Abstract
Background
The current state of general hospital operation room (OR) in Korea and how these ORs are being operated remain unclear. Therefore, the aim of this study was to investigate and assess the current state of OR management and surgical scheduling in general hospitals of Korea.
Methods
A total of 92 anesthesiology training hospitals and 2 equivalent hospitals in Korea were targeted for the survey. Anesthesiologists in hospitals received questionnaires for OR, anesthetic managements and surgical scheduling directly or by phone from the beginning of October 2015 to the end of December 2015.
Results
Of the 94 hospitals that were targeted, 59 hospitals (62.7%) responded to the survey. Of the 59 hospitals, 40 (67.8%) had 500–1,000 beds, 36 (61.0%) had 11–20 ORs. Most OR arrangements were made by residents and specialists in Anesthesiology Department (90%). Most hospitals (47.4%) in the response set performed total surgeries in the range of 10,000 to 20,000 annually. The proportion of emergency surgeries in the total surgeries was 2.8–55.0%. Methods for predicting expected surgery time were arbitrarily decided by surgeons (61%), anesthesiologist's experience (20%), or by analyzing historical data using software (5%).
The number of surgery cases in Korea was 3,302.89 per 100,000 people in 2013 [1]. This number has a gradual upward trend. Facing the ever increasing health care demand and competition with limited government support, hospitals are more and more aware of the need to use their resources as efficiently as possible [2]. Operation room (OR) is a major production unit in every hospital. It is also a challenging unit as it unites many stakeholders such as surgeons, nurses, and patients. Hospital management is characterized by scarce, costly, and interrelated resources [3]. For these reasons, strategic or tactical planning and scheduling OR activities have become major priorities for hospitals and OR managing committees [3].
To improve financial efficiency in OR, a variety of perspectives such as scheduling efficiency, operational efficiency (requiring work process redesign), practitioner-centered efficiency, and patient-centered efficiency have emerged as quality issues in the medical field [456]. To the best of our knowledge, no study has been performed to increase the efficiency of OR in Korea. Therefore, the objective of this study was to determine the current state of general hospital ORs in Korea and its management. We conducted a questionnaire survey to investigate and assess the current state of OR operation and surgical scheduling in general hospitals of Korea to help establish efficient OR operational system in the future.
The study protocol was reviewed by the Institutional Review Board. It was approved as a minimal risk study without requiring individual consent based on institutional guidelines. Therefore, consent was waived.
Starting from the set of Korean academic hospitals provided by the Korean Hospital Association, we targeted 92 anesthesiology training hospitals and 2 equivalent hospitals in Korea. Anesthesiologists in the hospitals received questionnaires directly or by phone from the beginning of October 2015 to the end of December 2015. Our search eventually resulted in 59 hospitals (both private and public) equipped with functional OR. Their answers were registered on an electronic questionnaire by the respondent or the questioner. We preferred this method to regular postal services as it allowed automated registration of answers in a spreadsheet. Moreover, this method is quicker, more cost-effective, and more user-friendly compared to regular postal services.
The questionnaire was kept as brief as possible (a printout of about 3 A4 pages). It covered general questions about the hospital and issues related to OR management, scheduling process for both elective and emergency surgeries. For most questions that were either quantitative or qualitative in nature, we suggested a list of possible answers. Participating hospitals received a summary of the results afterwards.
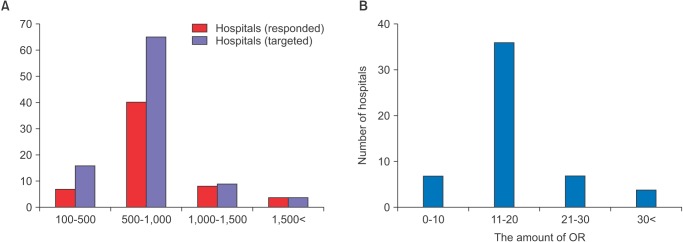
Of the 94 hospitals that we initially targeted, 59 (62.7%) responded to the survey, including 57 anesthesiology training hospitals and 2 equivalent hospitals. Hospitals connected to School of Medicine in Korea were all included in the responded hospitals. The numbers of beds in the targeted 94 hospitals and the 59 hospitals that actually responded to the survey were compared to each other (Fig. 1A).
Sixty-five (69.1%) of the total 94 hospitals and 40 (67.8%) of the 59 hospitals that completed the survey had 500–1,000 beds. Thirty-six (61%) of the 59 responded hospitals had 11–20 ORs (Fig. 1B). The higher the number of hospital beds, the higher the number of ORs (correlation coefficient = 0.85). Sixty-three percent of the responded hospitals were satisfied with their current OR capacities. However, 37% of these hospitals were not satisfied with their current OR capacities due to insufficient OR.
ORs were mainly (61%) managed by anesthetic residents. Approximately 29% ORs were managed by anesthetic staffs. Only 2% ORs were managed by nurses. OR management software program was not used in any hospital.
The most important objective in OR managements was questioned. About 43% of respondents indicated that high utilization of ORs was the most important objective. It had the highest score among all objectives. Avoiding overtime in the ORs also seemed to be highly important (32%). Throughput/lead time (the time between scheduling surgeries and completing the scheduled surgeries), preferences surgical start time and OR structure of surgeon, or anesthesiologist did not seem to be of major interest to respondents (10%, 3%, and 2%, respectively).
Methods for obtaining expected surgery time were questioned. Three approaches were applied in hospitals in order to estimate surgery durations. Surgery duration was either arbitrarily decided by a surgeon (61%), anesthesiologist's experience (20%), or by analyzing historical data using software (5%).
The OR management committee provides advice and consultation on the function and performance of ORs, including operational efficiency, quality, safety, and service. Most of these hospitals (86%) had an OR management committee. The chairs of the OR management committee were either anesthesiologists (66%), surgeons (17%), or administrators (9%).
We surveyed whether these hospitals had PEC. Most of these hospitals (75%) did not have PEC. Only 25% of these responded hospitals operated PEC.
Assignment of one nurse to several rooms was the most common (at 34%), followed by assignment of one nurse to every room (at 32%) and assignment of one monitoring nurse to a specific OR (at 19%).
Forty (67.8%) of the 59 responded hospitals did not have electric anesthetic records. Only 18 hospitals (30.5%) had electric anesthetic records.
The total amount of surgeries and emergency surgeries performed in 2014 were surveyed. Most (47%) hospitals in the response set performed annual surgeries of 10,000 to 20,000 (Fig. 2A). The proportion of emergency surgeries in total surgeries was 2.8–55.0%. However, 10 to 30% emergency surgeries were performed in 32 hospitals (54%) of the 59 responded hospitals (Fig. 2B).
The more the number of OR, the higher the number of total surgeries performed, including surgeries requiring general anesthesia and surgeries under local or regional anesthesia (correlation coefficient = 0.84). Similarly, the more the number of OR, the higher the number of emergency surgeries (correlation coefficient = 0.61).
We surveyed whether these hospitals had dedicated OR for emergency surgeries. Only 17% of them had dedicated OR. However, anesthetic nurses and anesthesiologists were not designated for emergency surgeries.
The proportion of emergency surgery and current state of OR management were surveyed in this study. For general surgical emergencies, around 10% of operations in high-income countries and 21–90% in low- to middle- income countries are performed [78]. According to the American College of Surgeons National Surgical Quality Improvement Program data, an average of 14.7% of surgeries performed in 198 U.S. hospitals between 2005 and 2008 were emergency surgeries [9]. Although more than half of responded Korean hospitals had 10–30% operations performed in the form of emergency surgeries, this survey showed wide variations in emergency surgeries performed (from 2.8 to 55.0%). Cancer dedicated and specialized hospitals had the lowest percentages of emergency surgeries performed. On the contrary, hospitals that had not any other large scale hospitals nearby had higher proportion of emergency surgeries. Therefore, demands for dedicated emergency ORs has been raised to improve the efficiency of the emergency surgeries. Dedicated ORs for emergency cases has been reported to improve quality of care by decreasing cancellations and overruns in elective rooms [10]. However, using dedicated ORs for orthopedic trauma cases remains controversial. Emergency patients could be operated more efficiently on elective ORs instead of dedicated emergency ORs [1112]. Further study is needed to investigate OR efficiency and waiting time for emergency operations.
There might be differences in the current state of OR management and surgical scheduling between the targeted 94 hospitals and the 59 hospitals that actually responded to the survey. However, since the percent deviations of the total 94 hospitals and of the 59 hospitals that completed the survey had 100–500, 500–1,000, 1,000–1,500 and > 1,500 beds were below 5%, we considered the bias to be negligible. Therefore, the response set could represent resident training hospitals of Korea.
To maximize OR utilization, better estimates of case duration lengths are needed. Only 5% hospitals of responded sets used software to analyze historical data. This is much lower than the 30% of software utilization rate in a survey reported by Flanders [3]. The duration of operative procedures could be modeled as a lognormal variable with mean and standard deviations obtained by historic operative data. However, a regression methodology to predict case length has been reported to be a promising method in decreasing uncertainty about surgical case length than the standard method of surgical length prediction using historical means [13]. A recent computerized simulation study has demonstrated that using a predictive modeling system by incorporating patient and surgery-specific factors is superior to scheduling with duration prediction based on historical means per surgeon in both throughput and OR efficiency [14].
This survey revealed that OR arrangements were mainly performed by anesthetic residents and staffs in 90% of the responded hospitals. OR managers are responsible of determining the OR capacity and assigning capacity to different medical specialists. Increases in the efficiency of using ORs can result in more production and more revenue for the hospital. However, operational management courses are currently lacking in the Korean academic educational programs. It should be considered in the research and education areas. Educational tools can help OR managers learn the consequences triggered by their operational policy and managerial decisions. OR efficiency can be affected by the personalities of OR managers in risk-taking in planning schedules. Risk-averse OR managers might cancel elective cases scheduled for surgery compared to a risk-taking OR managers [15]. In addition, OR managers need to frequently communicate and negotiate with various stakeholders, such as anesthesiologists, surgeons, and other OR staff. Significant improvements in OR efficiency can be achieved by better organizing the flow of work. In addition, multi-disciplinary efforts of surgeons, anesthesiologists, and nurses supervised and integrated by OR managers are necessary [16]. Education for management-related skill areas such as communication, human relation skills, use of supervisory power, and self–assessing tools for his/her risk appreciation could be helpful in training anesthetic residents.
This survey revealed that 15% of the responded hospitals had PEC. It has been reported that PEC can minimize cancellation rate and reduce any adverse effects of surgeries or procedures, thus increasing the level of satisfaction of both patients and surgeons while reducing medical costs for regularly scheduled surgeries [1718192021]. However, there are specific and unique personnel and system requirements for the accumulation of multidisciplinary information in PEC. The justification for this type of program is that cost saving can be realized by decreasing wasted operating room time due to inadequate or incomplete patient preparation [22]. Financial efficiency and patient-centered efficiency might have conflicting interests and operating PEC should be considered in terms of hospital policy.
Nursing staffing to patient ratios and their education level have great impact on hospital mortality [2324]. However, unfortunately there is no recommended nursing staff ratio in OR or in a post-anesthesia setting. Meanwhile, factor in different roles of nurses (monitoring patients or assisting anesthesiologists) should be considered.
In conclusion, we conducted a questionnaire survey to investigate and assess the current state of OR operation and surgical management in general hospitals of Korea. This survey study might trigger active operational researches for OR efficiency. It might help hospital policy makers manage OR resources more efficiently.
References
1. 2013 Statistical Yearbook of major surgery [Internet]. Wonju (KR): National Health Insurance Service;2014. 12. 31. cited 2016 Feb 24. Available from http://www.nhis.or.kr/bbs7/attachments/15841.
3. Cardoen B, Demeulemeester E, Beliën J. Operating room planning and scheduling: a literature review. Eur J Oper Res. 2010; 201:921–932.

4. Archer T, Macario A. The drive for operating room efficiency will increase quality of patient care. Curr Opin Anaesthesiol. 2006; 19:171–176. PMID: 16552224.

5. Baumgart A, Schüpfer G, Welker A, Bender HJ, Schleppers A. Status quo and current trends of operating room management in Germany. Curr Opin Anaesthesiol. 2010; 23:193–200. PMID: 20071981.

6. Marjamaa R, Vakkuri A, Kirvelä O. Operating room management: why, how and by whom. Acta Anaesthesiol Scand. 2008; 52:596–600. PMID: 18419711.

7. Shafi S, Aboutanos MB, Agarwal S Jr, Brown CV, Crandall M, Feliciano DV, et al. Emergency general surgery: definition and estimated burden of disease. J Trauma Acute Care Surg. 2013; 74:1092–1097. PMID: 23511150.
8. Smith M, Hussain A, Xiao J, Scheidler W, Reddy H, Olugbade K Jr, et al. The importance of improving the quality of emergency surgery for a regional quality collaborative. Ann Surg. 2013; 257:596–602. PMID: 23470507.

9. Ingraham AM, Cohen ME, Raval MV, Ko CY, Nathens AB. Comparison of hospital performance in emergency versus elective general surgery operations at 198 hospitals. J Am Coll Surg. 2011; 212:20–28.e1. PMID: 21184955.

10. Heng M, Wright JG. Dedicated operating room for emergency surgery improves access and efficiency. Can J Surg. 2013; 56:167–174. PMID: 23706847.

11. Bhattacharyya T, Vrahas MS, Morrison SM, Kim E, Wiklund RA, Smith RM, et al. The value of the dedicated orthopaedic trauma operating room. J Trauma. 2006; 60:1336–1340. PMID: 16766980.

12. Wullink G, Van Houdenhoven M, Hans EW, van Oostrum JM, van der Lans M, Kazemier G. Closing emergency operating rooms improves efficiency. J Med Syst. 2007; 31:543–546. PMID: 18041289.

13. Kougias P, Tiwari V, Orcutt S, Chen A, Pisimisis G, Barshes NR, et al. Derivation and out-of-sample validation of a modeling system to predict length of surgery. Am J Surg. 2012; 204:563–568. PMID: 23140826.

14. Kougias P, Tiwari V, Berger DH. Use of simulation to assess a statistically driven surgical scheduling system. J Surg Res. 2016; 201:306–312. PMID: 27020812.

15. Stepaniak PS, Mannaerts GH, de Quelerij M, de Vries G. The effect of the Operating Room Coordinator's risk appreciation on operating room efficiency. Anesth Analg. 2009; 108:1249–1256. PMID: 19299796.

16. Sokolovic E, Biro P, Wyss P, Werthemann C, Haller U, Spahn D, et al. Impact of the reduction of anaesthesia turnover time on operating room efficiency. Eur J Anaesthesiol. 2002; 19:560–563. PMID: 12200944.

17. Parker BM, Tetzlaff JE, Litaker DL, Maurer WG. Redefining the preoperative evaluation process and the role of the anesthesiologist. J Clin Anesth. 2000; 12:350–356. PMID: 11025233.

18. Cantlay KL, Baker S, Parry A, Danjoux G. The impact of a consultant anaesthetist led pre-operative assessment clinic on patients undergoing major vascular surgery. Anaesthesia. 2006; 61:234–239. PMID: 16480347.

19. Flynn BC, Silvay G. Value of specialized preanesthetic clinic for cardiac and major vascular surgery patients. Mt Sinai J Med. 2012; 79:13–24. PMID: 22238035.

20. Correll DJ, Bader AM, Hull MW, Hsu C, Tsen LC, Hepner DL. Value of preoperative clinic visits in identifying issues with potential impact on operating room efficiency. Anesthesiology. 2006; 105:1254–1259. PMID: 17122589.

21. Farasatkish R, Aghdaii N, Azarfarin R, Yazdanian F. Can preoperative anesthesia consultation clinic help to reduce operating room cancellation rate of cardiac surgery on the day of surgery. Middle East J Anaesthesiol. 2009; 20:93–96. PMID: 19266833.
22. Ferrari LR. Preoperative evaluation of pediatric surgical patients with multisystem considerations. Anesth Analg. 2004; 99:1058–1069. PMID: 15385351.

23. Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Griffiths P, Busse R, et al. Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet. 2014; 383:1824–1830. PMID: 24581683.

24. Silber JH, Rosenbaum PR, McHugh MD, Ludwig JM, Smith HL, Niknam BA, et al. Comparison of the value of nursing work environments in hospitals across different levels of patient risk. JAMA Surg. 2016; 151:527–536. PMID: 26791112.





 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download