This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Although Lightwand and Glidescope have both shown high success rates for intubation, there has been no confirmation as to which device is most effective for difficult endotracheal intubation. We compared the Glidescope and Lightwand devices in terms of duration of intubation and success rate at the first attempt in a simulated difficult airway situation.
Methods
Fifty-eight patients were randomized to undergo tracheal intubation with either the Glidescope (Glidescope group, n = 29) or the Lightwand (Lightwand group, n = 29). All patients were fitted with a semi-hard cervical collar in order to simulate a difficult airway, and intubation was attempted with the assigned airway device. The data collected included the rate of successful endotracheal intubation, the number of attempts required, the duration of the intubation, as well as the interincisor distance, hemodynamic variables, and adverse effects.
Results
There was no difference between Glidescope group (92.6%) and Lightwand group (96.4%) in terms of success rate for the first attempt at intubation. The duration of successful intubation for the first tracheal intubation attempt was significantly longer in Glidescope group than in Lightwand group (46.9 sec vs 29.5 sec, P = 0.001). All intubations were completed successfully within two intubation attempts. The incidence of hypertension was significantly higher in Glidescope group than in Lightwand group (51.9% vs 17.9%, P = 0.008).
Conclusions
In a simulated difficult airway situation, endotracheal intubation using Lightwand yielded a shorter duration of intubation and lower incidence of hypertension than when using Glidescope.
Keywords: Airway management, Intubation, Laryngoscopes, Light, Transillumination
Introduction
The management of a difficult airway is an important part of clinical anesthesia and difficulty with intubation is the most common cause of severe airway complications during general anesthesia [
1]. The Glidescope and Lightwand devices are both used to facilitate intubation in the event of difficult airways [
2]. Glidescope is an airway device with a 60-degree curved blade and digital camera at its tip. It can improve the view of the glottis and is therefore beneficial in patients with a difficult airway [
3]. Lightwand is a stick featuring a light bulb at its tip, which can be used to perform a tracheal tube intubation blindly after confirmation that the bulb has passed the glottis and is illuminating the anterior neck clearly [
4].
Because of its large size, Glidescope can present difficulties when inserting it in the mouth and manipulating it to find the vocal cords, in the case of patients presenting problems with mouth opening and neck extension. The tracheal tube entry into the vocal cord can also be difficult due to Glidescope occupying the space of the oral cavity. On the other hand, Lightwand is a small device and the degree of its tip bent can be modulated, making it easier to handle in the case of a patient with difficulty in mouth opening and neck extension. The aim of this study was to compare Glidescope and Lightwand for endotracheal intubation in a simulated difficult airway situation.
Materials and Methods
This study was approved by our hospital Institutional Review Board. Fifty-eight patients who were scheduled to undergo elective surgery requiring general anesthesia and tracheal intubation agreed to participate in the present study. All intubations were completed by one researcher with proven experience of at least 30 successful intubations with both devices.
The subjects were patients of ASA physical status grade 1 or 2, aged 20-60 years, who were scheduled to undergo elective surgery and tracheal intubation. Patients were excluded according to the following criteria:
Risk of dental injury or aspiration
-
Functional airway problem
(i.e., asthma, burn)
-
Anatomical airway problem
(i.e., intraoral, pharyngeal, laryngeal or cervical masses, history of surgery in these regions)
History of difficult tracheal intubation
Body mass index (BMI) greater than 30 kg/m2
Patients were randomized into 2 groups of 29 following a prepared randomization table.
Glidescope group (Intubation attempt using Glidescope)
Lightwand group (Intubation attempt using Lightwand)
The patients underwent preanesthetic preoxygenation by mask before a standardized general anesthesia induction (2% lidocaine 40 mg, fentanyl 1 µg/kg, propofol 2 mg/kg followed by rocuronium 0.6 mg/kg) and 3-minute mask ventilation by 100% oxygen and 3 vol% inspired sevoflurane. The difficult airway was simulated by wearing a Philadelphia cervical collar (Tracheotomy Philadelphia Cervical Collars, Össur, Shanghai, China) [
5]. After the adequate neuromuscular blockade (TOF = 0) was confirmed, we checked the laryngeal view and Modified Cormack and Lehane Grade of the patients. The study was designed to compare the duration of the intubation in both groups. The duration of the intubation can be influenced by the intubation environment and conditions. Therefore, in order to make the intubation environment and conditions as identical as possible, Grade 3 patients were included but those who fell into Grade 4 were excluded from the study. The tracheal intubations were attempted with the assigned airway equipment (Glidescope group or Lightwand group). In Glidescope group, Glidescope (Glidescope videolaryngoscopy, Verathon, Bothell, WA, USA) was inserted along the middle of the tongue and positioned at the epiglottis vallecula. The intubation was then performed with a stylet-inserted tracheal tube using the lift blade and confirmation of the glottis on the monitor [
6]. In Lightwand group, the tip of the Lightwand (Surch-LiteTM Orotracheal Lighted Intubation Stylet, Bovie, USA) bent like a "hockey stick" before the jaw lift. The tracheal tube with Lightwand was approached through blind intubation by confirming transillumination [
4]. We allowed a maximum of two tracheal intubation attempts, and planned to abandon our attempts to intubate if one attempt took more than 2 min, or if the oxygen saturation decreased to below 95%. After attempting intubation, we checked for injuries of the lip, teeth and upper airway. If we had not been able to intubate successfully within two attempts, we planned to remove the cervical collar and intubate in the standard fashion.
The data collected included:
Duration of intubation: from the first handling of the airway device until confirmation of the success of the intubation by reading the end-tidal carbon dioxide, and, if two attempts were required, calculating the sum
Successful endotracheal intubation: for Glidescope group, this was defined as visualization of the tracheal tube passing through the vocal cord and confirmation of end-tidal carbon dioxide on a capnograph. For Lightwand group, it was defined as confirmation of transillumination and end-tidal carbon dioxide on a capnograph
The number of attempts: maximum of two attempts allowed, recording the number of attempts required
Interincisor distances: measure of the interincisor distances before and after wearing the Philadelphia cervical collar
Hemodynamic variables: measure of blood pressure, pulse rate, and oxygen saturation immediately before the induction of anesthesia, immediately before intubation, immediately after completion of the intubation, and 1 min after completion of the intubation
Complications: checking for injuries of the lips, teeth, and upper airway, hypertensions and oxygen desaturation (hypertension: blood pressure increased by 20% compared to the baseline [immediately before the induction of anesthesia], oxygen desaturation: oxygen saturation decreased to below 95%)
Our primary outcome was the difference in the duration of the intubation between Lightwand group and Glidescope group. The subject number was determined from a pilot study. The mean ± SD intubation time was 29 ± 18 sec with Lightwand and 44 ± 20 sec with Glidescope. To detect with α = 0. 05, β = 0.827, 27 patients per group were required. Taking a general 10% of patient loss into consideration, 29 patients were included in each group for a total of 58 patients.
Normality test of data was performed using Kolmogrov-Smirnov test. Parametric data were compared using a student's t-test, and proportional data were compared using the χ2 or Fischer's exact test between the two groups. The data are presented as the mean or number ± SD, with a P value considered statistically significant.
Results
One patient in Lightwand group and 2 patients in Glidescope group were excluded from the study because they fell in the Modified Cormack and Lehane Grade 4 when tested by direct laryngoscope after wearing a semi-rigid cervical collar.
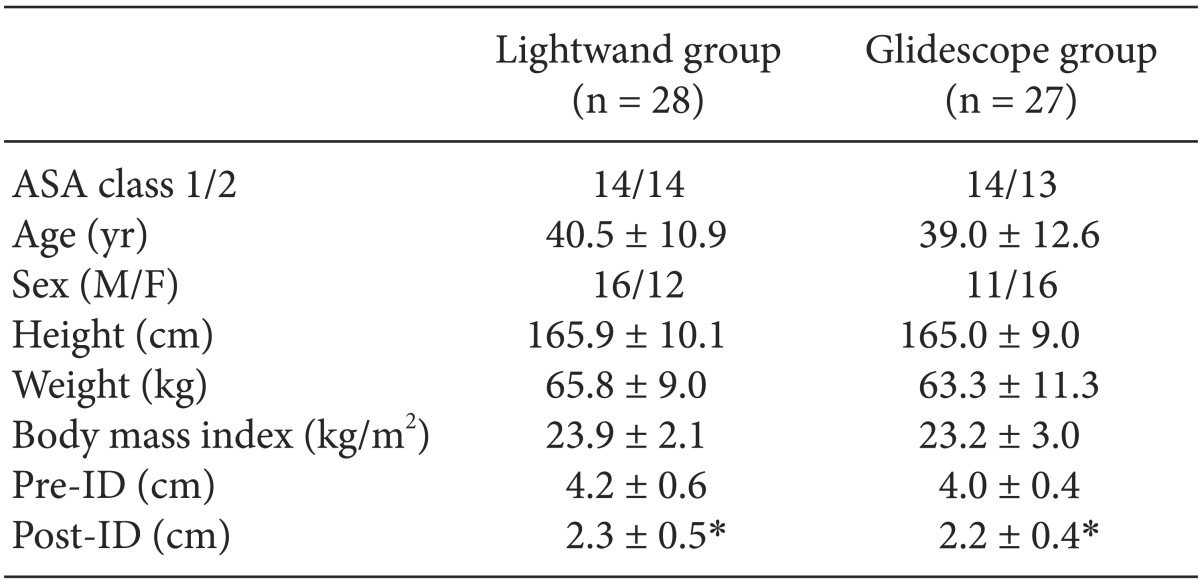
Between the two groups, the characteristics of the patients including the interincisor distance were not significantly different (
Table 1). There was a significant difference between the Pre-ID and Post-ID in the two groups (P < 0.05).
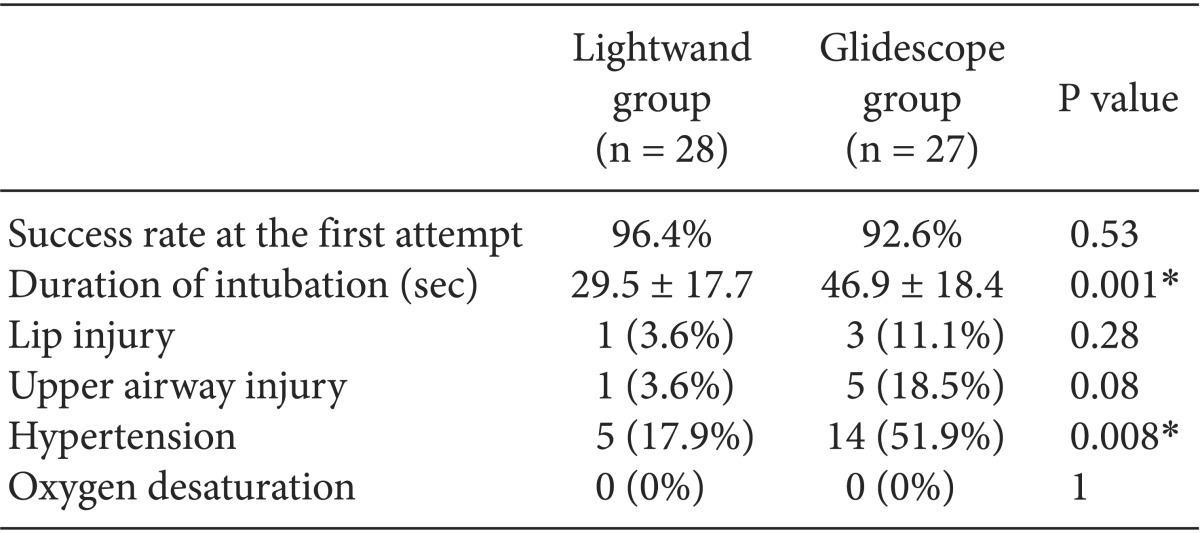
All intubations were completed within two attempts through the assigned airway equipment, and there was no significant difference in terms of success rate at the first attempt of intubation between Lightwand group and Glidescope group (96.4% vs 92.6% respectively, P = 0.53). However, there was a significant difference in the duration of the intubation between Lightwand group and Glidescope group (29.5 sec vs 46.9 sec respectively, P = 0.001) (
Table 2).
Lip and upper airway injuries, hypertensions, and oxygen desaturations are described in
Table 2. There were no statistically significant differences in lip and upper airway injuries between the two groups. However, the incidence of hypertension was significantly different between Lightwand group and Glidescope group (17.9% vs 51.9% respectively, P = 0. 008). Oxygen saturation did not decrease to below 95% for any of the patients.
Discussion
Intubation with a direct laryngoscope is required for direct vision of the vocal cord but is difficult in patients with poor alignment of the oropharyngeal-laryngeal axes [
7,
8]. To obtain alignment of the oropharyngeal-laryngeal axes, neck extension and mouth opening are essential. Therefore the interincisor distance, sternomental distance, thyromental distance, and modified Mallampati tests are all predictor of a difficult airway [
9]. At this point, several studies have been performed by applying a cervical collar for the limitation of cervical movement and mouth opening [
5,
10,
11,
12,
13]. The results of our study showed a decreased interincisor distance and range of neck movement after application of the cervical collar.
In previous studies, both devices had shown excellent success rates at the first attempt. The success rate at the first attempt using Glidescope was reported to be 90-94.4% [
3,
11,
14], and that of Lightwand was reported to be 78-96.8 [
15,
16]. These high success rates at the first attempt correspond with the results of our study. In the present study, the success rate at the first attempt was 96.4% in Lightwand group and 92.6% in Glidescope group. There was no difference in the success rate at the first attempt using Lightwand or Glidescope in patients with limited mouth opening and neck extension.
Endotracheal intubation using Glidescope took more time than when using Lightwand. In the present study, the duration of the intubation with Glidescope and Lightwand was 46.9 ± 18.4 sec and 29.5 ± 17.7 sec, respectively. This resulted from the difficult passage of the Glidescope blade and endotracheal tube through the pharyngeal and laryngeal pathway [
3]. Because of the bulky blade size of Glidescope (the height was 24-27 mm and the width 25 mm), the space for handling the blade of Glidescope and the endotracheal tube is narrow. When the mouth opening and neck extension are limited, the space for handling the blade of Glidescope and the endotracheal tube can be further reduced. Lightwand on the other hand may be little influenced by limitations in the mouth opening and neck extension, as it is a slender stick device.
In our study, endotracheal intubation using Glidescope took about 17 sec longer than when using Lightwand. The clinical significance of this difference in the duration of the intubation (17 sec) is debatable. As there was no desaturation episode in our study, the duration of the intubation using both airway devices was acceptable. However the difference may be meaningful for patients with a poor lung reservoir (due to lung disease, kyphoscoliosis, pregnancy, and obesity) [
17]. In these patients, the mean duration of the intubation using Glidescope (46.9 sec) in the present study may induce desaturation. Endotracheal intubation using Lightwand may therefore be recommended in patients with limited mouth opening and neck extension who also have a poor lung reservoir.
It had been reported that there was no difference in the hemodynamic response to endotracheal intubation using either Lightwand or Glidescope [
18]. However, previous studies were performed on patients with a normal airway. In the present study, the incidence of hypertension was higher in Glidescope group than in Lightwand group. That may be because oropharyngolaryngeal stimulation was more severe in Glidescope group than in Lightwand group. There might be several reasons for this. First, Glidescope may stimulate the sensitive extra-epiglottic structure more than Lightwand [
19,
20]. Second, intubation using Glidescope requires more time than that using Lightwand. Third, the cervical collar can worsen the narrowing that is caused by using Glidescope, therefore increasing the stimulation and duration of the intubation.
In our study, we expected a higher incidence of lip and upper airway injury by Glidescope because of its size and of the narrow space for handling the device compared to Lightwand. However there was no statistically significant difference in terms of lip and upper airway injury. Glidescope was likely to induce complications with patients who had high-risk dental problems because of its large device size. Lightwand on the other hand was prone to causing oral and laryngeal damage due to obligatory blind intubation [
21]. The reason for this result may be that high-risk patients for both devices were excluded from our study. Therefore, endotracheal intubation using Glidescope should be performed with caution on patients with a high risk of upper airway injury.
There are several limitations regarding our study. First of all, the researcher who performed the endotracheal intubations in this study was not blinded to the patient group. Moreover, the recording of the lip and airway injuries was done by another anesthesiologist. Secondly, the study population was Modified Cormack and Lehane Grade 3. Therefore the results cannot be applied to patients falling into other grades of the Modified Cormack and Lehane scale. Lastly, the simulated difficult airway was a limitation of the neck extension and mouth opening, which was achieved by wearing a cervical collar. Therefore, the result of this study cannot be applied to other patients with different types of airway difficulties.
In patients with a simulated difficult airway, there was no significant difference in the success rate at first attempt with either Glidescope or Lightwand. Lightwand required less time than Glidescope to complete the intubation. The incidence of hypertension was lower in the Lightwand group. Thus, if patients are at a high risk of desaturation or cardiovascular instability during the intubation, Lightwand presents advantages over Glidescope regarding patient safety.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download