Abstract
Micro-emboli have been reported to occur commonly during arthroscopic surgery, which is frequently performed as an orthopedic surgical procedure. We here report a patient who experienced unilateral postoperative visual loss after a hip arthroscopy using irrigation fluid in the supine position without any evidence of external compression to either eye throughout the surgical procedure. Retinal fundoscopy suggested that the patient had central retinal artery occlusion, one of the causes of the postoperative visual loss. This case suggests that arthroscopic surgery may pose a substantial risk for paradoxical air embolism, such as central retinal artery occlusion, and suggests the need to prevent the entry of micro-air bubbles during such a type of surgery.
Go to : 
Postoperative visual loss (POVL) rarely develops, but is associated with unfavorable consequences including permanent loss of vision [1]. POVL can be caused by central retinal artery occlusion (CRAO), ischemic optic neuropathy, or cortical blindness [1234]. It poses high risk when blood flow and subsequent oxygen delivery to eyes, including blood pressure and hematocrit level, decrease during the perioeprtive period [3567].
Micro-emboli are commonly generated during arthroscopic surgery, and are generally of clinical insignificance [891011]. Such micro-emboli may, however, contribute to the development of a paradoxical embolism, if an intra-cardiac shunt, such as a patent foramen ovale, is observed in the surgical patients [12].
We here report a patient who experienced unilateral POVL caused by CRAO following a hip arthroscopy performed in the supine position throughout the surgery. A CRAO might be speculated to be associated with micro-emboli formed during arthroscopic surgery.
A 52-year-old female patient (height 160 cm and weight 60 kg) was scheduled for emergent hip arthroscopic synovectomy and partial labral resection due to acute hematogenous osteomyelitis with abscess. She had been treated with thiazide and angiotensin receptor blocker to control hypertension. A preoperative electrocardiogram indicated a normal sinus rhythm. Preoperative hematocrit was 29.8% and other laboratory findings were within the normal ranges. She had been NPO for 14.5 hours before surgery.
Upon arriving in the operating room, an initial systolic/diastolic blood pressure (BP) of 124/99 mmHg, heart rate (HR) of 90 beats/min, and oxygen saturation of 100% at room air were observed. Anesthetic induction was performed using 300 mg of thiopental sodium and 40 mg of rocuronium, followed by tracheal intubation. Anesthesia was maintained using 6.0–7.0 vol% of desflurane with 50% of oxygen using medical air. The surgery was performed while the patient was in the supine position. After surgical draping, the patient's face was observed by the attending anesthesiologist to be free from any external compression throughout the surgery.
During the surgery, the systolic and diastolic BP were kept within the ranges of 95–110 mmHg and 60–80 mmHg, respectively. A normal sinus rhythm was sustained through the surgery, with a HR of 85 beats/ min. The end-tidal carbon dioxide was maintained within the range of 30–35 mmHg. The surgery lasted for 256 minutes, with the administration of Ringer's lactate solution (800 ml). A 3000 ml normal saline for irrigating the arthroscopic field was delivered by an arthroscopic pump (24k® Fluid Management System, ConMED, Largo, FL, USA). At the end of the surgery, the patient was confirmed to be fully awake and was delivered to the post anesthetic care unit (PACU).
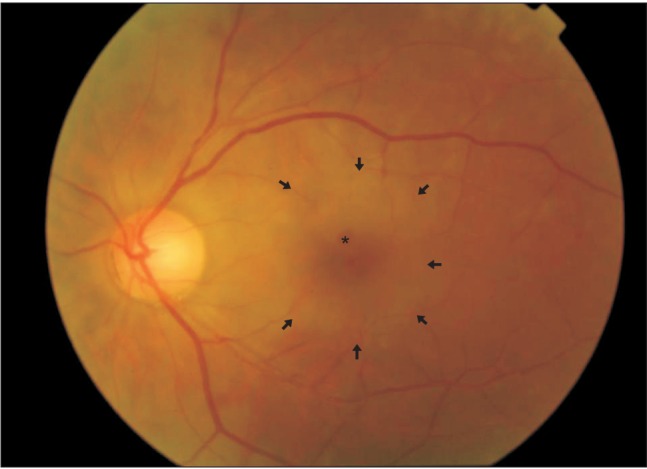
One hour after arriving at the PACU, she complained of visual impairment in her left eye, saying that she could not detect any light with her left eye. A hematology evaluation indicated a hematocrit value of 25.1%. Immediately after being notified as regard to her visual problem, the patient was referred to an ophthalmologist and diagnosed as most likely having CRAO (Fig. 1). At that time, intraocular pressure (IOP) was 19 mmHg in the left eye that might be caused by swelling of the surrounding tissue. Paracentesis in the anterior chamber of the left eye was performed to increase perfusion pressure to retinal artery perfusion, resulting in decreased IOP to 15 mmHg in the left eye. Three hours after paracentesis, her visual impairment had slightly improved and she could distinguish the outline of objects. On postoperative day 2, the patient was treated with hyperbaric oxygen therapy to improve oxygen delivery, combined with topical medications every day for 1 week. On postoperative day 4, brain magnetic resonance imaging revealed a normal optic pathway and transthoracic echocardiography showed no intra-cardiac shunt and no thrombus. Her visual acuity in the left eye had gradually recovered to 0.8 on postoperative day 5, at which point the IOP was 10 mmHg in the left eye. She was discharged with a visual acuity of 0.8 and IOP of 7 mmHg in the left eye on postoperative day 29.
Go to : 
We present a patient who experienced an unilateral POVL following hip arthroscopic surgery in the supine position. An unilateral POVL in our case was confirmed to be caused by CRAO in fundoscopic examination.
CRAO is most commonly associated with emboli and direct globe compression [2]. Most cases that reported an embolization described embolic materials from intravascular injections, from the surgical field, and from cardiopulmonary bypass equipment during cardiac surgery [1]. All CRAO cases shows unilateral loss of vision and can be diagnosed by fundoscopic examination of typical findings, such as macular or retinal edema, a cherry-red spot, or attenuated retinal vessels [3]. For acute management of CRAO, attempts to increase the blood oxygen content, to reduce IOP below 15 mmHg and thus increase the retinal artery perfusion, and to reduce the retinal edema have been made [13]. Most patients who developed CRAO postoperatively show unfavorable outcomes, despite prompt and appropriate managements [1].
In our present case, hip arthroscopic surgery was performed while the patient was in the supine position. This enabled us to confirm that the patient's eye was free of any external pressure throughout the surgery. When considering the unilaterality of visual loss, ischemia induced by a specific artery was suspected to contribute to the patient's symptoms. Finally, CRAO was confirmed by fundoscopic examination. Air emboli, which have been known to commonly develop during arthroscopic surgery [891011], can result in CRAO, likely through an undetected intracardiac shunt [14]. The potential risk for fatal venous air embolism in arthroscopic procedures has been previously reported [9]. In addition, some clinical factors, including the patient's medical history of hypertension, a long duration of surgery over 4 hours, and a low perioperative hematocrit level of 25.1%–29.8%, may have aggravated the ischemia-related symptoms and signs in our case.
It has been reported that the pressure gradient between the surgical site and the right atrium is a critical factor in the volume and rate of air entry during arthroscopic surgery [9]. To decrease the gradient between the operative site and right atrium, it is important to adequately maintain the patient's volume status. We think that the intravascular volume status in our present patient might not be sufficiently maintained, when considering the duration of NPO time and of surgery and the total amount of administered fluid. This condition may subsequently precipitate an air embolism during surgery. Vigilant monitoring and management to optimize the intravascular volume status may thus be necessary during arthroscopic surgery. In addition, it is also recommended to remove air from the irrigation bags and prime the arthroscopic tubing to prevent air embolism [89].
In conclusion, we have presented a case of unilateral visual loss after hip arthroscopic surgery performed with the patient in the supine position. Our case suggests that CRAO can be caused by a paradoxical air embolism during arthroscopic surgery when using irrigation fluid. It is necessary to adequately manage the patient's volume status and surgical irrigation bag to prevent clinically significant paradoxical air embolism during arthroscopic surgery.
Go to : 
References
1. Roth S. Postoperative visual loss. In : Miller RD, editor. Miller's Anesthesia. 7th ed. Philadelphia: Churchill Livingstone/Elsevier;2009. p. 2821–2841.
2. Lee LA. Perioperative visual loss and anesthetic management. Curr Opin Anaesthesiol. 2013; 26:375–381. PMID: 23614957.

3. Lee LA, Roth S, Posner KL, Cheney FW, Caplan RA, Newman NJ, et al. The American Society of Anesthesiologists Postoperative Visual Loss Registry: analysis of 93 spine surgery cases with postoperative visual loss. Anesthesiology. 2006; 105:652–659. PMID: 17006060.
4. Roth S. Perioperative visual loss: what do we know, what can we do? Br J Anaesth. 2009; 103(Suppl 1):i31–i40. PMID: 20007988.

5. Dunker S, Hsu HY, Sebag J, Sadun AA. Perioperative risk factors for posterior ischemic optic neuropathy. J Am Coll Surg. 2002; 194:705–710. PMID: 12081060.
6. Katz DA, Karlin LI. Visual field defect after posterior spine fusion. Spine (Phila Pa 1976). 2005; 30:E83–E85. PMID: 15682002.

7. Postoperative Visual Loss Study Group. Risk factors associated with ischemic optic neuropathy after spinal fusion surgery. Anesthesiology. 2012; 116:15–24. PMID: 22185873.
8. Austin L, Zmistowski B, Tucker B, Hetrick R, Curry P, Williams G Jr. Commercial liquid bags as a potential source of venous air embolism in shoulder arthroscopy. J Bone Joint Surg Am. 2010; 92:2110–2114. PMID: 20686050.

9. Austin LS, VanBeek C, Williams GR. Venous air embolism: an under-recognized and potentially catastrophic complication in orthopaedic surgery. J Shoulder Elbow Surg. 2013; 22:1449–1454. PMID: 24054311.

10. Pandey V, Varghese E, Rao M, Srinivasan NM, Mathew N, Acharya KK, et al. Nonfatal air embolism during shoulder arthroscopy. Am J Orthop (Belle Mead NJ). 2013; 42:272–274. PMID: 23805421.
11. Zmistowski B, Austin L, Ciccotti M, Ricchetti E, Williams G Jr. Fatal venous air embolism during shoulder arthroscopy: a case report. J Bone Joint Surg Am. 2010; 92:2125–2127. PMID: 20810863.
12. Hagen PT, Scholz DG, Edwards WD. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc. 1984; 59:17–20. PMID: 6694427.

13. Varma DD, Cugati S, Lee AW, Chen CS. A review of central retinal artery occlusion: clinical presentation and management. Eye (Lond). 2013; 27:688–697. PMID: 23470793.

14. Marriott K, Manins V, Forshaw A, Wright J, Pascoe R. Detection of right-to-left atrial communication using agitated saline contrast imaging: experience with 1162 patients and recommendations for echocardiography. J Am Soc Echocardiogr. 2013; 26:96–102. PMID: 23072711.
Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download