Abstract
Anterior cervical osteophytes are commonly found in elderly patients, but rarely produce symptoms. When symptoms occur, they can range from mild symptoms of dysphagia, dysphonia, and foreign body sensation to severe symptoms of airway obstruction due to compression of the pharynx or larynx. We report the case of a 59-year-old man who underwent brain tumor surgery, and developed post-operative respiratory difficulty due to progressive pharyngo-laryngeal edema, requiring urgent endotracheal intubation, secondary to the presence of a previously asymptomatic anterior cervical osteophyte. It is paramount to recognize that asymptomatic anterior cervical osteophytes are a potential cause of life-threatening post-operative respiratory complications that can rapidly progress to life-threatening airway obstruction after surgeries in the prone position, especially in elderly patients.
Anterior cervical osteophytes are found in 20–30% of the general population [1], but are more frequently observed in elderly patients. They are associated with the conditions such as senile degenerative disease, diffuse idiopathic skeletal hyperostosis (DISH), cervical spondylitis, infectious skeletal spondylitis, and ankylosing spondylitis [2], and are diagnosed on the basis of radiologic findings. Most osteophytes are asymptomatic, but can produce symptoms ranging from dysphagia, dysphonia, and foreign body sensation to severe respiratory difficulty due to inflammation and edema arising from mechanical compression [23]. Dysphagia appears to be the most common presentation, caused by mechanical obstruction of pharyngo-esophagus by anterior cervical osteophyte [4]. Clinically manifested airway compression by anterior cervical osteophyte is very rare [5].
Generally, the edema of laryngeal structure in postoperative period is one of the most severe complications, because it can cause progressive aggravating respiratory difficulty with significant morbidity and mortality [6]. Multiple factors may predispose to the development of airway edema in a previously normal airway during postoperative period. Here we present a case report of a postoperative upper airway obstruction secondary to a previously asymptomatic anterior cervical osteophyte after undergoing brain tumor surgery in a flexed cervical prone position. We discuss preoperative evaluation, intraoperative management, and extubation strategy.
A 59-year-old, 166 cm, 69 kg man was admitted to hospital via emergency room with the chief complaint of dysarthria and bilateral lower extremity weakness during 1 month. Brain computed tomography (CT) findings were consistent with hemangioblastoma with a cystic mass in the right cerebellum and the patient was scheduled to undergo a craniectomy and tumor removal. Patient's medical history included hypertension and diabetes mellitus (DM). Preoperative laboratory tests, including arterial blood gas analysis (ABGA: pH 7.428, PaCO2, 33.7 mmHg, PaO2 79.3 mmHg, BE −0.7 mmol/L, SaO2 96.1% on room air), chest radiography, and pulmonary function tests, were unremarkable. Pre-anesthetic airway examination revealed Mallampati class III airway with a short neck. Physical examination of the neck was unremarkable.
After premedication with glycopyrrolate 0.2 mg intramuscular 1 hour before anesthesia, the patient was monitored with non-invasive arterial pressure, electrocardiograph, pulse oximetry, and bispectral index (BIS). General anesthesia was induced with an effective-site concentration of propofol 5 µg/ml, remifentanil 5 ng/ml using target controlled infusion (TCI; Orchestra Base Primea, Fresenius Vial, Brézins, France), and rocuronium 0.9 mg/kg intravenously for tracheal intubation. Preoperative preparation and anesthetic induction took place in the supine position. Tracheal intubation was performed with an 8.0-mm internal diameter (ID) reinforced cuffed endotracheal tube (ETT) by a single attempt. Since we anticipated a difficult intubation, we used a video laryngoscopic approach (McGrath® MAC, Covidien, Mansfield, MA, USA). The cuff was inflated with air to a volume of 5 ml. Anesthesia was maintained around BIS 40 with effect-site TCI of propofol 3–5 µg/ml and remifentanil 5–15 ng/ml. Hemodynamics remained stable during tracheal intubation. After induction, we inserted the invasive arterial line in the right radial artery and the central venous line in the right subclavian vein as access for more continuous monitoring. The patient was moved to the prone position with neck flexion maintained by using a Mayfield fixation device for surgery. At the end of surgery, the patient was repositioned to the supine position and the trachea was extubated after adequate antagonization of neuromuscular blockade and confirming the air leak around endotracheal tube. After extubation, he was alert with normal spontaneous respiration and stable hemodynamics and was thus safely transferred to intensive care unit (ICU) on with supplemental O2 delivered by face mask at 6 L/min. After the patient's arrival to ICU, we checked an ABGA (pH 7.409, PaCO2 31.1 mmHg, PaO2 146.6 mmHg, BE −3.3 mmol/L, SaO2 99.3%) while he was receiving supplemental O2 via face mask at 5 L/min. Total operating time was 3 hours and 55 minutes and total anesthesia time was 5 hours and 35 minutes. Total infusion volume during anesthesia included; 500 ml of normal saline, 950 ml of a plasma solution, and 200 ml of 20% mannitol. Total output during anesthesia included a blood loss of 500 ml with 1,250 ml of urine output. Total anesthetic drugs infused were 3,000 mg of 2% propofol, 4 mg of remifentanil, and 105 mg of rocuronium.
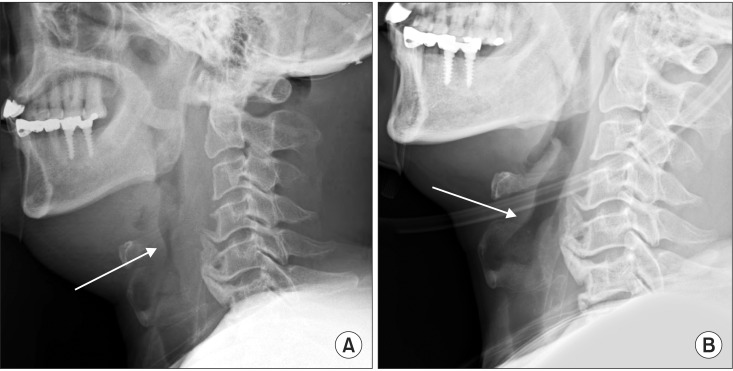
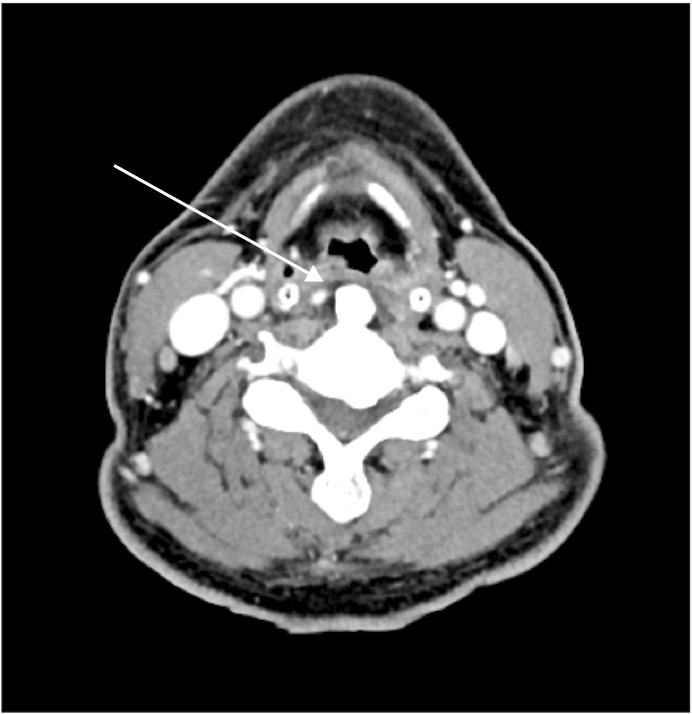
The patient remained stable until postoperative hour 4 when he developed respiratory stridor accompanied by increased swelling of anterior neck which progressed to respiratory difficulty and impending respiratory failure. However, the monitor measured a SpO2 of 100% and despite our best efforts (including an evaluation to rule out causes such as deep neck infection), we could not identify the cause of his postoperative respiratory difficulty. Despite the application of supplemental O2 via face mask at 10 L/min, his SpO2 decreased to 90% at postoperative hour 6. We did not check an ABGA at that time. At this time, we obtained a plain radiograph of the neck that showed severe swelling of anterior neck and pre-vertebral tissues with severe narrowing of the airway (Fig. 1A). We also obtained a cervical CT that revealed asymmetrical edematous thickening on the left epiglottic and hypopharyngeal wall with a partial airway obstruction; a fluid collection in multiple deep neck spaces, bilateral cheek, and prevertebral space; large protruding anterior osteophyte at C4-C7 level (Fig. 2).
At postoperative hour 14, owing to a markedly edematous pharyngo-laryngeal structure, the trachea was successfully intubated after 3 attempts with 6.5-mm ID polyvinylchloride ETT. The ETT was placed to maintain a patent airway, while the ventilator was set to allow for spontaneous respiratory effort with supplemental O2 at 5 L/min. After endotracheal intubation, ABGA returned to normal range (pH 7.397 PaCO2 32.4 mmHg PaO2 97.4 mmHg BE −3.3 mmol/L SaO2 99.3%) with supplemental O2 5 L/min during spontaneous ventilation. Our patient underwent the conservative treatment with antibiotics, anti-inflammatory agents, steroids, and muscle relaxants instead of surgical removal of the osteophyte. After 6 days of tracheal intubation, patient's respiratory difficulty resolved and swelling of the pharyngo-laryngeal area improved as seen on radiologic finding (Fig. 1B), and then endotracheal tube in patient was extubated. On the 15th postoperative day, the patient was discharged without neurologic sequelae or respiratory difficulty.
Although there are the case reports that describe dysphagia and respiratory difficulty secondary to an anterior cervical osteophyte, there have been no reports that describe progressing respiratory difficulty by asymptomatic anterior cervical osteophyte that required emergent endotracheal intubation postoperatively. Because our patient had no history of respiratory problems prior to surgery, we had a difficulty for determining the cause of his postoperative respiratory difficulty.
Although the most common causes of postoperative respiratory difficulty after brain surgery include hematoma, prolonged intubation, vocal cord paralysis by nerve injury, persistent cerebrospinal fluid leak, and allergy- or immune-mediated edema [7], our patient had no clinical findings consistent with any of the above mentioned causes. In our case, his respiratory difficulty was secondary to the presence of an asymptomatic anterior cervical osteophyte and the surgical position of patient. The compression of posterior pharyngeal wall and upper airway by anterior cervical osteophyte, led to the edema and subsequent partial obstruction or distortion of laryngeal inlet and consequent dyspnea. The extensive neck anterior flexion under prone position during surgery, resulted indirect extrinsic compression and reactive intrinsic inflammation, and also disrupted the venous, lymphatic flow in the anterior neck that resulted in airway edema and airway obstruction.
In our case, the formation of anterior cervical osteophyte was suggested by DISH, which was diagnosed by the flowing ossification along the anterolateral aspect of spine (at least 4 contiguous vertebral bony bridges without intervertebral degenerative changes) with the preservation of intervertebral disc height [8] (Figs. 1 and 2). In case of anterior cervical osteophyte by DISH, several layers of incomplete ossification may exist in soft tissue and induce the sudden onset of symptoms by intrinsic inflammation anterior to these layers [9]. The etiology of DISH is unknown, but it is associated with obesity and type 2 DM that was the co-morbidity in our patient. Chronic metabolic derangement induces insulin-like growth factor 1 and increases levels of interleukins 1 and 2, which promotes proliferation of osteoblasts and bone deposition on spine bony bridges [10]. In Verlaan et al.'s review article [11], with the global increase of metabolic disorder and prolonged life expectancy, there is a tendency for the increase in the number of patients with anterior cervical osteophytes. However, many anesthesiologists and surgeons are not familiar with the clinical or radiologic findings of anterior cervical osteophyte. Initially, an anterior cervical osteophyte is tolerated well in most patients due to the slow growth of osteophyte. However, when a patient undergoes major events such as surgery in our patient's case, and there is a decrease in compensatory reserves. The minor changes in well-tolerated mechanical obstruction around trachea or larynx, can lead to sudden acute onset of airway obstruction [11]. In addition, in the presence of distortion, similar to our case, the development of respiratory discomfort not only occurs faster, but can be more exaggerated. But this relationship between respiratory difficulty and anterior cervical osteophyte is often overlooked during perioperative anesthetic management.
Location and size of anterior cervical osteophyte manifest variable signs and symptoms in patient. The partial airway obstruction or vocal cord immobility by inflammation of anterior cervical osteophytes at the level of C4-C5 manifests as dyspnea, dysphonia, and stridor [912]. Generally stridor is associated with acute respiratory difficulty, urgent intubation with mechanical ventilation is required or has to be maintained postoperatively for keeping airway patency from pharyngo-laryngeal edema [13]. In our patient, we diagnosed the cause of respiratory difficulty by the findings in the plain radiograph of the lateral neck and cervical CT findings, and subsequently performed tracheal intubation.
Our patient also underwent conservative treatment with antibiotics, anti-inflammatory agents, steroids, and muscle relaxants instead of surgical removal of the osteophyte. Surgical excision of osteophytes is considered if conservative support is result in failure [1], but it is important to note that even after surgical resection, the radiologic reappearance of osteophyte formation in an average rate of 1 mm/year has been reported [14]. Generally, anterior cervical osteophytes are common, and the thorough preoperative evaluation for any existing anterior cervical osteophytes may be needed. This should especially be stressed in elderly patients planning to undergo longstanding surgery with neck flexion in the prone position.
As we have illustrated, the presence of an asymptomatic anterior cervical osteophyte should be included in the differential diagnosis when determining causes for postoperative rapidly progressing respiratory difficulty, especially in the elderly patients.
References
1. Papadopoulos SM, Chen JC, Feldenzer JA, Bucci MN, McGillicuddy JE. Anterior cervical osteophytes as a cause of progressive dysphagia. Acta Neurochir (Wien). 1989; 101:63–65. PMID: 2603770.

2. Matan AJ, Hsu J, Fredrickson BA. Management of respiratory compromise caused by cervical osteophytes: a case report and review of the literature. Spine J. 2002; 2:456–459. PMID: 14589272.
3. Seo JW, Park JW, Jang JC, Kim JW, Lee YG, Kim YT, et al. Anterior cervical osteophytes causing Dysphagia and paradoxical vocal cord motion leading to dyspnea and dysphonia. Ann Rehabil Med. 2013; 37:717–720. PMID: 24236261.

4. Varsak YK, Eryilmaz MA, Arbağ H. Dysphagia and airway obstruction due to large cervical osteophyte in a patient with ankylosing spondylitis. J Craniofac Surg. 2014; 25:1402–1403. PMID: 24905946.

5. Demuynck K, Van Calenbergh F, Goffin J, Verschakelen J, Demedts M, Van de Woestijne K. Upper airway obstruction caused by a cervical osteophyte. Chest. 1995; 108:283–284. PMID: 7606974.

6. Ho LI, Harn HJ, Lien TC, Hu PY, Wang JH. Postextubation laryngeal edema in adults. Risk factor evaluation and prevention by hydrocortisone. Intensive Care Med. 1996; 22:933–936. PMID: 8905428.

7. Tagawa T, Akeda K, Asanuma Y, Miyabe M, Arisaka H, Furuya M, et al. Upper airway obstruction associated with flexed cervical position after posterior occipitocervical fusion. J Anesth. 2011; 25:120–122. PMID: 21188427.

8. Resnick D, Niwayama G. Radiographic and pathologic features of spinal involvement in diffuse idiopathic skeletal hyperostosis (DISH). Radiology. 1976; 119:559–568. PMID: 935390.

9. Marks B, Schober E, Swoboda H. Diffuse idiopathic skeletal hyperostosis causing obstructing laryngeal edema. Eur Arch Otorhinolaryngol. 1998; 255:256–258. PMID: 9638468.

10. Sarzi-Puttini P, Atzeni F. New developments in our understanding of DISH (diffuse idiopathic skeletal hyperostosis). Curr Opin Rheumatol. 2004; 16:287–292. PMID: 15103260.

11. Verlaan JJ, Boswijk PF, de Ru JA, Dhert WJ, Oner FC. Diffuse idiopathic skeletal hyperostosis of the cervical spine: an underestimated cause of dysphagia and airway obstruction. Spine J. 2011; 11:1058–1067. PMID: 22015236.

12. Giger R, Dulguerov P, Payer M. Anterior cervical osteophytes causing dysphagia and dyspnea: an uncommon entity revisited. Dysphagia. 2006; 21:259–263. PMID: 17216390.

13. Kapetanakis S, Vasileiadis I, Papanas N, Goulimari R, Maltezos E. Can a giant cervical osteophyte cause dysphagia and airway obstruction? A case report. Wien Klin Wochenschr. 2011; 123:291–293. PMID: 21484285.

14. Miyamoto K, Sugiyama S, Hosoe H, Iinuma N, Suzuki Y, Shimizu K. Postsurgical recurrence of osteophytes causing dysphagia in patients with diffuse idiopathic skeletal hyperostosis. Eur Spine J. 2009; 18:1652–1658. PMID: 19714374.

Fig. 1
Lateral neck radiograph (A) at postoperative 6 hours that demonstrated swelling of pre-vertebral tissues and narrowing of the airway (arrow) with larger anterior osteophyte at C4-C7 level, (B) at postoperative 7 days that demonstrated relieved swelling of pre-vertebral tissues and narrowing of the airway (arrow) with anterior osteophyte at C4-C7 level.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download