Abstract
Background
Optimal head and neck positioning and clinical experience are important factors for successful endotracheal intubation in patients with a difficult airway. This study aimed to investigate the rate of successful endotracheal intubation between the sniffing and ramped positions in patients with an expected difficult intubation.
Methods
The study included 204 patients with an expected difficult intubation (airway difficulty score ≥ 8) based on the preoperative airway assessment. The patients were randomized into the following groups: group S was placed in the sniffing position, and group R was placed in the ramped position during direct laryngoscopy. The primary outcome was successful endotracheal intubation and the secondary measure was laryngeal view in the ramped or sniffing position when the operating table was placed at two different heights.
Results
Group R showed a higher rate of successful endotracheal intubation and better laryngeal view than group S (P < 0.05). The rate of successful endotracheal intubation was higher in group R than in group S at both heights of the operating table; but, it was not different within each group. Laryngeal view was not different between the two groups and within each group when the two heights of the operating table were used. Fully trained and experienced attending anesthesiologists achieved a higher rate of successful endotracheal intubation than less experienced residents in group R (P < 0.05) but not in group S.
Go to : 
A difficult airway can often be predicted because it is determined by head and neck anatomy and the size of the chest. However, if a difficult airway is encountered unexpectedly and is not managed correctly and rapidly, it results in significant morbidity and mortality [1].
Optimal head and neck positioning is important in patients with a difficult airway, although less optimal positioning could be applied [2]. The sniffing position has traditionally been considered the optimal position of the head and neck for successful direct laryngoscopy [3]. However, the ramped position has also been proposed to facilitate ventilation and visualization of the glottis for intubation in both obese and non-obese patients. This position can be achieved by placing a stack of blankets or specially designed pillows under the patients' head and upper torso so that the external auditory meatus and the sternal notch are aligned horizontally [4,5,6].
Most of the studies have reported differences in laryngeal view between the two positions in relation to obesity [5,6,7,8,9,10]. The patient's anatomy and the technique employed for laryngoscopy have a significant effect on the laryngeal view. The technique itself is influenced by a variety of factors including the laryngoscopic force and the skills, experience, and training of the anesthesiologist [8].
The aim of this study was to compare the rate of successful endotracheal intubation and laryngeal view between the sniffing and ramped positions, when they were employed by less experienced residents or fully trained and experienced attending anesthesiologists in patients with an expected difficult intubation based on the preoperative airway assessment.
Go to : 
Ethical approval for this study (Registration No. 1478) was provided by the Institutional Review Board on November 2011. Written informed consent was obtained from all participants. The study was performed at our hospital and branch hospital from December 2011 to July 2014. A total of 204 adult patients (≥ 18 or < 70 years) with an expected difficult intubation (airway difficulty score ≥ 8) [1] based on the preoperative airway assessment among 1,214 patients under general anesthesia were included in this study. Patients with an unstable cervical spine and those who required rapid sequence intubation were excluded from the study.
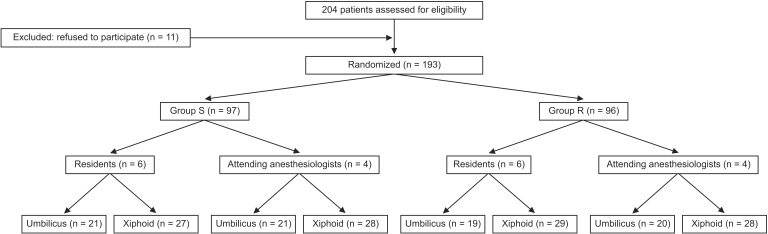
Preoperative airway assessment was performed with patients in the sitting position by an attending anesthesiologist working in each hospital and who was not involved in the study. The airway difficulty score included thyromental distance, modified Mallampati class, mouth opening, neck mobility, and dentition (Table 1). Using a computer-generated random number table, patients were randomly assigned into either the sniffing position (group S) or the ramped position (group R) with different heights of the operating table (umbilical or xiphoid level), which were achieved either by the less experienced residents or the fully trained and experienced attending anesthesiologists. A total of 204 patients were assessed for eligibility, and 193 patients were randomized to two groups (group S = 97, group R = 96) according to the head and neck position because 11 patients refused to participate in the study. The residents or attending anesthesiologists in each group were randomized to the umbilical (n = 96) or xiphoid level (n = 97) according to different heights of the operating table; but, two residents attempted endotracheal intubation at the xiphoid level instead of the umbilical level in 5 cases by mistake. As a result, 102 patients were intubated at the xiphoid level and 91 patients were intubated at the umbilical level in this study (Fig. 1).
All patients were premedicated with i.v. midazolam (2-3 mg) before arrival in the operating room. Routine monitoring, including pulse oximetry, automatic blood pressure measurement, electrocardiography, and end-tidal CO2 measurement, was performed in all patients. The induction of anesthesia was started with a slow (30-60 s) i.v. bolus dose of remifentanil 1 µg/kg followed by propofol 1-2 mg/kg; in all patients, tracheal intubation was facilitated with succinylcholine (2 mg/kg) or rocuronium (0.9 mg/kg). The choice of a muscle relaxant was at the discretion of the laryngoscopist.
Direct laryngoscopy was performed by residents with 2 years of experience or attending anesthesiologists with 10 years of experience. Patients in the sniffing position were placed on a flat operating table with an 8 cm high pillow under their heads to elevate the occiput. Patients in the ramped position were laid on a ramp made of a few layers of folded blankets and placed on a flat operating table. The blankets were then added or removed to ensure that the patient's head was above the shoulders and the external auditory meatus and the sternal notch were in the same horizontal plane.
Because successful endotracheal intubation may depend on the height of the operating table, we investigated the laryngeal view and endotracheal intubation attempts according to different levels of the operating table. The height of the operating table was adjusted or a stepstool was used so that the patient's forehead was at the level of the umbilicus or xiphoid process of the laryngoscopist. Laryngoscopy was performed using Macintosh blade 3. At the first attempt, a malleable stylet in a hockey-stick shape was used for tube placement. If the first attempt failed because the visualization of the glottis or the placement of the endotracheal tube was difficult, the modified bimanual laryngoscopy was performed in the second attempt in accordance with the instructions of the laryngoscopist. The modified bimanual laryngoscopy involves the following steps. An anesthetic nurse laid her hand on the patient's thyroid cartilage, and then the laryngoscopist guided the nurse's hand with his/her right hand to achieve the best laryngeal view and said "keep the pressure and direction." The assistant maintained the pressure on the thyroid cartilage in the same direction and with same force as guided by the laryngoscopist during the tracheal intubation.
Successful placement of the endotracheal tube was confirmed using capnography. After 2 failed attempts at laryngoscopy and endotracheal intubation, a call for help was generated. In procedures performed by the residents, the patients were managed by another skilled attending anesthesiologist at their discretion. Alternative techniques included the use of a laryngeal mask airway or fiberoptic bronchoscopy. Failed endotracheal intubation by direct laryngoscopy was defined as the need for an alternative technique or additional operator after two direct endotracheal intubation attempts had failed.
The laryngeal view with direct laryngoscopy was evaluated by using Cormack-Lehane (CL) classification. Grading was performed by the CL classification wherein grade 1 was complete visualization of the vocal cords, grade 2 was partial view of the vocal cords or arytenoids, grade 3 was only epiglottis seen (none of glottis seen), and grade 4 was neither glottis nor epiglottis seen. The primary outcome was successful endotracheal intubation and the secondary measure was laryngeal view in the ramped or sniffing position when the operating table was placed at two different heights.
A preliminary investigation showed that the rate of successful endotracheal intubation according to the head and neck positions at the table height of the umbilical level was 60% in group R and 40% in group S. Thus, a sample size of 97 patients in each group was needed to demonstrate a significant difference with a power of 80% and an α-coefficient of 0.05. Assuming a 5% dropout rate, the final sample size was determined to be 102 patients in both groups. Statistical analyses were performed using the Statistical Package for Social Sciences software (SPSS 18.0 for Windows; SPSS Inc., IL, USA). The results are presented as mean ± standard deviation or the number (percentage) of patients. Pearson's chi-square or Fisher's exact test was used to analyze nonparametric data such as sex, airway difficulty scores, CL classification, attempts of endotracheal intubation). Comparisons of age, height, body weight, and body weight were conducted using the Student's t test.
Go to : 
No significant differences were observed between the two groups with respect to age, sex, height, body weight, or body mass index. Airway difficulty scores in both groups were not significantly different (Table 2).
Group R showed a higher rate of successful endotracheal intubation than group S (Tables 3 and 4). Laryngeal view was not significantly different between the two groups and within each group (Table 5). The rate of successful endotracheal intubation at both heights of the operating table was significantly higher in group R than in group S, but it was not significantly different within each group (Table 6). Fully trained and experienced attending anesthesiologists achieved a higher rate of successful endotracheal intubation than less experienced residents in group R but not in group S (Table 7).
Go to : 
The incidence of difficult endotracheal intubation ranges from 5 to 30%, but variations in clinicians' expertise and experience greatly influence the subjective impression of intubation difficulty, and the need for additional equipment or operators [10,11,12,13]. The incidence of CL grade 3 or 4, which was considered as difficult endotracheal intubation, was 8.3% in our study.
Anesthesiologists must define the management strategy for securing the airways in cases involving difficult intubation. They can choose techniques to optimize the subsequent attempts at laryngoscopy. These techniques include alteration of patient position, use of an intubating stylet, optimal external laryngeal manipulation, or the use of a different blade or type of laryngoscope [1,2].
Proper positioning of the head and neck in patients undergoing direct laryngoscopy is an important step for successful endotracheal intubation. Improper positioning may lead to prolonged or failed endotracheal intubation attempts because of the inability to visualize the larynx. A standard definition of the sniffing position is that the neck should be flexed 35° on the chest and the head extended at the atlanto-occipital joint to produce a 15° angle between the facial and the horizontal planes in normal-weight patients [2,4].
One of the disadvantages of the sniffing position is its inadequacy in optimizing the glottis exposure in direct laryngoscopy in obese patients [11]. Moreover, some authors have questioned the effectiveness of this position even in normal-weight individuals [4,6,9]. The majority of studies on the ramped position include obese patients [5,6,7,8,9,10]. In these patients, neck flexion of 35° on the chest cannot be achieved by raising the occiput. Their anatomy may require raising the occiput to achieve not only 35° of neck flexion on the chest, but also 90° of head extension on the neck at the atlanto-occipital joint. In other words, in the ramped position, a horizontal alignment can be achieved between the external auditory meatus and the sternal notch either by placing a stack of blankets or by using one of the specially designed and commercially available pillows [2,14].
Ramped position is usually recommended for intubating morbidly obese patients. In our study, the ramped position in patients with an expected difficult intubation (airway difficulty score ≥ 8) based on the preoperative airway assessment provided a higher rate of successful endotracheal intubation and better laryngeal view by direct laryngoscopy than the sniffing position. Fully trained and experienced attending anesthesiologists achieved a higher rate of successful endotracheal intubation in the ramped position than in the sniffing position.
This may be due to the fact that fully trained and experienced attending anesthesiologists have a lot of clinical experience with both positions and better interpretation of the laryngeal view and laryngoscopic skills than less experienced residents, who are not used to the ramped position compared to the sniffing position for intubating patients with normal airway anatomy.
The operating table should be at a height that facilitates endotracheal intubation via direct laryngoscopy. There have been few studies investigating the optimal height of the operating table for direct laryngoscopy. In general, the patient's head should be placed at the level of or higher than the anesthesiologist's waist to prevent unnecessary back strain during laryngoscopy. In the present study, the umbilical or xiphoid level of the patient's forehead above the anesthesiologist's waist was not significant in laryngeal view between the ramped position and the sniffing position; however, the rate of successful endotracheal intubation in the ramped position was higher than that of successful endotracheal intubation in the sniffing position irrespective of the height of the operating table.
Taken together, the ramped position, irrespective of the height of the operating table, in attending anesthesiologists than in residents might be helpful for obtaining a better laryngeal view and endotracheal intubation in patients with an expected difficult intubation.
Our study has several limitations. Firstly, as a measure for the laryngeal view, the CL classification is frequently used to describe the laryngeal view on direct laryngoscopy. The reproducibility of CL classification was limited, with a poor intraobserver reliability and a fair inter-observer reliability [15,16]. Secondly, for comparison of the laryngeal view between positions and between heights of the operating table, multiple laryngoscopies may be needed in the same patient for assessing the reliability of the CL classification. However, we could not perform repetitive laryngoscopy in the same patient according to different positions and heights of the operating table because of ethical concerns associated with this approach. Lastly, in our study, all laryngoscopies were performed by a relatively small number of residents (n = 12) or attending anesthesiologists (n = 8); hence, the tendency to relatively narrow the conditions and the validity of its results might be criticized.
In conclusion, the ramped position in fully trained and experienced attending anesthesiologists is better than the sniffing position irrespective of the height of the operating table for endotracheal intubation in patients with an expected difficult intubation based on the preoperative airway assessment.
Go to : 
Acknowledgments
This study was supported by Wonkwang clinical research institute and Wonkwang University 2014.
Go to : 
References
1. Janssens M, Hartstein G. Management of difficult intubation. Eur J Anaesthesiol. 2001; 18:3–12. PMID: 11270007.

2. Benumof JL. Management of the difficult adult airway. With special emphasis on awake tracheal intubation. Anesthesiology. 1991; 75:1087–1110. PMID: 1824555.
3. Adnet F, Baillard C, Borron SW, Denantes C, Lefebvre L, Galinski M, et al. Randomized study comparing the "sniffing position" with simple head extension for laryngoscopic view in elective surgery patients. Anesthesiology. 2001; 95:836–841. PMID: 11605921.

4. El-Orbany M, Woehlck H, Salem MR. Head and neck position for direct laryngoscopy. Anesth Analg. 2011; 113:103–109. PMID: 21596871.

5. Rao SL, Kunselman AR, Schuler HG, DesHarnais S. Laryngoscopy and tracheal intubation in the head-elevated position in obese patients: a randomized, controlled, equivalence trial. Anesth Analg. 2008; 107:1912–1918. PMID: 19020138.

6. Lebowitz PW, Shay H, Straker T, Rubin D, Bodner S. Shoulder and head elevation improves laryngoscopic view for tracheal intubation in nonobese as well as obese individuals. J Clin Anesth. 2012; 24:104–108. PMID: 22301204.

7. Collins JS, Lemmens HJ, Brodsky JB, Brock-Utne JG, Levitan RM. Laryngoscopy and morbid obesity: a comparison of the "sniff" and "ramped" positions. Obes Surg. 2004; 14:1171–1175. PMID: 15527629.

8. Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice Guidelines for Management of the Difficult Airway: An Updated Report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013; 118:251–270. PMID: 23364566.
9. Ranieri D Jr, Filho SM, Batista S, do Nascimento P Jr. Comparison of Macintosh and Airtraq™ laryngoscopes in obese patients placed in the ramped position. Anaesthesia. 2012; 67:980–985. PMID: 22670846.
10. Walls RM, Brown CA 3rd, Bair AE, Pallin DJ. Emergency airway management: a multi-center report of 8937 emergency department intubations. J Emerg Med. 2011; 41:347–354. PMID: 20434289.

11. Sagarin MJ, Barton ED, Chng YM, Walls RM. Airway management by US and Canadian emergency medicine residents: a multicenter analysis of more than 6,000 endotracheal intubation attempts. Ann Emerg Med. 2005; 46:328–336. PMID: 16187466.

12. Orebaugh SL. Difficult airway management in the emergency department. J Emerg Med. 2002; 22:31–48. PMID: 11809554.

13. Martin LD, Mhyre JM, Shanks AM, Tremper KK, Kheterpal S. 3,423 emergency tracheal intubations at a university hospital: airway outcomes and complications. Anesthesiology. 2011; 114:42–48. PMID: 21150574.
14. Adnet F, Borron SW, Lapostolle F, Lapandry C. The three axis alignment theory and the "sniffing position": perpetuation of an anatomic myth? Anesthesiology. 1999; 91:1964–1965. PMID: 10598648.

15. Ochroch EA, Hollander JE, Kush S, Shofer FS, Levitan RM. Assessment of laryngeal view: percentage of glottic opening score vs Cormack and Lehane grading. Can J Anaesth. 1999; 46:987–990. PMID: 10522589.
16. Krage R, van Rijn C, van Groeningen D, Loer SA, Schwarte LA, Schober P. Cormack-Lehane classification revisited. Br J Anaesth. 2010; 105:220–227. PMID: 20554633.

Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download