Abstract
Proteus syndrome (PS) is a rare congenital hamartomatous disorder with multisystem involvement. PS shows highly clinical variability due to overgrowth of the affected areas, and several features can make anesthetic management challenging. Little is known about the airway problem associated with anesthesia in PS patients. An 11-year-old girl with PS was scheduled for ear surgery under general anesthesia. She had features complicating intubation including facial asymmetry and disproportion, abnormal teeth, limitation of neck movement due to torticollis, and thoracolumbar scoliosis. This study reports on a case of deformed airway of a PS patient under fiberoptic bronchoscopy.
Proteus syndrome (PS) is a rare complex harmartomatous disorder. PS is characterized by mosaic distribution of lesion, postnatal asymmetric overgrowth, and hyperplasia of multiple tissues including bone, connective tissues, fat, central nervous system, spleen, thymus, colon, and other tissues [1]. Therefore clinical findings of PS are various and several features including difficult airway, cystic lung disease, and pulmonary embolism can make anesthetic management challenging.
PS was first named by Wiedemann in 1983; only about 250 cases have been reported in literature [2], reports regarding anesthetic consideration of PS with difficult airway are limited, and no study has reported on airway of a patient with PS. We report on a case of PS and view of the airway in an 11-year-old girl, who was scheduled for ear surgery with unusual difficult airway necessitating fiberoptic bronchoscopy (FOB) for intubation.
An 11-year-old girl diagnosed as having PS with features of hemihypertrophy of the right side, scoliosis, macrodactyly accompanied by exostoses in digits and hands, subcutaneous tumors, and connective tissue nevi was scheduled for removal of a mass of the external auditory canal and mastoidectomy with tympanoplasty on the right side (Fig. 1). She had previously undergone tonsillectomy and adenoidectomy under general anesthesia with no events at the age of 2.
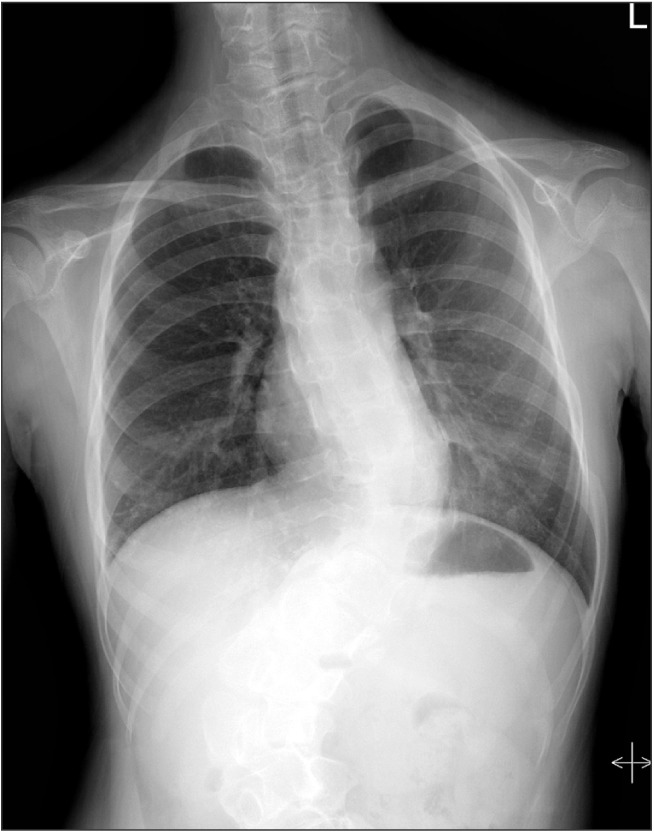
In preoperative assessment, she had facial and skull asymmetry, hypoplastic and carious teeth, a degree of mandibular prognathism and mild limitation of neck movement due to torticolis. Chest X-ray showed thoracolumbar scoliosis, but there was no deviation or stenosis of the trachea and no active lung lesion (Fig. 2). She presented good mouth opening and belonged to Mallampati class 2. However, computed tomography (CT) showed nasopharyngeal mucosal hypertrophy with adenoid vegetation and a deviated nasal septum to the right side (Fig. 3H). Therefore, flexible FOB was prepared for use when tracheal intubation was difficult or failed using a laryngoscope. Laboratory results were within normal ranges.
Her height was 155 cm, weight was 46.8 kg, blood pressure, heart rate, and oxygen saturation were 105/60 mmHg, 105 beats/min, and 99%, respectively. Glycopyrrolate 0.2 mg was administered for premedication. General anesthesia was induced with 200 mg of thiopental, 30 mg of rocuronium and continuous infusion of remifentanil. Observation of the larynx by direct laryngoscopy was unsuccessful despite complete muscle relaxation induced by rocuronium administered after confirming mask ventilation was not difficult. Cormack and Lehane (CL) grade obtained by laryngoscope was 3. Torticollis and restricted joint mobility added to difficulties. Prepared FOB was used immediately. A 6.0-mm-internal-diameter reinforced endotracheal tube was inserted orally into her trachea using FOB and fixed at the 21 cm mark over the right side of her lips after adequate positioning of the tube was confirmed by FOB. The view of FOB showed multiple polyp-like masses in the supraglottic region and her epiglottis was enlarged. The surface of the tracheal wall was rugged as there were a number of small nodules (Fig. 3). Despite the rugged wall, a 6.0-mm-internal-diameter tube was inserted smoothly. Anesthesia was maintained with sevoflurane (inspired 2.0 vol%) with a mixture of air/O2, continuous IV infusion of remifentanil. The surgery lasted for 5 hours under general anesthesia and she was sent to the recovery room after extubation with no problem. There were no anesthetic complications or problems in the recovery room and she was sent to the general ward.
PS is a rare congenital disorder with estimated incidence of less than 1 case per 1 million population. It was first named by Wiedemann et al. [2] in 1983 after the Greek sea god Proteus who had the ability to transform himself.
Clinical features of PS are highly variable and as follows: hemihypertrophy, often one whole side of body, partial bilateral gigantism of hands and feet, thickened skin on palms and soles, pigmented nevi, mesodermal tumors, macrocephaly with cranial hyperostosis, cystic lung disease, venous varicosities, anomalous teeth, scoliosis, elongated neck, vertebral enlargement, dysplastic vertebrae, hemivertebrae, and spondylomegaly [34].
Some of these deformities can cause serious perioperative complications including difficult intubation, pulmonary embolisms, thromboembolism, and pulmonary cystiform anomalies [5]. Deformities such as disproportional overgrowth of craniofascial bones, macrocephaly with cranial hyperostosis, fixed torticollis, hemihypertrophy of the cervical spine with restricted joint mobility, scoliosis, enlarged epiglottis, and macroglossia can make airway management challenging. Pennant reported on intubation using FOB for fixed torticollis, cervical deformity, and enlarged epiglottis [3]. Pradhan et al. [6] and Sinha et al. [7] reported on intubation using a McCoy levering laryngoscope for enlarged epiglottis. Cekmen et al. [8] reported on a 2.5-year boy who underwent general anesthesia using LMA without complication. In our case, difficult intubation was anticipated because the patient had facial asymmetry and disproportion, abnormal teeth, limitation of neck movement due to torticollis, and suboptimal positioning due to thoracolumbar scoliosis (Figs. 1 and 2). Laryngoscopy performed using a Macintosh blade did not show the laryngeal view and CL grade was 3. Tracheal intubation was performed with FOB. Multiple polyp-like masses and enlarged epiglottis were found in the supraglottic region. The surface of the tracheal wall was rugged with a number of small nodules (Fig. 3). Enlarged epiglottis or torticollis was previously reported as a cause of difficult intubation [367]. In addition to these factors, we found multiple masses in the supraglottic region and a rugged surface of the tracheal wall. These supraglottic mass were presumed to be lingual tonsillar hypertrophy and palatine tonsillar hypertrophy. Although there is no report of difficult intubation due to tonsillar hypertrophy in PS, a huge tonsillar mass causing dysphagia was reported as a manifestation of PS [9]. No case of PS involving a rugged surface or protruded masses of trachea has been reported, therefore it is not certain whether this feature is common or not. However, given hyperplasia of multiple tissue of PS, this feature appears to be associated with PS.
PS, which shows highly variable manifestations and a progressive pattern with age, have fatal complications associated with airway management. Overgrowth and asymmetry appear at birth in 17.5%, various manifestations of PS appear mainly after birth and develop at a various rate resulting in deformity in later childhood [4]. In our case, although she had mild PS manifestations at the age of 2 she underwent tonsillectomy and adenoidectomy under general anesthesia without event, she showed difficult airway necessitating FOB at this time of surgery.
We performed a preoperative airway evaluation with chest X-ray, temporal bone CT, and mallampati classification. Difficult intubation was expected, but was performed successfully using FOB. However, more evaluation was required, including neck CT, preoperative indirect laryngoscopic examination, and more preparation including videolaryngoscope, awake intubation, and trachoesotomy. Awake intubation using FOB is commonly recommended for patients with difficult airways. This method might be suitable in most cooperative patients [10]. In this case, we could not consider awake intubation due to lack of cooperation and less experience of awake intubation in children.
However, some reports have shown safe and successful awake fiberoptic intubation in pediatrics using adequate sedation and airway anesthesia. Xue et al. [11] suggested that rapport with children, adequate airway anesthesia, adequate sedation with midazolam, and opioid are important for awake intubation for pediatric patients. Accordingly, some practitioners suggested guidelines for use in performance of a fiberoptic intubation using propofol, fentanyl, and lidocaine spray while maintaining spontaneous breathing in pediatric patients [12]. These methods might be better options for safer anesthesia in this case. In conclusion, evaluation of the airway is required in PS patients while planning anesthesia for a patient with PS. Preoperative indirect laryngoscopic examination and tracheal intubation using FOB including awake intubation would be helpful in performance of safe anesthesia. In the aspect of anesthesiologists, this case can support some evidence for recognizing an airway problem with craniofacial disfigurement in PS patients.
References
1. Biesecker L. The challenges of Proteus syndrome: diagnosis and management. Eur J Hum Genet. 2006; 14:1151–1157. PMID: 16883308.

2. Wiedemann HR, Burgio GR, Aldenhoff P, Kunze J, Kaufmann HJ, Schirg E. The proteus syndrome. Partial gigantism of the hands and/or feet, nevi, hemihypertrophy, subcutaneous tumors, macrocephaly or other skull anomalies and possible accelerated growth and visceral affections. Eur J Pediatr. 1983; 140:5–12. PMID: 6873112.
3. Pennant JH, Harris MF. Anaesthesia for Proteus syndrome. Anaesthesia. 1991; 46:126–128. PMID: 1872427.

4. Turner JT, Cohen MM Jr, Biesecker LG. Reassessment of the Proteus syndrome literature: application of diagnostic criteria to published cases. Am J Med Genet A. 2004; 130A:111–122. PMID: 15372514.

5. Nakane M, Sato M, Hattori H, Matsumoto Y, Otsuki M, Murakawa M. Perioperative respiratory complications caused by cystic lung malformation in Proteus syndrome. J Anesth. 2006; 20:26–29. PMID: 16421672.

6. Pradhan A, Sen I, Batra YK, Biswas G. Proteus syndrome: a concern for the anesthesiologist. Anesth Analg. 2003; 96:915–916. PMID: 12598301.

7. Sinha C, Gupta B, Kaur M, Kumar A, Dey CK. Proteus syndrome: A medical rarity. Saudi J Anaesth. 2011; 5:233–234. PMID: 21804811.

8. Cekmen N, Kordan AZ, Tuncer B, Gungor I, Akcabay M. Anesthesia for proteus syndrome. Paediatr Anaesth. 2004; 14:689–692. PMID: 15283831.

9. Sahni JK, Kumar S, Wadhwa V, Kathuria G. Proteus syndrome with huge tonsillar mass causing dysphagia: a rare case. J Laryngol Otol. 2006; 120:408–410. PMID: 16556346.

10. Law JA, Broemling N, Cooper RM, Drolet P, Duggan LV, Griesdale DE, et al. The difficult airway with recommendations for management--part 2--the anticipated difficult airway. Can J Anaesth. 2013; 60:1119–1138. PMID: 24132408.
11. Xue FS, Luo MP, Xu YC, Liao X. Airway anesthesia for awake fiberoptic intubation in management of pediatric difficult airways. Paediatr Anaesth. 2008; 18:1264–1265. PMID: 19076599.

Fig. 3
Photograph shows bronchoscopic views of larynx (A–C), vocal cord (D, E), tracheal lumen (F), and carina (G) with multiple protruded mass lesions due to overgrowth of connective tissue. Computed tomography (H) shows nasopharyngeal mucosal hypertrophy with adenoid vegetation and deviated nasal septum to the right side. The image also shows mucosal hypertrophy at nasal cavity and inferior turbinate with narrowing of nasopharynx.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download