ropivacaine. The I group received of 1% lidocaine mixed with 20 ml of 0.75% ropivacaine. No complications were caused by the ISB.
General anesthesia was induced in the I+G and I+E+G groups with 1–2 mg/kg of propofol and 0.8 mg/kg rocuronium for the neuromuscular block. Remifentanil (0.1 µg/kg/min) was administered for the balanced anesthesia technique. The trachea was then intubated, and mechanical ventilation was provided with an oxygen/medical air mixture (50% oxygen) to maintain 30–40 mmHg end-tidal carbon dioxide pressure. We used sevoflurane during surgery to maintain a BIS score of 40–60. The remifentanil infusion rate was regulated to maintain a MBP at 80% of the initial value. If the MBP decreased below 60 mmHg, 50 µg of phenylephrine or 5 mg of ephedrine was administered as a bolus dose. If the MBP increased over 110 mmHg, nicardipine (0.5 or 1 mg) or labetalol (10 mg) was used to improve the arthroscopic view.
The patient's position was changed from the supine position to the BCP after general anesthesia was induced. The position of the I group patients was changed after confirming the ISB with ice.
Statistical analysis
A statistical analysis was done using R ver. 3.3.1. The statistical tests were two-sided. Patient characteristics were compared using one-way analysis of variance (ANOVA). Categorical variables were compared using Fisher's exact test. MBP and HR were converted to a linear mixed effect model using the package lme4; the model coefficients were compared using the lmerTest package (F-test). The Shapiro–Wilks test was used to test for normality and the Bartlett test was used to test for equal variance. The mixed effect model was fit using the maximum likelihood criterion, and ANOVA was used to select the final model. Group, time (slope), and intercept were used to evaluate fixed effects. Each correlated intercept and slope was used for random effects. The model included the linear term and quadratic term of time, and the interaction among the groups. P value < 0.05 was considered statistically significant.
Go to :

Results
Demographic data
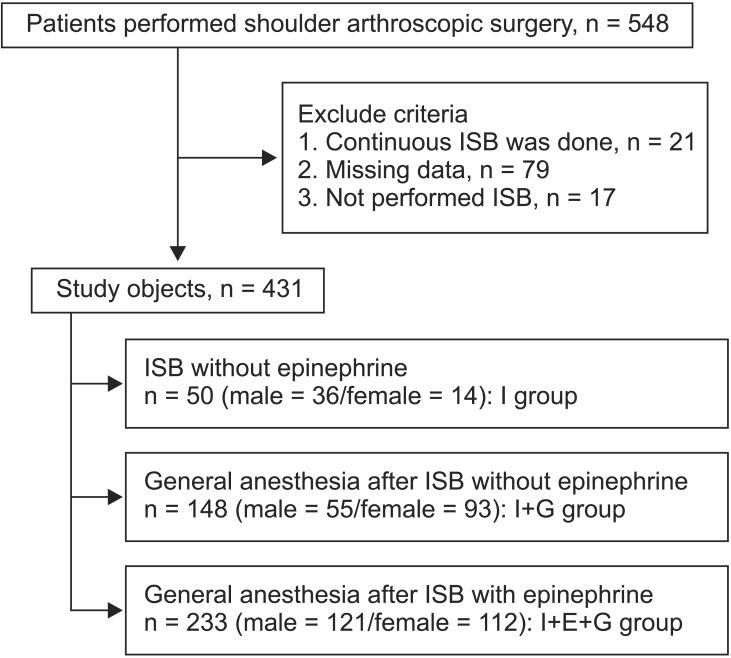
During the study, 548 patients underwent shoulder arthroscopic surgery. We excluded 117 cases: 79 cases for missing data, 17 cases that underwent general anesthesia without ISB, and 21 cases that received a continuous ISB (
Fig. 1). No differences in age or underlying diseases were detected among the groups. The sex ratio differed among the three groups. Significant differences in weight and height were observed (
Table 1); this was attributed to the gender distributions of the groups (e.g., the I+G group).
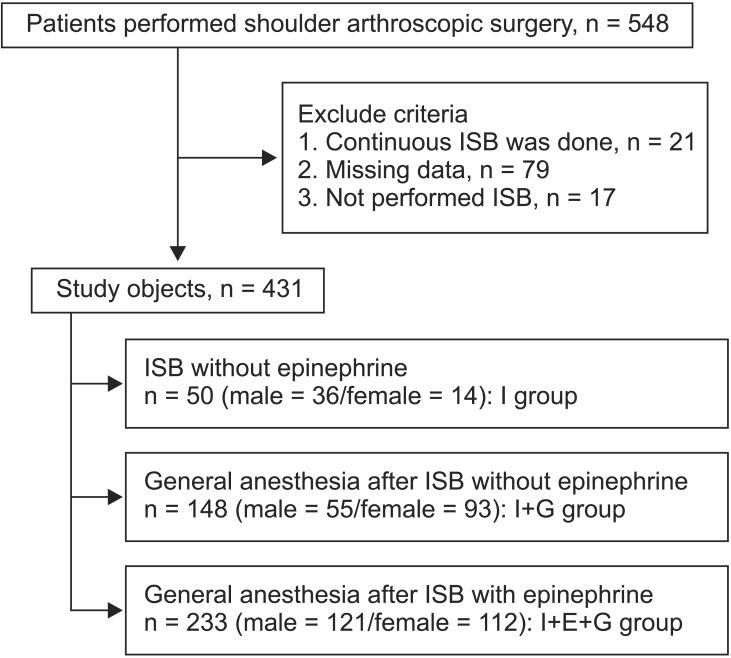 | Fig. 1Flow chart of the patients. ISB: interscalene block.
|
Table 1
Patient Demographics
|
Variable |
I+G (n = 148) |
I+E+G (n = 233) |
I (n = 50) |
P value |
|
Sex (M/F) |
55 (37.1%)/93 (62.8%) |
121 (51.9%)/112 (48.1%) |
36 (72%)/14 (28%) |
< 0.001 |
|
Age (yr) |
59 ± 10 |
59 ± 9 |
56 ± 9 |
0.064 |
|
Height (cm) |
158.2 ± 8.4 |
160.9 ± 8.7 |
163.8 ± 8.1 |
< 0.001 |
|
Weight (kg) |
62.4 ± 11.0 |
64.9 ± 13.1 |
67.4 ± 11.4 |
0.024 |
|
Hypertension |
57 (38.5%) |
75 (32.2%) |
15 (30%) |
0.365 |
|
Diabetes |
17 (11.5%) |
26 (11.2%) |
4 (8%) |
0.781 |
|
ASA (I/II/III) |
59/83/5 (39.9%/56.1%/3.4%) |
98/130/6(42.1%/55.8%/2.6%) |
29/17/4 (58%/34%/8%) |
0.344 |

Blood pressure and heart rate
We choose the I+G group as the default group.
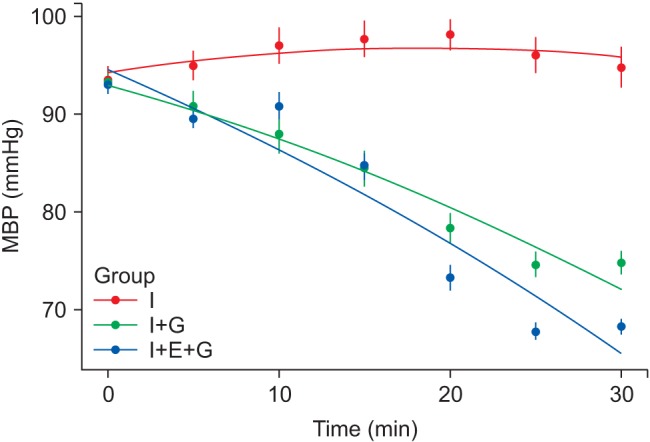
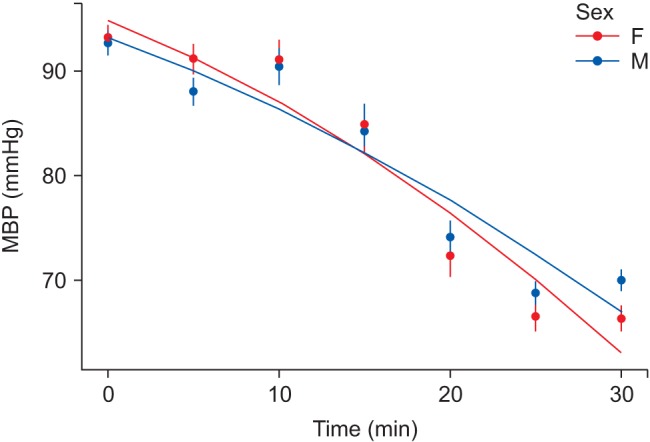
Fig. 2 shows the changes in mean MBP during the initial 30 of monitoring. First, we used linear and quadratic expressions to show interactions with time. Using ANOVA, the quadratic model was selected (chi-square 6.8041, df = 1, P value = 0.009). We created a full model that included all of the covariates (sex, age, height, weight, ASA class, group, and time) and a regressed model, and selected covariates using ANOVA. The model finally selected was:
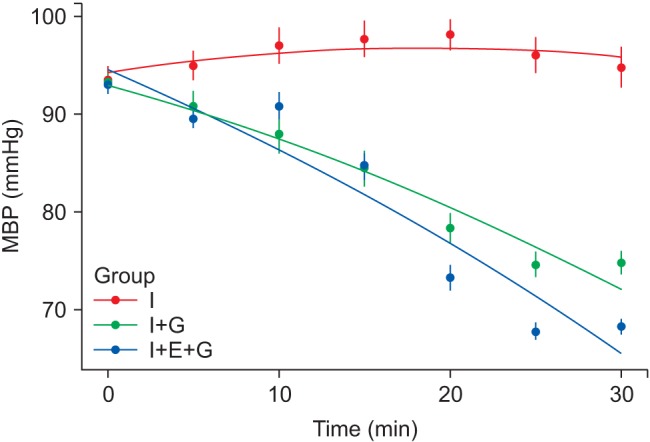 | Fig. 2Changes in mean blood pressure (MBP). Dots and vertical lines indicate mean ± SE. The curve is the fitted value. I: interscalene block without epinephrine, I+G: general anesthesia after interscalene block without epinephrine, I+E+G: general anesthesia after interscalene block with epinephrine.
|
A significant difference was observed in the change of MBP with time in the I+G group (the linear term coefficient and its standard error for the I+G group was −0.7468 ± 0.1588, P < 0.001).
The linear term coefficient differed significantly between groups I+G and I (1.2950 ± 0.3176, P < 0.001), but there was no significant difference from the I+E+G group (1.2890 ± 0.2025, P = 0.524). The quadratic term coefficient differed significantly between groups I+G and I+E+G (−0.0134 ± 0.0063, P = 0.036).
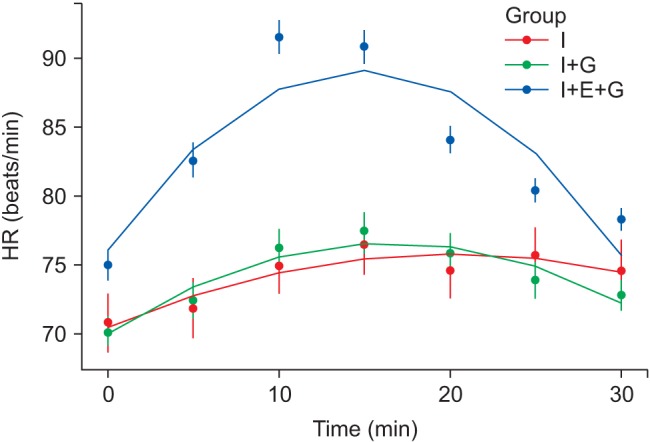
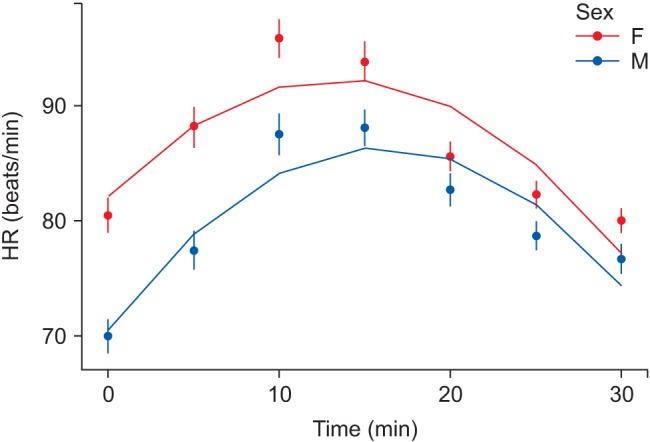
Fig. 3 shows the changes in HR. We expressed the HR as:
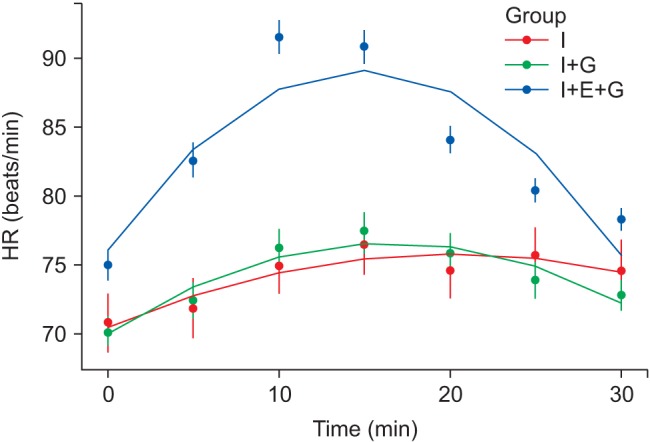 | Fig. 3Changes in heart rate (HR). Dots and vertical lines indicate the mean ± standard error. The curve is the fitted value. I: interscalene block without epinephrine, I+G: general anesthesia after interscalene block without epinephrine, I+E+G: general anesthesia after interscalene block with epinephrine.
|
In the I+G group, the linear and quadratic term coefficients were statistically significant (0.8012 ± 0.1213, P < 0.001; −0.0242 ± 0.0036, P < 0.001). The linear and quadratic term coefficients differed significantly between groups I+G and I+E+G (0.9511 ± 0.1546, P < 0.001; −0.0346 ± 0.0047, P < 0.001), but not between groups I+G and I (−0.2703 ± 0.2425, P = 0.265; 0.0110 ± 0.0074, P = 0.137).
Separate analysis of males and females
Because the male to female ratios were significantly different among the groups, we compared the values between the sexes. A nearly equal male:female ratio was observed in the I+E+G group. MBP did not differ significantly between males and females (linear term coefficient and its standard error, 0.0416 ± 0.2643, P = 0.875; quadratic term coefficient and its standard error, 0.0047 ± 0.0083, P = 0.571) (
Fig. 4). In comparison, HR differed significantly in the linear term coefficient (0.4794 ± 0.2065, P = 0.020), but not in the quadratic term coefficient (0.0061 ± 0.0063, P = 0.3312) in our model (
Fig. 5). Although females had a significantly faster HR than males within the same group, we considered the difference clinically insignificant.
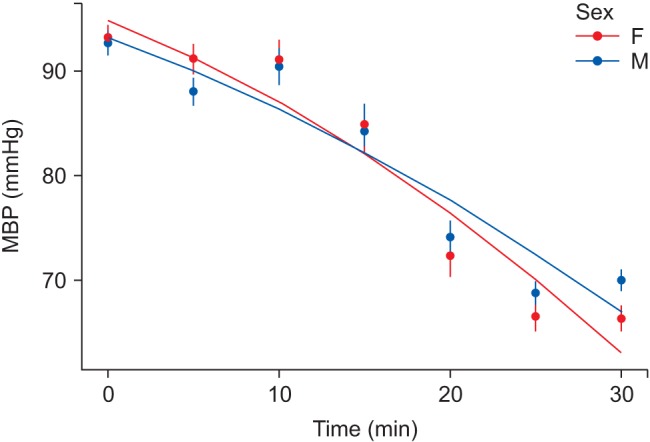 | Fig. 4Comparison of mean blood pressure (MBP) between the sexes in the general anesthesia after interscalene block with epinephrine (I+E+G) group. Dots and vertical lines indicate the mean ± standard error. The curve is the fitted value. F: female, M: male.
|
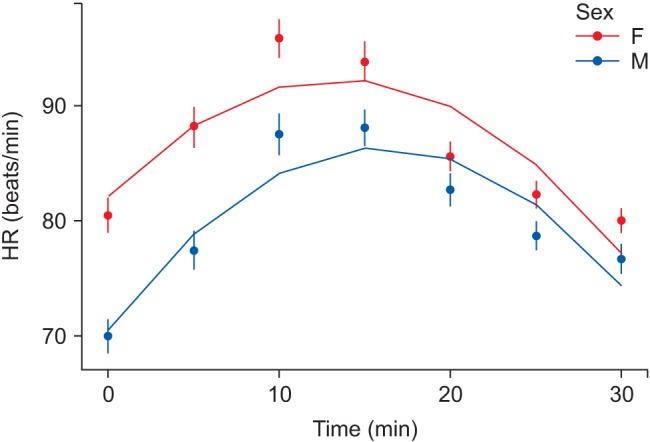 | Fig. 5Comparison of heart rate (HR) between the sexes in general anesthesia after interscalene block with epinephrine in the (I+E+G) group. Dots and vertical lines indicate the mean ± standard error. The curve is the fitted value. F: female, M: male.
|
Administration of vasoactive drugs
Ephedrine, phenylephrine, nicardipine, and labetalol were administered to maintain the targeted MBP (60 < MBP < 110 mmHg). The numbers of patients using each of the vasoactive drugs in each group are shown in
Table 2. None of the drugs showed significant differences among the groups, except nicardipine in the I group.
Table 2
Vasoactive Drugs Used during the First 30 Minutes
|
Dose |
I+G (n = 148) |
I+E+G (n = 233) |
I (n = 50) |
P value |
|
Ephedrine (mg) |
5 |
1 |
3 |
0 |
|
|
10 |
3 |
4 |
0 |
|
|
20 |
1 |
1 |
0 |
|
|
Total |
5 |
8 |
0 |
0.890 |
|
Phenylephrine (µg) |
50 |
1 |
3 |
0 |
|
|
100 |
2 |
9 |
0 |
|
|
150 |
0 |
1 |
0 |
|
|
200 |
1 |
1 |
0 |
|
|
300 |
0 |
1 |
0 |
|
|
Total |
4 |
15 |
0 |
0.742 |
|
Nicardipine (mg) |
0.5 |
0 |
0 |
3 |
|
|
1 |
0 |
1 |
2 |
|
|
Total |
0 |
1 |
5 |
< 0.001 |
|
Labetalol (mg) |
10 |
1 |
0 |
0 |
|

Go to :

Discussion
Our goal was to determine the efficacy of epinephrine used with ropivacaine for ISB. MBP tended to decrease gradually in groups I+G and I+E+G. There was a significant difference in MBP between the groups I+G and I, and between the groups I+G and I+E+G. HR was affected by epinephrine; the I+E+G group showed a significant increase in HR compared with that in the other two groups.
Many studies have investigated controlling hypotension induced by the BCP. Kwak et al. [
8] showed that the use of a sequential compression device reduces the incidence of hypotension from 64 to 28% and supports hemodynamic variables such as mean arterial pressure and stroke volume index, when patients undergoing shoulder arthroscopy are changed from the supine to the BCP. Cho et al. [
9] reported that a prophylactic bolus administration of arginine vasopressin prevents hypotension associated with BCP.
Not using general anesthesia could help prevent a drop in BP. Koh et al. [
10] found that patients in the BCP treated with regional anesthesia and sedation had almost no change in BP or cerebral desaturation events, unlike patients who received general anesthesia. Rohrbaugh et al. [
11] suggested that intraoperative or immediate postoperative stroke is rare when surgery is conducted in the BCP in conjunction with regional anesthesia, propofol sedation, and spontaneous respiration via a natural airway.
Sudden decreases in HR and BP had been reported in 13% of patients anesthetized with ISB in the BCP [
12], associated with the Bezold–Jarisch reflex (BJR). The BJR occurs when venous pooling (sitting position) and increased sympathetic tone (epinephrine) induce a low volume and hypercontractile ventricle. Then, activation of the parasympathetic and depression of the sympathetic systems occur. Epinephrine has been reported as a cause of BJR [
13]. However, Seo et al. [
14] reported that using epinephrine as an adjunct to local anesthetic does not contribute to bradycardia and hypotension episodes. In addition, 31% of epinephrine group patients received an antihypertensive drug in the study of Sia et al. [
13]. None of these three studies used general anesthesia or ultrasonography [
121314]. Therefore, an incomplete block is possible, and systemic absorption of epinephrine can be irregular. We applied ultrasonography to all patients in the present study. We expected the MBP to increase in the I+E+G group, as in a previous study [
13], but it did not. The reason may be that we added general anesthesia in the I+E+G group. General anesthesia inhibits the lower extremity muscle contraction necessary for maintaining venous return to the heart. Venous congestion caused by the BCP during shoulder surgery under general anesthesia decreases preload and promotes abnormal cardiac contractions due to hypersecretion of catecholamines [
15]. However, the HR remained significantly higher for 30 min after injecting epinephrine, unlike BP in our study.
Several reports have shown severe hypotension and bradycardia immediately after placing patients in a sitting position under general anesthesia [
216], which cannot be explained by the BJR associated with epinephrine. Rather, preventive epinephrine is thought to be helpful in these events. The BJR associated with epinephrine usually occurs 33–40 min after placing the patient in the sitting position and 59–64 min after ISB [
1315].
Fig. 2 shows that MBP decreased slightly after the I+E+G group patients were seated; thus, comparing the results after 30 min was important. However, various biases occur once the operation begins. The beginning of the operation may cause fluctuations in BP, and surgeons sometimes require induced hypotension. Cold fluid flowing into the joint space may also have an effect. As it usually takes about 20 min to prepare for surgery, the hemodynamic data during the first 30 min after inducing anesthesia were collected in this study.
Our study had several limitations. First, this was a retrospective study. Second, we only collected 30 min of data after the initial check. Third, there were differences in the sample size among groups; the I+E+G group had 234 cases, but the I group had only 50 cases. More females were included in the I+G group and more males were included in the I group, because females tended to consent to general anesthesia for surgery. Thus, the I+G and I groups did not have a balanced patient gender ratio. There was also a significant difference in HR between males and females.
The HR differed among the groups at baseline. The vital signs were recorded automatically but there was a time gap to upload the data; thus, there could be some cases in which the recorded data were affected by the epinephrine. This may explain why the initial HR in the I+E+G group tended to higher than that in the I+G group.
In summary, ISB with an epinephrine mixture did not prevent the hypotension caused by the BCP after general anesthesia. The HR increased only in response to the epinephrine mixture. Hypotension after placing the patient in the BCP was not present only in cases of regional anesthesia without general anesthesia. A well-planned prospective study is required to compare the hemodynamic changes related to BCP.
Go to :





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download