Abstract
Pneumocephalus is common after brain surgeries, but usually is not substantial enough to cause serious complications. We recently encountered a case of post-operative tachypnea after an endoscopic 3rd ventriculostomy. At first, we thought that the hyperventilation was the result of residual paralysis after emergence from anesthesia, but during further evaluation we found a massive pneumocephalus. In such unusual post-operative situations, physicians should consider surgery-related complications as the possible cause as well, along with the anesthetic factors.
Go to : 
Obesity and incomplete reversal of neuromuscular blockade are risk factors for post-operative airway compromise in postanesthetic care units (PACUs) [123]. Respiratory complications occur from surgical factors as well, especially after brain, thoracic, or head and neck surgeries [34]. We recently anesthetized an obese patient with risk factors for difficult airway management. The patient received 3rd ventriculostomy (ETV). Despite all preventative measures, the patient experienced tachypnea in the PACU. It turned out that the tachypnea was caused by a neurologic problem secondary to an unexpected massive pneumocephalus. Here, we present a case of tachypnea caused by a pneumocephalus.
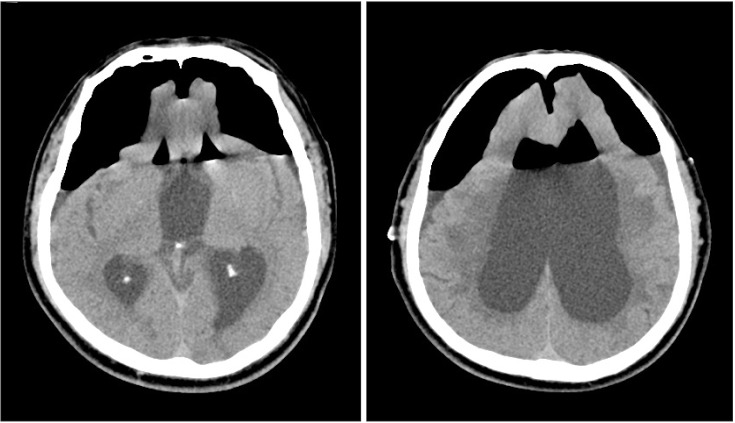
A 59-year-old man diagnosed with obstructive hydrocephalus was scheduled for an ETV. The patient had a medical history of well-controlled diabetes mellitus and hypertension that was being treated with an angiotensin receptor blocker, a calcium channel blocker, and a beta blocker. The body mass index was 33.8, but he had no respiratory symptoms, including sleep apnea. A preoperative chest X-ray showed mild cardiomegaly but electrocardiography and echocardiogram findings were normal. The patient's symptoms were amnesia, gait disturbance, and urinary incontinence that had persisted for 5 months; preoperatively, he was alert and cooperative and had no problem communicating. The preoperative vital signs were: blood pressure, 110/70 mmHg; heart rate, 59 beats/min; respiratory rate, 18 breaths/min; and oxygen saturation, 96%. Since the appearance of the patient suggested a possible difficult intubation, a video laryngoscope was used for tracheal intubation after induction of general anesthesia with 150 mg propofol 1%, 40 mg lidocaine 2%, and 60 mg rocuronium. The vocal cord was clearly visible on the video laryngoscope and the intubation was accomplished without trauma or other difficulties. Anesthesia was maintained with 5% desflurane and 0.02 µg/kg/min remifentanil, and air with 50% oxygen. The surgery lasted 2 hours and required no additional muscle relaxants. During the surgery, there was sudden and sustained hypotension (mean blood pressure 52–57 mmHg) with bradycardia (heart rate 45–55 beats/min) that did not respond well to ephedrine; these complications began about 10 min after the beginning of the surgery and lasted for 25 min until a dopamine infusion was administered that restored normal blood pressure. Remifentanil infusion was discontinued at the onset of hypotension and bradycardia. After the purge of volatile agents at the end of the surgery, the train of four (TOF) count was 4, and the ratio was 50%, so 2 mg/kg of sugammadex was injected. The patient recovered muscle power within a few minutes, showing firm hand grip, head elevation, and mouth opening, and was fully obeying verbal commands, but was not opening his eyes. As he was alert and cooperative at that point and no other neurologic deficit was observed, the neurosurgeons thought that the inability to open his eyes was not related to the surgery. We relieved the bandage on the head in order to reduce the chance of unintended pressure or tension on the forehead, and suggested that further neurologic examinations be done after full recovery from anesthesia. Spontaneous respiration was present, showing expired tidal volumes reaching 500 ml each time, but was tachypneic; the patient's respiratory rate ranged from 40 to 50 breaths/min. This condition continued for 5 min, at which time the patient was extubated and transferred to the PACU under mask ventilation. The patient showed signs of inspiratory stridor, chest retractions, and hoarse voice after the extubation. The patient's accessory respiratory muscles were not involved in the hyperventilation. There was no crackle or wheezing clear on auscultation besides the inspiratory stridor, but the findings were not clear on account of the hoarse voice and the rapid and dynamic ventilation. An additional 2 mg/kg of sugammadex was injected in the PACU under the theory that the patient's upper airway was obstructed because of possible residual paralysis but the condition did not change. The patient was fully responsive to verbal commands but was still unable to open his eyes or hold his breath and he complained of feeling like he was choking despite the hyperventilation. Arterial blood gas analysis (ABGA) at that point showed: pH, 7.35; pCO2, 37 mmHg; pO2, 76 mmHg; HCO3, 20.4 mmol/L; and O2 saturation, 94%. The vital signs at that point were: blood pressure, 150/90 mmHg; heart rate, 110 beats/min; and respiratory rate, 44 breaths/min. Since tachypnea (40–50 breaths/min) persisted for 20 min in the PACU and oxygen saturation started to drop under 95%, 200 mg thiopental sodium and 100 mg succinylcholine were injected and endotracheal intubation was performed. Endotracheal suction was done immediately after intubation and there was no sputum or discharge. Auscultation right after the re-intubation sounded smooth, without crackle or wheezing, and the oxygen saturation rapidly corrected to 100%. Tachypnea persisted even under sedation after the succinylcholine wore off, so a central cause was suspected. Computed tomography (CT) revealed a massive pneumocephalus with pneumoventricle and hydrocephalus (Fig. 1). A chest X-ray taken after the brain CT showed no pathologic findings such as pulmonary edema, congestion, or pneumothorax. On the neurosurgeon's recommendation, the patient was transferred to the intensive care unit and was kept there for three days under mechanical ventilation with sedation with midazolam, cisatracurium, and rocuronium until the pneumocephalus and tachypnea spontaneously resolved. Follow-up chest radiographs were taken over the next 3 weeks and showed nothing abnormal. According to a pulmonology consultation, the tachypnea was not likely to have originated from pulmonary problems. ABGA results stayed within normal limits under fully controlled mechanical ventilation but showed hypoxemia when the patient gained spontaneous respiration during the sedative period before the resolution of the pneumocephalus. Since the follow-up chest X-rays showed no abnormal findings, pulmonary embolism evaluation including embolism CT and laboratory examinations, which also showed nothing abnormal, were done on the recommendation of a pulmonologist. When a follow-up brain CT showed resolution of the pneumocephalus on the 3rd day after the surgery, sedative and neuromuscular blocking agents were discontinued and the mechanical ventilation mode was switched to synchronized intermittent mandatory ventilation. The respiratory rate at that point ranged from 15 to 20 breaths/min and ABGA results remained normal when the patient gained consciousness and self-respiration, so the endotracheal tube was extubated. The patient is now (30 days post-operation) in the general ward; he is mentally alert and has stable vital signs but still is unable to open his eyes because of bilateral ptosis and is receiving conservative treatment.
Go to : 
There are many factors that can cause airway problems in the PACU, including surgical factors. Obese patients have a higher risk of difficult intubations and post-operative respiratory complications [56]. In the present case, because our patient was obese and had a short, thick neck and small chin, we were concerned about the difficulty of intubation and upper airway obstruction or recurarization after emergence from anesthesia. Thus, we used a video laryngoscope for the intubation and sugammadex for the reversal of the muscle relaxant. Since persistent tachypnea and difficulties with inspiration after anesthesia often indicate upper airway obstruction [7], and there was no likelier cause than residual paralysis of the patient's obese airway, we injected additional sugammadex upon the onset of these symptoms [6]. Although the dose of additional sugammadex should be guided by neuromuscular monitoring, it was not possible to run TOF on our patient in the PACU as he was alert and actively moving his extremities [8]. So, the additional dose was based on a clinical decision. Since there was no anesthetic factor left to consider as the cause and the patient was fully alert and cooperative except for bilateral ptosis and loss of control of breathing, we performed the treatment to rule out residual paralysis which is a common cause of respiration problems in PACU.
Pneumocephalus is common after brain surgeries but usually is small, asymptomatic, and does not significantly affect surgical outcomes [910]. However, if it becomes brainstem tension pneumocephalus, it can cause hyperventilation during the early phase of herniation by compressing the brainstem and thereby causing malfunction in the respiratory centers of the medulla oblongata or pons [1112]. In the present case, not only was the pneumocephalus massive enough to cause brainstem symptoms but also, despite the ETV, there was still hydrocephalus and a pneumoventricle which led to extensive dilation of the ventricles. The pneumocephalus might have exerted additional pressure on top of the pressure caused by the pneumoventricle and unresolved hydrocephalus. These might have caused not only the post-operative respiratory symptoms but also the intra-operative sudden hypotension and bradycardia as such a large pneumocephalus can cause various hemodynamic disturbances along with symptoms of transtentorial herniation [1314]. In the PACU, we did not immediately suspect a neurological cause of the tachypnea because of the patient's stable vital signs, alert mental state, and absence of other neurological deficits, along with the assumption that the hydrocephalus must have been resolved by the surgery; we focused instead on the possibility of an upper airway problem. Had we considered surgical factors along with anesthetic factors, we may have suspected pneumocephalus or another neurological problem and thus saved time and effort and, most importantly, reduced the patient's suffering and any further risk to his health. That the patient, even 30 days after the surgery, is still not able to open his eyes because of bilateral ptosis, which is a possible consequence of hydrocephalus [15], emphasizes the fact that surgical factors may be involved when a post-operative patient develops unexplained symptoms.
In conclusion, when there is no anesthetic factor left to consider as the cause of unexpected post-operative complications, physicians should consider surgery-related complications as a possible cause as well.
Go to : 
References
1. Norton M, Xará D, Parente D, Barbosa M, Abelha FJ. Residual neuromuscular block as a risk factor for critical respiratory events in the post anesthesia care unit. Rev Esp Anestesiol Reanim. 2013; 60:190–196. PMID: 23453244.

2. Kandasamy T, Wright ED, Fuller J, Rotenberg BW. The incidence of early post-operative complications following uvulopalatopharyngoplasty: identification of predictive risk factors. J Otolaryngol Head Neck Surg. 2013; 42:15. PMID: 23570393.

3. Rose DK, Cohen MM, Wigglesworth DF, DeBoer DP. Critical respiratory events in the postanesthesia care unit. Patient, surgical, and anesthetic factors. Anesthesiology. 1994; 81:410–418. PMID: 8053592.
4. Manninen PH, Raman SK, Boyle K, el-Beheiry H. Early postoperative complications following neurosurgical procedures. Can J Anaesth. 1999; 46:7–14. PMID: 10078396.

5. Biro P, Kaplan V, Bloch KE. Anesthetic management of a patient with obstructive sleep apnea syndrome and difficult airway access. J Clin Anesth. 1995; 7:417–421. PMID: 7576679.

6. Piper AJ, Grunstein RR. Obesity hypoventilation syndrome: mechanisms and management. Am J Respir Crit Care Med. 2011; 183:292–298. PMID: 21037018.
7. Sasidaran K, Bansal A, Singhi S. Acute upper airway obstruction. Indian J Pediatr. 2011; 78:1256–1261. PMID: 21559808.

8. Sokół-Kobielska E. Sugammadex - indications and clinical use. Anaesthesiol Intensive Ther. 2013; 45:106–110. PMID: 23877905.
9. Ihab Z. Pneumocephalus after surgical evacuation of chronic subdural hematoma: Is it a serious complication? Asian J Neurosurg. 2012; 7:66–74. PMID: 22870154.

10. Reasoner DK, Todd MM, Scamman FL, Warner DS. The incidence of pneumocephalus after supratentorial craniotomy. Observations on the disappearance of intracranial air. Anesthesiology. 1994; 80:1008–1012. PMID: 8017640.
11. Prakash PS, Jain V, Sandhu K, Walia BS, Panigrahi BP. Brain stem tension pneumocephalus leading to respiratory distress after subdural haematoma evacuation. Eur J Anaesthesiol. 2009; 26:795–797. PMID: 19424072.

12. Nogués MA, Benarroch E. Abnormalities of respiratory control and the respiratory motor unit. Neurologist. 2008; 14:273–288. PMID: 18784597.

13. Endo T, Sato K, Takahashi T, Kato M. Acute hypotension and bradycardia by medulla oblongata compression in spinal surgery. J Neurosurg Anesthesiol. 2001; 13:310–313. PMID: 11733662.

14. Bor-Seng-Shu E, Paiva WS, Figueiredo EG, Fujimoto Y, de Andrade AF, Fonoff ET, et al. Posttraumatic refractory intracranial hypertension and brain herniation syndrome: cerebral hemodynamic assessment before decompressive craniectomy. Biomed Res Int. 2013; 2013:750809. PMID: 24377095.

15. Suzuki H, Matsubara T, Kanamaru K, Kojima T. Chronic hydrocephalus presenting with bilateral ptosis after minor head injury: case report. Neurosurgery. 2000; 47:977–979. PMID: 11014441.

Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download