This article has been
cited by other articles in ScienceCentral.
Abstract
Percutaneous epidural neuroplasty may lead to complications such as hematoma, infection, epidural abscess, meningitis, hypotension, respiratory depression, urinary and fecal dysfunction, sexual dysfunction and paresthesia. Other technical complications may include shearing or tearing, misplacement, blockage and migration of the catheter. We report a case of a 41-year-old female patient, who underwent surgical removal of a sheared catheter, which was retained for 30 months after cervical Racz neuroplasty.
Go to :

Keywords: Catheters, Complication, Epidural space, Neck
Percutaneous epidural neuroplasty with various catheters, such as the Racz catheter, navigation catheter, and so on, has been used widely. These procedures are intended to reduce scar formation, fibrous adhesion and inflammation in patients with neck and low back pain. Racz neuroplasty is a specifically designed procedure for lysis of adhesion with hypertonic saline. A wire-embedded catheter with a fine sheath coated around the wires is specially designed for this procedure.
Many complications are reportedly related to these catheters. Some immediate complications include hypotension, bleeding in the epidural space, bending of the needle tip, penetration of the dura, subdural insertion, catheter shearing, blocking of the catheter and problems during withdrawal of the catheter. Late complications are penetration of the dura, numbness, temporary and permanent paresthesia, bowel and bladder dysfunction, sexual dysfunction, headache, infection, epidural abscess and arachnoiditis. There are several case reports related to a sheared catheter retained in the lumbar epidural space [
1]. However, cases related to the cervical epidural space are not reported to date. We have reported a patient with new neurologic symptoms due to a retained catheter fragment from cervical Racz neuroplasty performed three years earlier. The catheter was incidentally found during cervical epidural block with fluoroscopy. It was removed surgically without any residual symptoms until the 9 months follow-up.
Case Report
A 41-year-old female patient presented with posterior neck pain at our outpatient clinic. The patient had a tingling sensation from the right axilla to the fingertips. She had no special trauma history or other underlying diseases. On physical examination, the spurling test was positive. There was tenderness to the right trapezius muscle with a pain score of 7-points on the numeric rating scale (NRS). The symptom improved after a paravertebral block at the T2 level. She revisited the outpatient clinic 15 months later, with the same symptoms and again received the paravertebral block at the T2 level. Two weeks later, she still had a pain score of 4 to 6-points on NRS. Findings in the cervical spine magnetic resonance imaging (MRI) showed broad central disc protrusion at the C5-6 and C6-7 levels. Two weeks later, cervical Racz neuroplasty was done, and on the next day, after infusion of hypertonic saline through the Racz catheter for 30 minutes, the catheter was removed with no side effects. Two months later, the patient visited the outpatient department with a new symptom. She complained of a tingling sensation on her right arm, without pain in the neck or arm, which subsided after receiving physical therapy and medications. The patient consequently refused further intervention or radiologic examination, and continued to receive physical therapy for neck and arm in the department of rehabilitation medicine.
The patient visited the outpatient clinic every two months, due to numbness of the right arm and a pain score of 3 to 8-points on NRS. She was prescribed 225 mg of pregabalin, and received a paravertebral block on the T2 level. She was maintained on physical therapy. Twenty-eight months after the Racz neuroplasty, the patient still had pain in the neck and right arm, and the intensity and duration of the pain was progressive. She received a paravetebral block on T2 and a right brachial plexus block, when the pain score reached 7-point on NRS. However, the pain did not subside; we therefore chose to do a cervical epidural block as the next line of treatment.
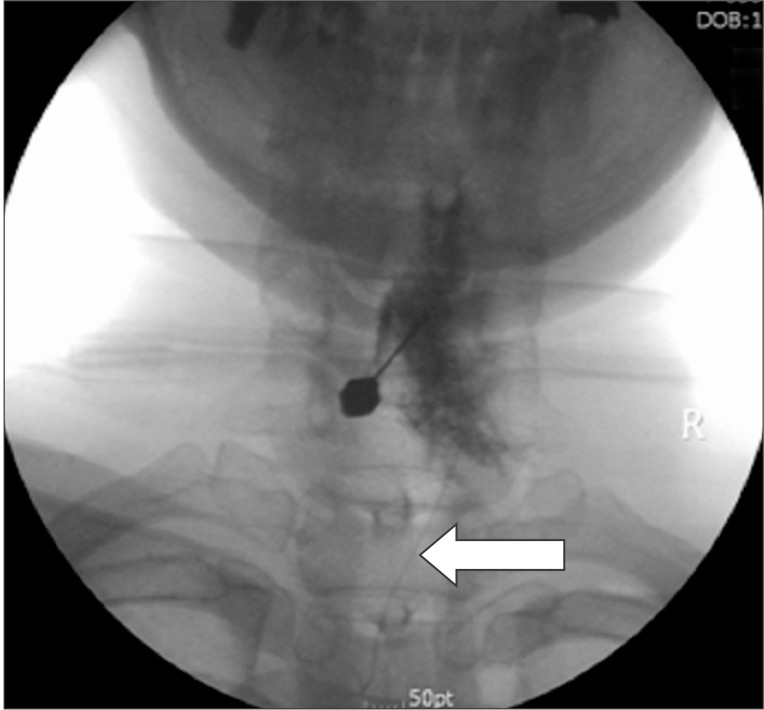
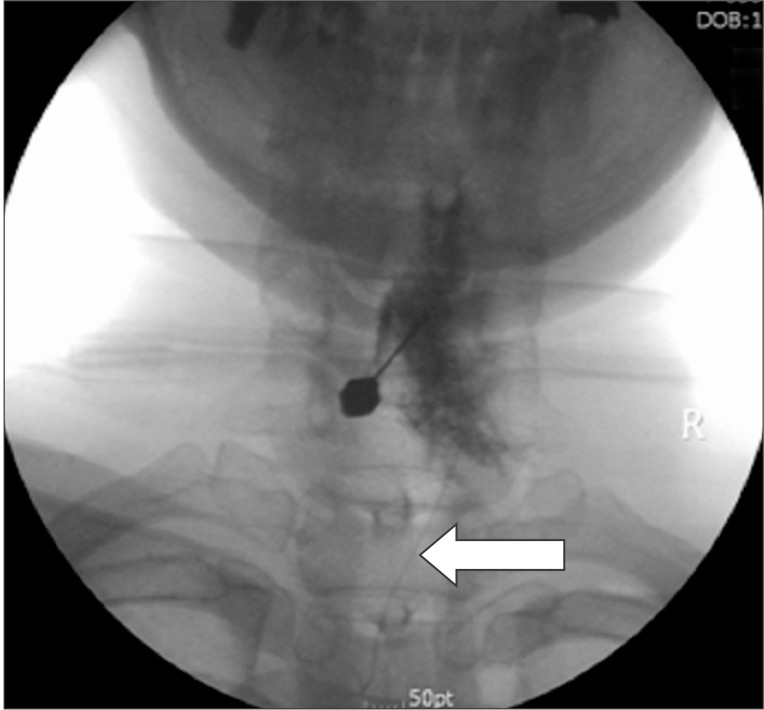
During the procedure, we found a foreign body in the cervical epidural space by fluoroscopy (
Fig. 1). It resembled a Racz catheter fragment inserted 30 months previously. C-spine computed tomography images were obtained to determine the exact location of the proximal and distal tip of the catheter and whether it was knotted or looped. We confirmed that the tip of the catheter was at the right C6-7 foraminal zone (
Fig. 2). We decided that surgical removal was necessary because of the presence of neurologic symptoms. The patient consented, and we consulted a neurosurgeon for surgical removal of the catheter fragment. Two weeks later, it was removed under fluoroscopy in the operating room. After a linear skin incision on the T1-2 level, the paraspinal muscle and interspinous ligament were dissected. The distal sheared tip of the catheter located at a 2 cm depth from skin, was removed. There was no knotting or looping in the removed catheter (
Fig. 3). Findings during the operation were not suggestive of any fibrosis or granuloma tissue formation. The patient's symptom subsided immediately after surgery. During the 9 months post-surgical follow-up, the patient had no neurologic symptoms, nor pain in the neck and arm.
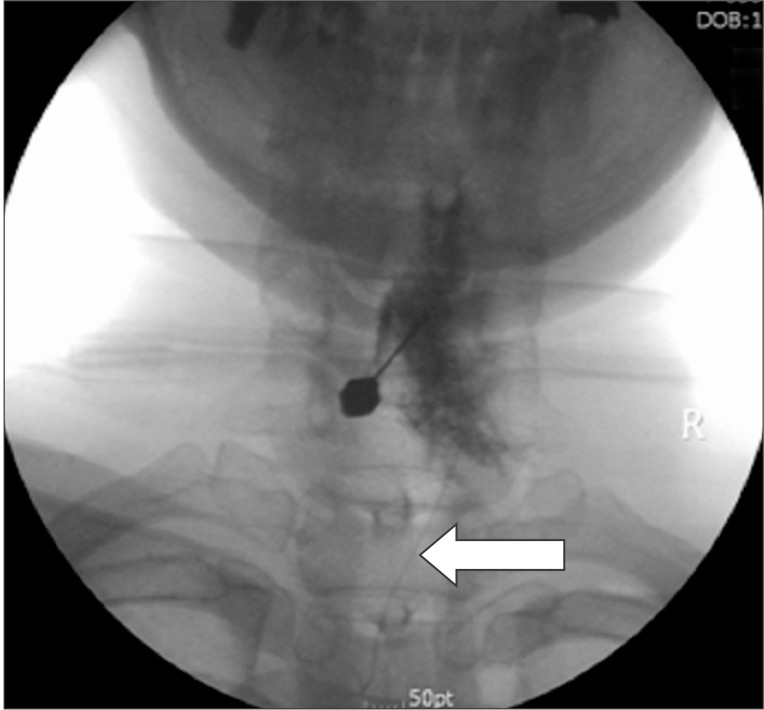 | Fig. 1Fluoroscopy during cervical epidural block. Racz catheter fragm ent seen at the cervical spine level.
|
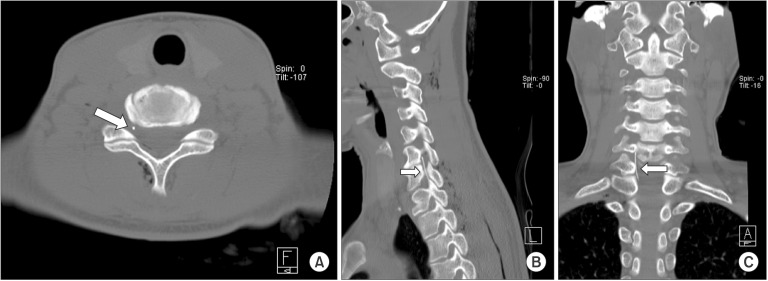 | Fig. 2A computed tomography (CT) image before catheter fragment removal, (A) Transverse section, (B) Sagittal section, (C) Coronal section. The catheter fragment tip at the right C6-7 foraminal zone, without knotting or looping of the catheter.
|
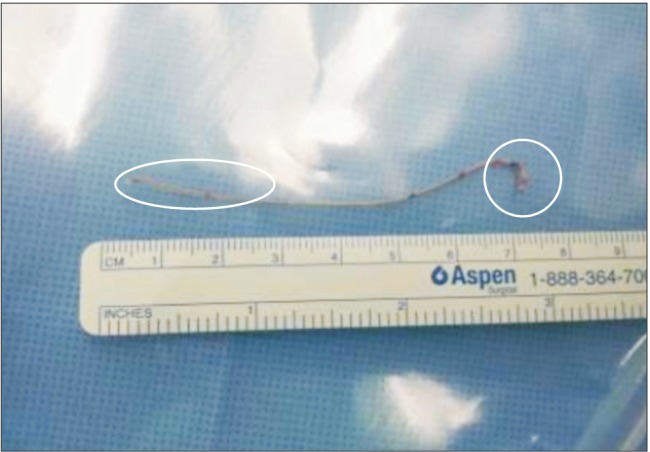 | Fig. 3Removed Racz catheter. The proximal tip of the catheter with shearing of sheath; absence of knotting or looping; and the stretching of wire observed at about the 3 cm segment of the distal tip.
|
Go to :

Discussion
There have been several cases of sheared neuroplasty catheters in the lumbar epidural space, whereas there are no similar case reports in the cervical epidural space. In a study performed in 250 patients who underwent Racz catheter neuroplasty the reported incidence of catheter shearing was 1.2%. The most common cause was bending of the needle tip, with an incidence of 4.8% [
2]. During insertion, the needle tip can come in contact with bony structures and bending can occur. This can seriously damage the end of the catheter, during insertion and removal.
The tension and stretching during insertion or removal of the catheter can also damage the catheter. Catheter shearing depends on the material of the catheter. Polyurethane is considered the strongest material. In another study, Abbott epidural catheters were found to be significantly the strongest, whereas Baxter catheters were significantly the weakest (Abbott [nylon; Abbott Laboratories Inc., Abbott Park, IL, USA], Baxter [nylon; Baxter Healthcare Corp., Deerfield, IL, USA]). Looping or knotting of the catheter during insertion can lead to shearing. Excessively forceful removal of an entrapped catheter due to knotting or looping in epidural space, can also lead to shearing [
3]. Therefore, if too much tension is felt during the removal of the catheter, the cause of entrapment should be evaluated.
When catheter shearing occurs, it is necessary to determine the position of the proximal and distal tip. Fluoroscopy is often used as a first test. For definite evaluation, computed tomography (CT) is the most recommended method, while the use of MRI is controversial. Theoretically, MRI can cause neural damage via thermal injury by a metallic catheter, and dislocation of ferromagnetic catheters [
4,
5,
6]. However, in cases that were evaluated by MRI, there was neither dislocation of the catheter, nor any neurologic sequela [
7,
8].
The recommended methods for the prevention and management of catheter shearing are as follows [9]: (1) continuous application of force slowly; (2) discontinuation of force application if resistance and stretching of catheter is felt. traction may be resumed several hours later; (3) maintenance of the patient in the same position, as during insertion; (4) removal in the flexion position on failure of previous attempts; (5) removal in the extension position on failure of the flexion position; (6) removal with injection of normal saline through the catheter; (7) optional use of a convex surgical frame; (8) optional CT scan to identify the cause of entrapment; (9) consideration of allowing a retained epidural catheter in adult patients; (10) education of "red flags"; and (11) neurosurgical consultation for all cases.
It is controversial whether surgery is indicated in cases of retained catheter fragment. There are several reports of neurologic complications due to direct mass effect of the catheter fragment, as well as the possibility of fibrosis and cyst formation [
7,
10]. There have been a variety of case reports documenting granuloma formation and fibrosis for chronic implanted epidural catheters [
11,
12,
13]. On the other hand, there was no evidence of granulation tissue formation in CT scans of patients with sheared catheter fragment for upto one year [
14].
In the current case, the catheter had been pulled out with excessive force and was sheared in the process.
Fig. 3 showed no knotting and looping of the catheter. Stretched wire observed in the approximately 3 cm segment of the distal tip, indicated that excessive tension caused catheter shearing within the interspinous ligament during removal. We thus reported a symptomatic case of a retained catheter for 30 months in the cervical epidural space that was successfully removed by surgery, without any neurologic complications. In conclusion, although the incidence of catheter shearing is extremely low in Racz catheter neuroplasty, the removal of the catheter is a meticulous process that may require preventive and management practices. The precise length of the removed catheter should be compared with the original catheter, and follow up images should be taken whenever new symptoms develop.
Go to :