Abstract
A bronchial blocker (BB) is preferred for lung separation in patients with difficult airways. However, BBs, unlike double-lumen tubes, must be placed in the bronchus of the lung being operated on, hence can be damaged by surgical manipulation. Intubation was unexpectedly difficult in this male patient, so a Coopdech BB was placed in the right mainstem bronchus through a single-lumen tracheoscopic ventilation tube for a thoracoscopic right upper lobectomy. During the bronchial resection, however, the distal tip of the BB was transected and pinched in the staple line, so the staple line was partially opened, and the BB was withdrawn into the trachea. The opened bronchial stump was sutured manually under apnea without conversion to an open thoracotomy, and there was no significant air leakage through the suture line. This case underlines the importance of frequently evaluating the position of a BB during lung surgery.
Double-lumen endobronchial tubes (DLTs) are the airway devices most commonly used for one-lung ventilation in thoracic surgery. However, DLTs are rigid and have large external diameters, and intubation with a DLT requires more complicated manipulation than with a single-lumen endotracheal tube (SLT). Therefore, in order to perform one-lung ventilation (OLV) in patients with difficult airways, it is safer to use a SLT with an independent bronchial blocker (BB) to achieve endotracheal intubation and lung isolation compared to using a DLT [1,2]. However, since BBs should be placed within the mainstem bronchus of the operative lung, the BB can be dislodged into the trachea or lobar bronchi during the surgical procedure. Consequently, the BB might not only interfere with the procedure, but it might also be damaged during surgical resection of the bronchus. We report a case involving transection of the BB tip during resection of the right upper lobar bronchus in video-assisted thoracoscopic surgery.
A 69-year-old male (height 160 cm, weight 56 kg) was diagnosed with non-small cell lung carcinoma in the right upper lobe (RUL) and scheduled for a right upper lobectomy under video-assisted thoracoscopic surgery. Preoperatively, the patient had no findings suggesting a difficult airway. The Mallampati grade was Class II, with normal mouth opening, neck extension, and thyromental distance. The chest X-ray and computed tomography showed no anatomical abnormalities in the trachea or mainstem bronchi. The internal diameter of the left mainstem bronchus was 12.5 mm; thus, a 37 Fr left-sided DLT was selected for lung separation.
The patient arrived at the operating room without premedication. After preoxygenation with 100% oxygen, anesthesia was induced by the target-controlled infusion of propofol and remifentanil, starting at effect site concentrations of 4 µg/ml and 4 ng/ml, respectively. After loss of consciousness, manual bagmask ventilation was achieved without difficulty, and 50 mg rocuronium were administered for neuromuscular blockade. After 3 min, we attempted endotracheal intubation with a 37 Fr left-sided DLT using a Macintosh no.4 laryngoscope blade. However, unexpectedly, the direct laryngoscopic view showed Cormack-Lehane grade IIIb, even though he had no physical attributes that predicted difficult intubation during the preoperative airway evaluation. The epiglottis was only just visible, and additional manipulations, such as pressing the cricoid cartilage or jaw thrust by two assistants, did not improve the direct laryngoscopic glottic view. Although we tried to insert the DLT into the glottis under the epiglottis without obtaining sufficient glottic exposure, intubation failed. Fortunately, however, manual ventilation was adequate, and the oxygen saturation by pulse oximetry was maintained at 100% between intubation attempts.
Instead of a DLT, we decided to use a SLT to secure the airway and a BB to achieve lung separation. A tracheoscopic ventilation tube (TVT; VivaSight™-SL, ETView Ltd, Misgav, Israel) was selected to improve the poor glottic view (Fig. 1). A stylet was inserted into a TVT with a 7.5 mm internal diameter (10.5 mm external diameter), and the distal portion of the TVT was flexed in a hockey-stick shape. The TVT was connected to a monitoring device with a 5.4 × 7 cm screen. After direct laryngoscopy with a Macintosh no.4 blade, the TVT was inserted into the oropharynx, and then full glottic opening was visible on the TVT monitor. Using the real-time image on the monitor, the TVT was inserted into the glottis. After removing the stylet, the TVT was positioned at the level of the mid-trachea. Then, a Coopdech BB (Daiken Medical Co. Ltd, Osaka, Japan) was inserted through the TVT and placed in the right mainstem bronchus (RMB) under the view of the TVT monitor. The BB cuff was positioned just below the carina, so as not to obstruct the RUL bronchus (Fig. 2). The BB position was monitored continuously while changing the patient's position and then readjusted after the patient was in the left lateral decubitus position. Complete collapse of the right lung was verified by the thoracoscopic view, and OLV was performed with a tidal volume of 6-8 ml/kg predicted body weight and a positive end-expiratory pressure of 5 cmH2O. The respiratory rate and inspired oxygen fraction were adjusted to obtain arterial tensions of 40-45 mmHg for CO2 and > 100 mmHg for oxygen.
The surgery proceeded uneventfully before the bronchial resection. After dissecting the RUL bronchus, it was transected using a surgical stapler (Endo GIA™, Covidien, Mansfield, MA, USA). However, when checking the transected bronchial stump, the surgeon found that the distal tip of the BB had been included in the staple line (Fig. 3). Since the BB tip was firmly trapped in the staple line, the BB could not be withdrawn manually. Therefore, the surgeon removed some staples from the bronchial stump to free the BB tip, and then the BB was withdrawn carefully and left in the trachea considering the risk of its reinsertion into the RUL bronchus. For right lung collapse, thus, the surgeon manually sutured the partially opened stump under apnea without conversion to open thoractomy. The repair took about 2 min, and the oxygen saturation remained above 95% during apnea. The separated distal tip of the BB was found in the staple line of the RUL surgical specimen (Fig. 4). No endobronchial defect was seen in the sutured line on bronchoscopic evaluation, and no significant air leak was detected during a leakage test of the operative lung at a positive pressure of 25 cmH2O. A chest tube was inserted to check postoperative bleeding and air leakage.
The operation was finished without any other adverse events, the patient was transferred to the intensive care unit for close observation. No air leakage was found through the chest tube. A bronchoscopic evaluation was done on the 2nd postoperative day and there were no problems in the repaired lesion. The patient was discharged on the 7th postoperative day without complications.
Preoperatively, patients requiring OLV should be evaluated for the possibility of a difficult airway. This patient had no specific findings suggesting a difficult airway during the preoperative airway evaluation, and manual bag-mask ventilation was adequate after muscle relaxation, so we did not anticipate a difficult intubation. Although video laryngoscopes increase the visualization of the epiglottis and vocal cords, thereby facilitating intubation with a DLT [3], this institution lacked a video laryngoscope. For bronchoscopy-guided intubation of a DLT, only a limited part of the fiberoptic bronchoscope (FOB) is available for manipulation owing to the length of the DLT. In addition, the large external diameter and rigidity of the DLT make it awkward to pass the glottis through the FOB [4]. Therefore, when tracheal intubation is unfeasible with a DLT, a SLT might be preferred to secure the airway. Moreover, a single-lumen TVT is superior to a plain SLT for intubation of a patient with a poor view of the glottic opening [5]. In this case, intubation using a DLT via direct laryngoscopy failed despite several attempts, while the TVT was successfully inserted into the glottis on the first attempt.
After the airway is secured with a SLT, it can be replaced by a DLT using an airway exchange catheter for the subsequent lung separation. However, there are significant risks of failure during tube exchange and associated airway injury with its use [6]. The failure rate is higher when replacing a SLT with a DLT, as compared with changing from a SLT to a SLT or a DLT to a SLT. In addition, although OLV can be achieved with endobronchial intubation using a SLT, an extra-long SLT must be placed in the mainstem bronchus, and suction of the contralateral bronchus or conversion between two- and one-lung ventilation are impracticable. Therefore, using an independent BB is preferred for lung isolation when a SLT has been placed in the trachea.
If a BB is inserted via a SLT, a FOB is required for correct positioning of the BB in the desired mainstem bronchus. However, the position of a BB inserted through a TVT can be adjusted without a FOB, because the TVT has a video-camera near its distal aperture. The distal tip of the TVT is usually placed at mid-trachea, so the lower portion and carina of the trachea and openings of the mainstem bronchi can be inspected, while the lobar bronchi and bronchial carinas are invisible through the TVT. Therefore, we could not grossly examine the precise position of the RUL bronchial orifice. In general, however, because the RMB is short, the BB cuff was placed in the RMB as close to the carina as possible, so as not to obstruct the RUL bronchus. Subsequently, left OLV and collapse of the RUL were achieved without any problems until resection of the RUL bronchus.
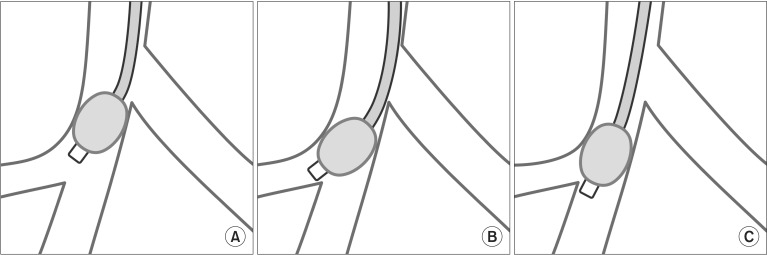
Preoperatively, although the internal diameter of the left mainstem bronchus is commonly measured on chest computed tomography to select an appropriately sized left-sided DLT [7], the other tracheobronchial anatomical features, such as the internal diameter of the RMB or length of the mainstem bronchi, are frequently overlooked. However, as shown in this case, intubation with a left-sided DLT might sometimes fail, so alternative techniques should be considered for securing the airway and for lung separation. Therefore, in patients who are scheduled for thoracic surgery requiring OLV, the entire anatomy of the tracheobronchial tree should be evaluated thoroughly from preoperative airway imaging examinations. In addition, although the BB was positioned correctly in the mainstem bronchus before surgery, it can be displaced by a positional change of the patient or airway manipulation during surgery. Moreover, because the distal part of a Coopdech BB is angulated to facilitate its insertion into the desired mainstem bronchus, it might have a greater risk of being dislodged into the RUL bronchus rather than into the bronchus intermedius (Fig. 5). In this case, the patient's RMB was 2.5 cm long, which was nearly identical to the distance between the distal tip and proximal border of the BB cuff (Fig. 6). Thus, before resection of the RUL bronchus, withdrawing the BB in the trachea would be required to prevent the complication as in this case [8]. Moreover, At the start of OLV, the three lobes of the right lung were collapsed completely, so the distal tip of the BB seemed to have been positioned properly in the RMB, outside the RUL bronchus. However, the BB tip might have been dislodged slightly into the RUL bronchus by surgical manipulation of the right bronchus, and it was consequently cut off during resection of the RUL bronchus. Therefore, we should remember that even though a BB has been placed correctly in the mainstem bronchus preoperatively, its position might change, so it should be frequently checked intraoperatively. Furthermore, after the stapler has been placed with its jaws closed but before permanently resecting the bronchus, anesthesiologists should attempt to move the BB freely, so as to exclude its trapping by the stapler [9]. The role of anesthesiologists would be more important in thoracoscopic surgery rather than in open thoracotomy, because the surgeon could not check the precise position of the BB tip manually under the thoracoscopy.
In conclusion, a BB combined with a SLT can be used preferentially over a DLT in patients who require OLV and have a difficult airway. Anesthesiologists should consider the possibility of BB dislodgement during surgical manipulation and ensure that the bronchus is clear before performing the bronchial resection by moving the BB slightly while communicating with the thoracic surgeons. In addition, as well as constant vigilance regarding the BB, obtaining meticulous information on the airway anatomy should precede successful OLV to avoid potentially hazardous mishaps.
References
1. Campos JH. Lung isolation techniques for patients with difficult airway. Curr Opin Anaesthesiol. 2010; 23:12–17. PMID: 19752725.

2. Campos JH. Which device should be considered the best for lung isolation: double-lumen endotracheal tube versus bronchial blockers. Curr Opin Anaesthesiol. 2007; 20:27–31. PMID: 17211163.

3. Hernandez AA, Wong DH. Using a Glidescope for intubation with a double lumen endotracheal tube. Can J Anaesth. 2005; 52:658–659. PMID: 15983163.

4. Ransom ES, Carter SL, Mund GD. Univent tube: a useful device in patients with difficult airways. J Cardiothorac Vasc Anesth. 1995; 9:725–727. PMID: 8664468.

5. Heitz JW, Shum PP, Grunwald Z. Use of a tracheoscopic ventilation tube for endotracheal intubation in the difficult airway. J Clin Anesth. 2011; 23:403–406. PMID: 21723719.

6. McLean S, Lanam CR, Benedict W, Kirkpatrick N, Kheterpal S, Ramachandran SK. Airway exchange failure and complications with the use of the cook airway exchange catheter(R): a single center cohort study of 1177 patients. Anesth Analg. 2013; 117:1325–1327. PMID: 24257382.
7. Hannallah M, Benumof JL, Silverman PM, Kelly LC, Lea D. Evaluation of an approach to choosing a left double-lumen tube size based on chest computed tomographic scan measurement of left mainstem bronchial diameter. J Cardiothorac Vasc Anesth. 1997; 11:168–171. PMID: 9105987.

8. Benumof JL, Partridge BL, Salvatierra C, Keating J. Margin of safety in positioning modern double-lumen endotracheal tubes. Anesthesiology. 1987; 67:729–738. PMID: 3674473.

9. Soto RG, Oleszak SP. Resection of the Arndt Bronchial Blocker during stapler resection of the left lower lobe. J Cardiothorac Vasc Anesth. 2006; 20:131–132. PMID: 16458238.

Fig. 1
The overall appearance (A) and distal orifice (B) of the VivaSight™-SL tracheoscopic ventilation tube.
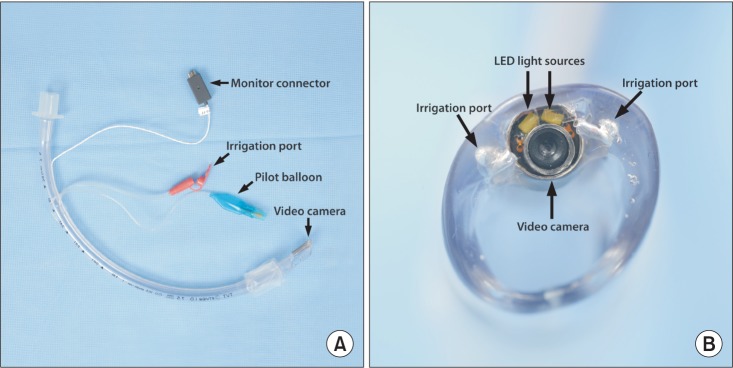
Fig. 2
View of the tracheoscopic ventilation tube. Although the bronchial blocker was appropriately positioned in the right mainstem bronchus just below the carina, its distal tip was invisible.
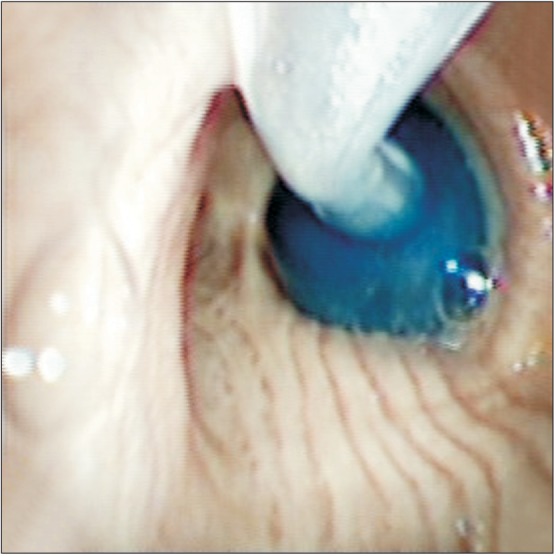
Fig. 3
The distal tip of the Coopdech bronchial blocker in the surgical staple line of the right upper lobar bronchial stump.

Fig. 4
The transected distal tip of the Coopdech bronchial blocker found in the surgical specimen of the right upper lobe.
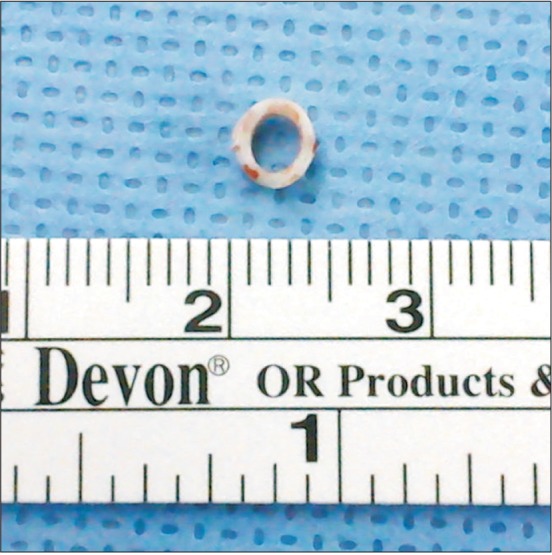
Fig. 5
Schematic diagrams of a Coopdech bronchial blocker placed in the right bronchus. A Coopdech bronchial blocker is angulated distally. Consequently, even if it has been placed in the right mainstem bronchus (A) properly, it might more likely be dislodged into the right upper lobar bronchus (B) than into the bronchus intermedius (C) during surgical manipulation of the right bronchus.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download