Abstract
Vagally mediated atrioventricular (AV) block is a condition which a paroxysmal AV block occurs with the slowing of the sinus rate. Owing to its unpredictability and benign nature, it often goes unrecognized in clinical practice. We present the case of a 49-year-old man who suddenly lost consciousness when he assumed a prone position for hemorrohoidectomy under spinal anesthesia; continuous electrocardiographic recording revealed AV block with ventricular asystole. He was completely recovered after returning to a supine position. This case calls our attention to fatal manifestation of vagally mediated AV block leading to syncope.
Vagally mediated atrioventricular (AV) block is any degree AV block accompanied by the slowing of the sinus rate without affecting the His-Purkinje system [1]. Vagally mediated AV block is typically paroxysmal and is generally present as an asymptomatic event in most cases without ventricular asystole, if present, rarely exceeds 3 s [234]. However, as presented in this case, the vagal effect on AV conduction system can be severe enough to cause prolonged ventricular asystole and, subsequently, syncope. We will discuss the predisposing factors and implication of vagally mediated AV block relevant to this case.
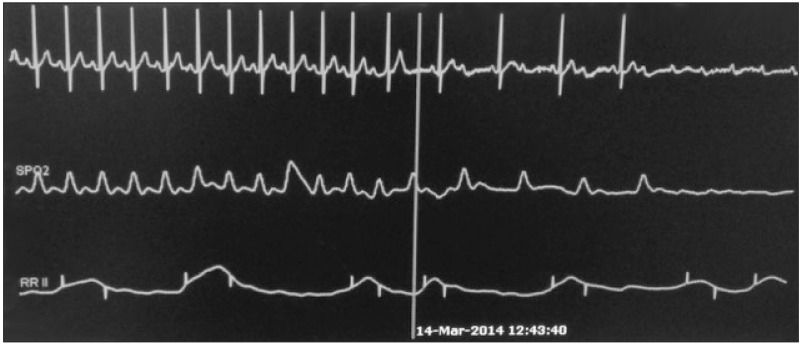
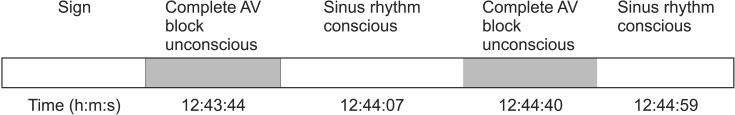
A 49-year-old man with a body mass index of 30 (height 165.4 cm, weight 81.7 kg and abdominal circumference 108.5 cm) was scheduled to have a hemorrhoidectomy under spinal anesthesia. He was not taking any medication and his medical history was unremarkable. The preoperative laboratory examinations were normal; sinus rhythm without conduction abnormalities on 12-lead electrocardiogram (ECG). The patient arrived operating room without premedication. Upon arrival, standard monitoring devices were applied; baseline heart rate (HR) was 81 beats per minute (bpm) with normal sinus rhythm and blood pressure (BP) was 134/72 mmHg. A spinal anesthesia was carried out using 8 mg of bupivacaine at sitting position. Then, he lay prone 3 minutes after bupivacaine injection. The block level, immediately after a prone position, was L3 checked using an alcohol swab with stable vital sign (BP 102/63 mmHg, HR 92 bpm). About 2 minutes later, the patient complained of nausea and soon after lost consciousness. The ECG monitoring showed complete AV block with ventricular asystole (Video 1). While reaching for a stretch cart to move the patient to supine position and preparing atropine injection, a sinus rhythm returned and the patient regained consciousness. But soon another episode of AV block developed and the patient became unconscious again (Video 1). This time he was immediately transferred to a stretch cart for a supine position and simultaneously 0.5 mg atropine was injected. Shortly after, both patient's consciousness and sinus rhythm returned (BP 95/60 mmHg, HR 81 bpm, block level L3). The sequence of events was summarized in Fig. 1. He did not recall syncope events and did not seem to be nervous or restless through out the anesthesia. The operation was performed under lithotomy position without any further development of AV block. On questioning, he reported that he had been found unconscious at a local steam sauna with bruise on his forehead a few years ago. After two days, he was discharged without any complication.
We believe that the patient in this case suffered syncope as a result of vagally mediated AV block with prolonged ventricular asystole. A variety of mechanisms can cause vasovagal response [5]. Sudden decrease of venous return is a well-known risk factor of a severe vagal activation [6]. Typical cases of vagally mediated AV block can be discovered in any conditions which create sudden surge of parasympathetic outflow to heart, such as carotid sinus massage, tilt-induced syncope, vasovagal syncope, and emotional distress [1].
An unopposed parasympathetic hyperactivity is the main pathophysiology responsible for both vasovagal syncope and AV block. A vagal surge can cause syncope and AV block simultaneously in some patients but not always. Indeed, AV block during tilt-induced syncope was rarely reproduced and Brignole et al. [7] reported that isolated depression of sinus node function was four times more common than AV block during a positive tilt test. Also, an artificial pacing does not prevent vasovagal syncope in patients with bradycardia [8]. Although we frequently encounter vagally mediated second- or third-degree AV block as an asymptomatic in clinical practice, the resultant sustained ventricular asystole can lead to a loss of consciousness as a result of profound decrease in cerebral blood flow. In this case, the stored telemetry showed heterogeneous presentation of AV block during the first episode of syncope (Video 1). We suggest that the vagal overactivity in our patient is related to a reduced venous return due to prone positioning. Instead of atropine, we believe the restoration of AV conduction was a result of the change of the patient's position because of the drug's inability to reach central circulation. Additionally, patient's previous syncope episode could be attributed to a vasovagal response considering circumstances where peripheral vasodilation in hot environment could cause central blood volume depletion. We cannot confirm that vasovagal AV block was also present at that time because vasovagal syncope can occur without heart symptom.
Prone position is often required for hemorrhoidectomy, the second most common operation performed in 2013 [9]. The physiologic changes in prone position have been well described in literatures and the most consistent of which is a decrease in cardiac index [10]. In a prone position, a hypotension in the obstruction of the inferior vena cava (IVC) is influenced by the degree of abdominal compression. Since our patient was centrally obese, he is more susceptible to venous obstruction from the high abdominal pressure. The direct compression of the abdomen could have been reduced if parallel thoracic rolls were placed and the patient correctly positioned on them.
Peripheral venous pooling resulted from spinal anesthesia could be attributed to a sudden drop in central venous volume in this case. Geffin and Shapiro [11] reported 13 cases of severe bradycardia or asystole from approximately 4000 regional anesthesia. They could not find any common risk factor from patients' profile and concluded that a reflex, possibly associated low cardiac filling pressure could be the cause of these clinical feature. Although the block level was relatively low to produce a significant effect alone in our case, when it was superimposed on IVC obstruction, it could be a significant hazard.
Vagally mediated AV block is generally considered as benign because there is no anatomical abnormality in the AV conduction system. If an asymptomatic vagally mediated AV block is encountered, these patients should only be followed up in order to monitor the possible appearance of symptoms [1]. However, it is important to understand that life-threatening syncope due to prolonged ventricular asystole may be developed in vagally mediated AV block in a small percentage of patients. Jang et al. [12] reported a case of vasovagal cardiac arrest during spinal anesthesia for cesarean section. The symptoms of vasovagal reflex were far more serious than ours and the patient was successfully resuscitated with chest compression, mask ventilation and epinephrine injection.
If a patient experiences any vasovagal symptom such as nausea, abdominal discomfort and diaphoresis, adequate venous return should be restored promptly with Trendelenburg or leg elevation and relieve of IVC compression [13]. Spontaneous recovery from ventricular standstill may occur with restoration of sufficient central venous volume [14]. Intravenous fluid must be considered if there is hypovolemic evidence and pre-existing hypovolemic should be corrected before establishment of regional anesthesia. Kinsella and Tuckey [13] recommended ephedrine as a single agent for profound bradycardia and asystole during regional anesthesia, considering the lack of vasoconstrictor effect of atropine. However, for persistent cardiac arrest, external cardiac massage with epinephrine injection must be started early to ensure circulation of resuscitation drugs and perfusion of vital organs [15].
This case illustrates a serious consequence of vagally mediated AV block in a prone positioned patient under spinal anesthesia. It seems likely that this phenomenon was chiefly induced by a decrease in venous return, secondary to the postural change from the sitting to the prone. It should be stressed again that the proper patient positioning and constant monitoring should not be overlooked only because patients are awake and under regional anesthesia.
References
1. Alboni P, Holz A, Brignole M. Vagally mediated atrioventricular block: pathophysiology and diagnosis. Heart. 2013; 99:904–908. PMID: 23286970.

2. Moore PK, Lee JK, Garcia JA, Krantz MJ. A case of swallow syncope. Tex Heart Inst J. 2013; 40:606–607. PMID: 24391337.
3. Mendoza IJ, Castellanos A, Lopera G, Moleiro F, Mitrani RD, Myerburg RJ. Spontaneous paroxysmal atrioventricular block in patients with positive tilt tests and negative electrophysiologic studies. Am J Cardiol. 2000; 85:893–896. A9PMID: 10758936.
4. Moya A, Brignole M, Menozzi C, Garcia-Civera R, Tognarini S, Mont L, et al. Mechanism of syncope in patients with isolated syncope andin patients with tilt-positive syncope. Circulation. 2001; 104:1261–1267. PMID: 11551877.
5. Grubb BP. Clinical practice. Neurocardiogenic syncope. N Engl J Med. 2005; 352:1004–1010. PMID: 15758011.
6. Kaufmann H, Bhattacharya K. Diagnosis and treatment of neurally mediated syncope. Neurologist. 2002; 8:175–185. PMID: 12803689.

7. Brignole M, Gaggioli G, Menozzi C, Del Rosso A, Costa S, Bartoletti A, et al. Clinical features of adenosine sensitive syncope and tilt induced vasovagal syncope. Heart. 2000; 83:24–28. PMID: 10618330.

8. Benditt DG, Petersen M, Lurie KG, Grubb BP, Sutton R. Cardiac pacing for prevention of recurrent vasovagal syncope. Ann Intern Med. 1995; 122:204–209. PMID: 7810939.

9. Korea national health insurance service. Major surgery statistical yearbook 2013. 2014. 3. retrieved in 2015/Jul. 2nd. Available from http://stat.kosis.kr/statHtml_host/statHtml.do?orgId=350&tblId=DT_35004_A09&dbUser=NSI_IN_350.
10. Edgcombe H, Carter K, Yarrow S. Anaesthesia in the prone position. Br J Anaesth. 2008; 100:165–183. PMID: 18211991.

11. Geffin B, Shapiro L. Sinus bradycardia and asystole during spinal and epidural anesthesia: a report of 13 cases. J Clin Anesth. 1998; 10:278–285. PMID: 9667342.

12. Jang YE, Do SH, Song IA. Vasovagal cardiac arrest during spinal anesthesia for Cesarean section -A case report-. Korean J Anesthesiol. 2013; 64:77–81. PMID: 23372892.

13. Kinsella SM, Tuckey JP. Perioperative bradycardia and asystole: relationship to vasovagal syncope and the Bezold-Jarisch reflex. Br J Anaesth. 2001; 86:859–868. PMID: 11573596.

14. McConachie I. Vasovagal asystole during spinal anaesthesia. Anaesthesia. 1991; 46:281–282. PMID: 2024746.

15. Caplan RA, Ward RJ, Posner K, Cheney FW. Unexpected cardiac arrest during spinal anesthesia: a closed claims analysis of predisposing factors. Anesthesiology. 1988; 68:5–11. PMID: 3337390.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download