Abstract
Background
Sore throat and hoarseness are common complications after general anesthesia with tracheal intubation. The position for patients can affect the incidence of postoperative sore throat (POST) by causing displacement of the endotracheal tube. This study investigated the prophylactic effect of dexamethasone in prone position surgeries.
Methods
One hundred-fifty patients undergoing lumbar spine surgery (18-75 yr) were randomly allocated into the normal saline group (group P, n = 50), dexamethasone 0.1 mg/kg group (group D1, n = 50) or dexamethasone 0.2 mg/kg group (group D2, n = 50). The incidence and severity of POST, hoarseness, and cough were measured using direct interview at 1, 6, and 24 h after tracheal extubation. The severity of POST, hoarseness, and cough were graded using a 4-point scale.
Results
At 1, 6, and 24 h after extubation, the incidence of sore throat was significantly lower in group D1 (1 h; P = 0.015, 6 h; P < 0.001, 24 h; P = 0.038) and group D2 (1 h; P < 0.001, 6 h; P < 0.001, 24 h; P = 0.017) compared to group P. There were less number of patients in the groups D1 and D2 than group P suffering from moderate grade of POST at 1, 24 h after extubation. The incidence of hoarseness at 1, 6, and 24 h after extubation was significantly lower in groups D2 than group P (P < 0.001). There were no significant differences in the incidence of cough among the three groups.
Sore throat is common complication after surgery with tracheal intubation. It is said that postoperative sore throat (POST) is one of the outcomes that patients want to avoid after anesthesia. It adversely affects the satisfaction and activities of the patients after leaving hospital [123]. Incidence of sore throat is reported to range from 14.4% to 50.0% [45] and depends on various factors such as age, sex, the size and cuff pressure of the endotracheal tube, the duration for which the tube is in place, number of suctioning attempts, and the time and manipulations needed to insert the tube [67].
Dexamethasone is extensively used for the remedy of a sore throat arising from tracheal mechanical stimulation. It is a powerful glucocorticoid with anti-inflammatory and painkilling effects and anti-emetic properties [891011]. It may have the potential for decreasing the incidence of POST during recovery, and the mechanism for this result is probably by modifying the inflammatory process caused by tissue injury [121314].
The position change from supine to prone can make a change in endotracheal tube cuff pressure and endotracheal tube displacement [1516]. The change in cuff pressure and tube displacement can affect the incidence of POST, hoarseness, and cough [67]. As previous studies only studied the effect of dexamethasone in supine position surgeries, this study investigated the prophylactic effect of dexamethasone in decreasing POST, hoarseness, and cough in prone position surgeries.
After we got approval from the Institutional Review Board for this study, written informed consent was obtained from all patients. One hundred-fifty patients aged between 18 to 75 years, American Society of Anesthesiologists (ASA) physical status I-III, requiring lumbar spine surgery under general anesthesia with endotracheal intubation were prospectively investigated.
Patients with a history of recent respiratory tract infection, prior medication with analgesics or corticosteroids were excluded. Other exclusion criteria included patients who had preoperative sore throat, hoarseness and cough, had a neuromuscular disease or had a nasogastric tube, had a duration of tracheal intubation of < 60 min or > 300 min, and required more than one attempt for tracheal intubation.
Using a computer-generated random number table, the patients were randomly allocated into the normal saline group (placebo, group P, n = 50), dexamethasone 0.1 mg/kg group (group D1, n = 50) or dexamethasone 0.2 mg/kg group (group D2, n = 50) before anesthesia induction. An anesthetic nurse, who was not taking part in postoperative patient interview and assessment, prepared the study drugs (dexamethasone or normal saline) as a 4 ml clear solution in identical syringes and anesthesiologists were blinded to the syringe contents.
Patients were premedicated with intramuscular injection of 0.2 mg of glycopyrrolate and intravenous injection of 50 mg ranitidine. Non-invasive blood pressure, electrocardiography, pulse oximetry, and bispectral index were applied when the patients arrived in the operating room. The study drug was injected intravenously before anesthetic induction.
Anesthesia was induced with fentanyl 100 µg, propofol 2 mg/kg and rocuronium 0.6 mg/kg. We ventilated all patients with 100% oxygen via a facial mask. We performed tracheal intubation after confirming adequate muscle relaxation (the absence of movement and jaw relaxation). Endotracheal intubation was performed with tubes having an internal diameter of 8.0 or 7.5 mm for male patients, and 7.5 or 7.0 mm for female patients. After intubation, we inflated the tracheal tube cuff with room air at once and tuned the cuff pressure between 10 and 20 cmH2O using a cuff pressure manometer (Cuff Pressure Gauge; VBM Medizintechnik, DE). Patient's position was changed from supine to prone for surgery, and patient's head was positioned on the sponge face pillow without head rotation. After position change from supine to prone, we re-adjusted the cuff pressure between 10 and 20 cmH2O. All groups did not use humidifiers or heat and moisture exchangers. Anesthesia was maintained with 1.5-2.5 vol% sevoflurane and 50% in air. The end-tidal CO2 was kept between 35 and 40 mmHg.
When the surgeon began to suture the skin, an IV patient-controlled analgesia (PCA) pump (GemStar™ Infusion System, Hospira, Inc., Lake Forest, IL, USA) containing fentanyl 30 µg/kg and ramosetron 0.6 mg in normal saline with total volume of 100 ml was connected. This pump programmed to deliver 1 ml/h as background infusion with a 1 ml bolus at 10 min lockout period.
After the end of surgery, residual neuromuscular block was reversed with pyridostigmine 0.3 mg/kg and glycopyrrolate 0.01 mg/kg. Oral secretion was suctioned gently once. The endotracheal tube was removed when the patient was able to obey commands and lung ventilation was considered adequate.
Cricoid compression, duration of tracheal intubation, duration of prone position, duration of anesthetic time, and incidence of cough during extubation were recorded. The incidence and severity of POST, hoarseness, cough, and postoperative pain visual analog scale (VAS) were measured using direct interview by researcher who did not participate in this study at 1, 6, and 24 h after extubation. The severity of POST, hoarseness, and cough was graded using a 4-point scale (0: no, 1: minimal, 2: moderate, 3: severe) (Table 1) [13] Postoperative pain was assessed using a VAS (0 = no pain to 10 = the most severe pain).
The sample size was estimated from preliminary data obtained from 40 patients, and the assumption that a 20% reduction in the incidence of POST would be clinically relevant. The power analysis suggested that a minimum of 44 patients in each group would be needed for a β = 0.2, α = 0.05, (adjusted Bonferroni's p-value). To compensate for potential dropouts (drop rate = 10%), 50 patients were enrolled in each group.
The results are expressed as the mean ± SD or number of patients (%). The demographic data and continuous data (duration of tracheal intubation, duration of prone position, and anesthetic duration) were analyzed using one-way ANOVA. Categorical data (gender, ASA status, size of endotracheal tube, external compression during intubation, cough during extubation, and incidence and severity of sore throat, hoarseness, and cough among the three groups) were analyzed by chi-square test. All follow-up analyses were corrected the Bonferroni adjustments. Values of P < 0.05 were considered statistically significant.
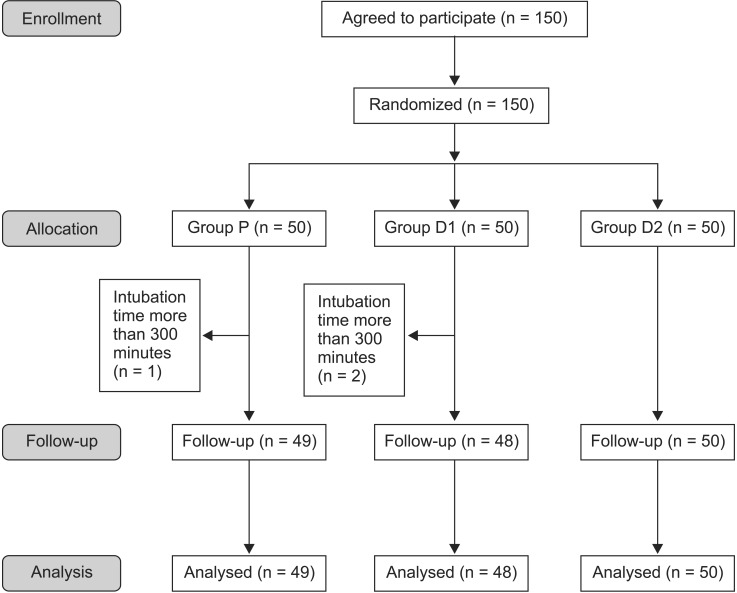
Of the 150 enrolled patients, 3 patients were excluded from the analysis (1 in Group P and 2 in Group D1): three patients had an intubation time of more than 300 minutes (Fig. 1). The characteristics of these 147 patients are summarized in Table 2. There were no significant differences among the three groups with respect to age, weight, height, gender, ASA status. There were no significant differences in the duration of tracheal intubation and prone position, and the anesthetic time, and postoperative pain VAS score among the three groups. There were no significant differences in the size of endotracheal tube and external compression during intubation.
At 1, 6, and 24 h after extubation, the incidence of POST was significantly lower in group D1 (1 h; 40% , P = 0.015 / 6 h; 17%, P < 0.001 / 24 h; 4%, P = 0.038) and group D2 (1 h; 30% , P < 0.001 / 6 h; 4% , P < 0.001 / 24 h; 2%, P = 0.017) compared to group P (1 h; 67% / 6 h; 65% / 24 h; 20%) (Table 3).
The incidence of hoarseness at 1, 6, and 24 h after tracheal extubation was significantly lower in group D2 (1 h; 16%, P = 0.001 / 6 h; 8%, P < 0.001 / 24 h; 0%, P = 0.001) than group P (1 h; 49% / 6 h; 59% / 24 h; 33%) (Table 4).
There was no significant difference in the incidence of cough among the three groups (Table 5).
The incidence of severity scores of POST is described in Table 6. There were less number of patients in the groups D1 and D2 than group P suffering from minimal grade of POST at 6 h after extubation and moderate grade of POST at 1, 24 h after extubation (P < 0.05) (Table 6). There was no significant difference in the incidence of severity scores of hoarseness and cough among the three groups.
The result of this study showed that dexamethasone given before the induction of anesthesia decreased the incidence of POST and hoarseness (in group D2) at 1, 6, and 24 h after tracheal extubation compared with that in the group P. Less number of patients reported moderate grade of POST at 1, 24 h after extubation in groups D1 and D2 compared with group P.
Park et al. [17] reported that the prophylactic use of 0.1 mg/kg and 0.2 mg/kg of dexamethasone significantly decreased the incidence of sore throat at 1 h after extubation by 22% and 42%, respectively, and dexamethasone 0.2 mg/kg decreased the incidence of sore throat at 24 h after extubation by 30%. Bagchi et al. [13] found that the prophylactic intravenous dexamethasone in a dose of 0.2 mg/kg reduced the incidence of sore throat at 1 h after extubation by 30% and at 6 h after extubation by 24%. Based on these previous studies, this study set the dose of dexamethasone in group D1 and group D2 as 0.1 mg/kg and 0.2 mg/kg, respectively.
The factors which are known to affect the prevalence of postoperative sore throat include difficult intubation procedure or repeated attempts, larger diameter of the tracheal tube, displacement of the endotracheal tube during the surgery, bucking on the tube, and excessive oral suctioning during extubation [18]. The pathological cause of sore throat is thought to be an aseptic inflammatory process because of the irritation of the pharyngeal mucosa during laryngoscopy, the damage of tracheal mucosa by the cuff of the endotracheal tube, and the trauma to tissues during the processes of intubation and extubation [171920].
Postoperative hoarseness is the result of at least some degree of laryngeal injury. Several risk factors for laryngeal injury and postoperative hoarseness have been identified, including endotracheal tube size, cuff design, cuff pressure, movement of the tube, physical trauma, duration of intubation as well as demographic factors such as sex or even the type of surgery [21].
The prophylactic use of steroids reduced the incidence of sore throat and hoarseness during recovery, probably by modifying the inflammatory process caused by tissue injury. This antiinflammatory process includes inhibition of leukocyte migration to the site of inflammation and inhibition of release of cytokines probably by maintaining cellular integrity. Fibroblast proliferation may also be inhibited [17182022]. Dexamethasone can reduce the synthesis of inflammatory mediators, prostaglandins, and leukotrienes by inhibiting phospholipase A2 through production of calcium-dependent phospholipid-binding proteins called annexins [23] and by inhibition of cyclooxygenase 2 during inflammation [24].
Potential side effects of dexamethasone include increased susceptibility of infection, hyperglycemia, delayed wound healing, adrenal suppression, and a vascular necrosis of the hip or other joints. Although a single dose of dexamethasone is considered safe, further studies with longer follow-ups are required [25].
The position change from supine to prone can cause the change of cuff pressure and the displacement of endotracheal tube [16]. In a recent study, endotracheal tube displacement was occurred in 91.7% of patients after the supine-to-prone position change; of these, 48% of patients' endotracheal tube moved more than 10 mm and endotracheal tube cuff pressure was changed in 86.3% of patients [15]. The changes in cuff pressure and tube displacement are the factors that affect the incidence of POST, hoarseness, and cough [67]. Therefore, higher incidence and severity of POST, hoarseness, and cough were expected in prone position surgery compared with supine position surgery.
In this study, the incidence of POST in the group P was 67 and 65% at 1 and 6 h after tracheal extubation, respectively. These incidence figures are somewhat higher than those in previous reports [1314] of supine surgery patients. The incidence of hoarseness in the group P after extubation was also higher than that in the other study [1314]. In this study, the change in patient position was performed two times in order to achieve the prone position and recovery of anesthesia at termination of surgery. In addition, prone position was maintained during the operation. These factors might be thought to contribute the incidence of sore throat and hoarseness. However, there were the difference of intubation time between this study and the other studies [1314]. Therefore, many studies would be required to find out the relationship between prone position and POST.
The limitation of this study was that the fiberoptic bronchoscope was not used to assess tissue damage and displacement of endotracheal tube. Sore throat, hoarseness, and cough could not be assessed objectively, and there were inter-individual variations; therefore, a chance of bias exists. This study was not designed to perform an additional follow-up beyond 24 h as the process of acute inflammation usually peaks by 24 h.
In conclusion, prophylactic intravenous dexamethasone 0.1 and 0.2 mg/kg significantly reduced the incidence of postoperative sore throat and dexamethasone 0.2 mg/kg decreased the incidence of hoarseness in patients undergoing prone position
surgery.
References
1. Higgins PP, Chung F, Mezei G. Postoperative sore throat after ambulatory surgery. Br J Anaesth. 2002; 88:582–584. PMID: 12066737.

2. Macario A, Weinger M, Truong P, Lee M. Which clinical anesthesia outcomes are both common and important to avoid? The perspective of a panel of expert anesthesiologists. Anesth Analg. 1999; 88:1085–1091. PMID: 10320175.

3. Estebe JP, Dollo G, Le Corre P, Le Naoures A, Chevanne F, Le Verge R, et al. Alkalinization of intracuff lidocaine improves endotracheal tube-induced emergence phenomena. Anesth Analg. 2002; 94:227–230. PMID: 11772834.

4. Christensen AM, Willemoes-Larsen H, Lundby L, Jakobsen KB. Postoperative throat complaints after tracheal intubation. Br J Anaesth. 1994; 73:786–787. PMID: 7880666.

5. Maruyama K, Sakai H, Miyazawa H, Toda N, Iinuma Y, Mochizuki N, et al. Sore throat and hoarseness after total intravenous anaesthesia. Br J Anaesth. 2004; 92:541–543. PMID: 14766717.

6. Mandøe H, Nikolajsen L, Lintrup U, Jepsen D, Mølgaard J. Sore throat after endotracheal intubation. Anesth Analg. 1992; 74:897–900. PMID: 1595921.
7. McHardy FE, Chung F. Postoperative sore throat: cause, prevention and treatment. Anaesthesia. 1999; 54:444–453. PMID: 10995141.

8. Baxendale BR, Vater M, Lavery KM. Dexamethasone reduces pain and swelling following extraction of third molar teeth. Anaesthesia. 1993; 48:961–964. PMID: 8250191.

9. Elhakim M, Ali NM, Rashed I, Riad MK, Refat M. Dexamethasone reduces postoperative vomiting and pain after pediatric tonsillectomy. Can J Anaesth. 2003; 50:392–397. PMID: 12670818.

10. Schmelzeisen R, Frölich JC. Prevention of postoperative swelling and pain by dexamethasone after operative removal of impacted third molar teeth. Eur J Clin Pharmacol. 1993; 44:275–277. PMID: 8491244.

11. Wang JJ, Ho ST, Lee SC, Liu YC, Liu YH, Liao YC. The prophylactic effect of dexamethasone on postoperative nausea and vomiting in women undergoing thyroidectomy: a comparison of droperidol with saline. Anesth Analg. 1999; 89:200–203. PMID: 10389804.
12. Ruangsin S, Wanasuwannakul T, Pattaravit N, Asim W. Effectiveness of a preoperative single dose intravenous dexamethasone in reducing the prevalence of postoperative sore throat after endotracheal intubation. J Med Assoc Thai. 2012; 95:657–660. PMID: 22994024.
13. Bagchi D, Mandal MC, Das S, Sahoo T, Basu SR, Sarkar S. Efficacy of intravenous dexamethasone to reduce incidence of postoperative sore throat: A prospective randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2012; 28:477–480. PMID: 23225928.

14. Thomas S, Beevi S. Dexamethasone reduces the severity of postoperative sore throat. Can J Anaesth. 2007; 54:897–901. PMID: 17975234.

15. Minonishi T, Kinoshita H, Hirayama M, Kawahito S, Azma T, Hatakeyama N, et al. The supine-to-prone position change induces modification of endotracheal tube cuff pressure accompanied by tube displacement. J Clin Anesth. 2013; 25:28–31. PMID: 23391343.

16. Kim D, Jeon B, Son JS, Lee JR, Ko S, Lim H. The changes of endotracheal tube cuff pressure by the position changes from supine to prone and the flexion and extension of head. Korean J Anesthesiol. 2015; 68:27–31. PMID: 25664152.

17. Park SH, Han SH, Do SH, Kim JW, Rhee KY, Kim JH. Prophylactic dexamethasone decreases the incidence of sore throat and hoarseness after tracheal extubation with a double-lumen endobronchial tube. Anesth Analg. 2008; 107:1814–1818. PMID: 19020122.

18. Scuderi PE. Postoperative sore throat: more answers than questions. Anesth Analg. 2010; 111:831–832. PMID: 20870978.
19. Huang YS, Hung NK, Lee MS, Kuo CP, Yu JC, Huang GS, et al. The effectiveness of benzydamine hydrochloride spraying on the endotracheal tube cuff or oral mucosa for postoperative sore throat. Anesth Analg. 2010; 111:887–891. PMID: 20581162.

20. Canbay O, Celebi N, Sahin A, Celiker V, Ozgen S, Aypar U. Ketamine gargle for attenuating postoperative sore throat. Br J Anaesth. 2008; 100:490–493. PMID: 18310675.

21. Mencke T, Echternach M, Kleinschmidt S, Lux P, Barth V, Plinkert PK, et al. Laryngeal morbidity and quality of tracheal intubation: a randomized controlled trial. Anesthesiology. 2003; 98:1049–1056. PMID: 12717124.
22. Liu J, Zhang X, Gong W, Li S, Wang F, Fu S, et al. Correlations between controlled endotracheal tube cuff pressure and postprocedural complications: a multicenter study. Anesth Analg. 2010; 111:1133–1137. PMID: 20736432.
23. Yao XL, Cowan MJ, Gladwin MT, Lawrence MM, Angus CW, Shelhamer JH. Dexamethasone alters arachidonate release from human epithelial cells by induction of p11 protein synthesis and inhibition of phospholipase A2 activity. J Biol Chem. 1999; 274:17202–17208. PMID: 10358078.

24. Lubenow TR, Ivankovich D, McCarthy RJ. Management of acute postoperative pain. In : Barash PG, Cullen BF, Stoelting RK, editors. Clinical Anesthesia. Philadelphia: Lippincott Williams & Wilkins Inc.;2001. p. 1403–1434.
25. Elhakim M, Ali NM, Rashed I, Riad MK, Refat M. Dexamethasone reduces postoperative vomiting and pain after pediatric tonsillectomy. Can J Anaesth. 2003; 50:392–397. PMID: 12670818.

Table 1
Scoring System for Assessment of Sore Throat, Hoarseness and Cough
Table 2
Patient Characteristics
Table 3
Incidences of Sore Throat among the Groups after Tracheal Extubation
Table 4
Incidence of Hoarseness among the Groups after Tracheal Extubation
Table 5
Incidence of Cough among the Groups after Tracheal Extubation
|
Group P (n = 49) |
Group D1 (n = 48) |
Group D2 (n = 50) |
P values P vs. D1 vs. D2 |
|
|---|---|---|---|---|
| 1 h | 5 (10%) | 3 (6%) | 0 (0%) | 0.078 |
| 6 h | 2 (4%) | 0 (0%) | 1 (2%) | 0.364 |
| 24 h | 4 (8%) | 2 (4%) | 0 (0%) | 0.122 |




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download