Hemophagocytic lymphohistiocytosis (HLH) is a life-threatening condition characterized by pathological immune activation leading to a severe hyperinflammatory condition and organ damage including fever, cytopenia, hepatitis, coagulopathy, and central nervous system damage [1,2]. HLH consists of two different conditions: primary or genetic HLH, and secondary or acquired HLH. Primary HLH is associated with autosomal recessive genetic mutations and occurs primarily in children, although a few adult cases have been reported [3]. Secondary HLH which is associated with predisposing factors is more common in adults [1]. Predisposing factors include primary or acquired immunodeficiency, malignancy, and autoimmune disease, infections. Viral-associated HLH occurs most commonly with the Epstein-Barr virus, although the cytomegalovirus, human herpes virus 8, human immunodeficiency virus, and other viruses have been reported [1,4].
We present an 18-year-old man with HLH in order to illustrate clinical features and the importance of prompt diagnosis and therapy. An 18-year-old man was admitted to undergo an operation for diaphragmatic hernia due to a traffic accident. He was diagnosed with a minimal subdural hemorrhage, left femur fracture, liver and spleen contusion and diaphragmatic hernia. His previous medical history revealed Down syndrome with ostium secondum defect and anoplasty 17 years ago. He was previously healthy and taking no regular medications.
Three days after the operation, he was admitted to the intensive care unit (ICU) to manage respiratory distress which had occurred in the general ward. A chest radiograph revealed consolidation and pleural effusion in both lungs, and he was intubated for desaturation. He was ventilated by lung-protective ventilation, but his state did not improve for several days. although we used high dose sedatives, he was so irritable that the patient-ventilator dyssynchrony persisted. The brain-computed tomography demonstrated no specific lesions except for a minimal subdural hemorrhage and intracranial hemorrhage. To maintain the mean blood pressure over 65 mmHg, norepinephrine and vasopressin were infused, and no abnormal findings were observed on the transthoracic echocardiogram.
After 4 days in the ICU, a vesicular skin rash abruptly appeared on the pateint's face and trunk. The Tzanck test revealed that he had chickenpox. He was isolated and administered acyclovir. Additionally, he was given broad-spectrum antibiotics and antipyretics, but a fever over 39℃ was maintained.
His clinical conditions met the criteria for septic shock: fever, tachypnea, edema, leukopenia, elevated C-reactive protein, hypotension, arterial hypoxemia and thrombocytopenia. Therefore, hemodynamic support and adjunctive therapy were performed according to sepsis. Despite fluid resuscitation and broad-spectrum antibiotics therapy, his clinical outcome showed no significant difference.
To rule out an autoimmune disease, rheumatoid factor, antineutrophil antibody perionuclear antineutrophil cytoplasmic antibody and cytoplasmic antineutrophil cytoplasmic antibody tests were carried out. All were found negative, and the C3 (108 mg/dl) and C4 (29 mg/dl) levels were in the normal range. Suspecting infections, various tests (aspergillus galactomannan antigen, virus hepatitis, aci-fast bacillus smear, mycobacterium culture), cultures (sputum, throat, blood, urine, stool, catheter tip, pleural fluid, bronchial washing, wound swab), and polymerase chain reactions (cytomegalovirus, pneumocystis jirovecii, adenovirus, respiratory syncytial virus, influenza, parainfluenza, legionella) were performed, but only yeast and candida were found in the urine culture.
Although we could not identify the specific causes, he still presented fever and pancytopenia. 27 days after admission, suspecting him of having hematological abnormalities, a bone marrow biopsy was performed, and hemophagocytes were found. Hepatomegaly and splenomegaly were also found in the abdomen-computed tomography, while enlarged lymph nodes were found in the neck-computed tomography. Besides, the soluble interleukin-2 receptor (1,540 U/ml) and triglyceride (293 mg/dl) showed high levels, but the fibrinogen (263 mg/dl) levels were normal.
Diagnosed with HLH, a steroid pulse therapy was initiated with methylprednisolone and dexamethasone, and cyclosporine A was also administered. The patient responded well to treatment, as the pancytopenia improved and the fever was controlled. After 41 days in the ICU, he was weaned off the ventilator and was moved to the general ward.
The clinical symptoms of HLH are fever, chills, general weakness, gastrointestinal symptoms, hepatomegaly, splenomegaly, lymph nodes enlargement, rash and jaundice, which seem like symptoms of sepsis. In this case, the symptoms did not appear to be related to trauma, as the patient he did not show these clinical signs until three days after the surgery.
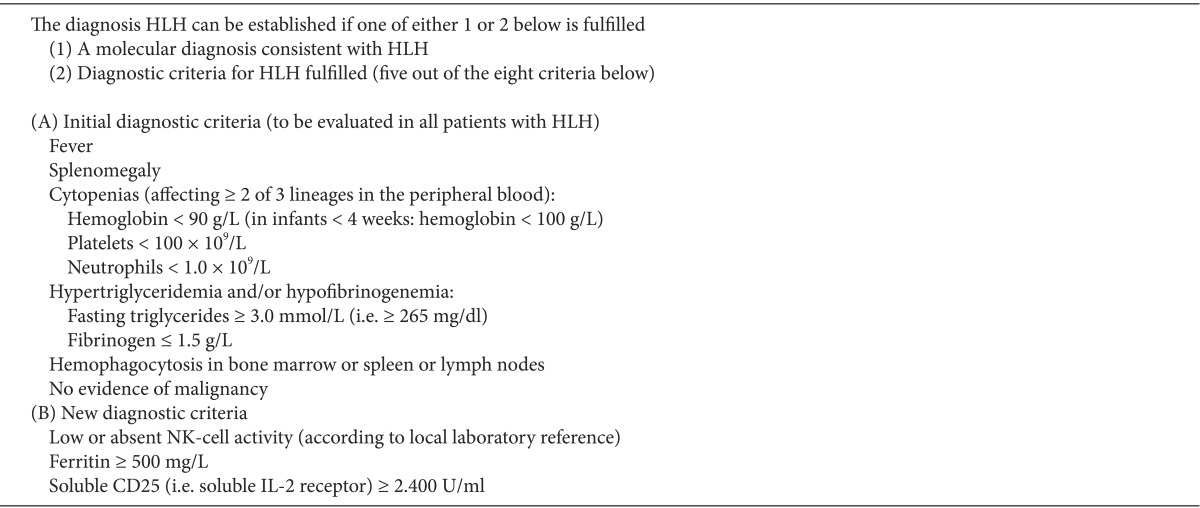
It is reported that HLH mostly occurs in children, but it can occur in all ages [3]. The diagnosis of HLH is described in Table 1 [3]. Out of 8 clinical signs or blood tests, the diagnosis of HLH typically requires five or more clinical criteria. This case included 6 criteria items, namely, fever, splenomegaly, cytopenia, hemophagocytosis in the bone marrow, hypertriglyceridemia, and a high ferritin level. The diagnosis of HLH is necessary to the broad investigations of underlying diseases, particularly infection, lymphoma, leukemia, and autoimmune diseases, such as systemic lupus erythematosus [5].
Pathologically, infected T-lymphocytes cause clonal proliferation, producing high levels of activating cytokines such as TNF-α, INF-γ, IL-1, IL-2, IL-6, and IL-18. The cytokines lead to fever and activate the macrophage consistently, resulting in hemophagocytosis [2,4].
HLH is associated with connective tissue disease and malignancy as well as infections from viruses, bacteria, fungi and parasites. Although yeast and candida were cultured in the urine, they responded well to the antibiotics and immediately stopped growing. This was therefore considered to be varicella-zoster-triggered HLH.
The treatment for HLH is the early administration of chemotherapy, such as etoposide and dexamethasone, with a dose adjustment for patients with renal failure. Cyclosporine is part of the protocol, but is often withheld until the patient's clinical status and renal function improve. Patients with viral-associated hemophagocytic syndrome should receive appropriate antiviral therapy such as ganciclovir. Other interventions include intrathecal therapy with methotrexate and prednisolone in patients with evidence of a central nervous system disease, as well as supportive therapy with antimicrobial prophylaxis and intravenous immunoglobulins [1].
In this case, much time was spent diagnosing the accurate disease, but the patient improved clinically and responded well to steroid pulse therapy and cyclosporine A. His clinical course resembled that of sepsis, with persistent fever and pancytopenia. Early suspicion and diagnostic are very important for the timely treatment of HLH, before an overwhelming disease activity causes irreversible damage and make the response to treatment less likely.
References
1. Cheung C, Owen D, Brar H, Sweet DD, Yoshida E, Dalal B. Hemophagocytic Lymphohistiocytosis in Adults: Two Instructive Cases. UBCMJ. 2013; 4:17–22.
2. Seo JY, Seo DD, Jeon TJ, Oh TH, Shin WC, Choi WC, et al. A case of hemophagocytic syndrome complicated by acute viral hepatitis A infection. Korean J Hepatol. 2010; 16:79–82. PMID: 20375646.

3. Roganovic J, Kvenic B, Jonjic N, Sili-Bekafigo I, Kardum-Skelin I. Neonatal Hemophagocytic Lymphohistiocytosis-Case Report. Coll Antropol. 2010; 34:285–290. PMID: 20432763.
4. Mun JI, Shin SJ, Yu BH, Koo JH, Kim DH, Lee KM, et al. A case of hemophagocytic syndrome in a patient with fulminant ulcerative colitis superinfected by cytomegalovirus. Korean J Intern Med. 2013; 28:352–355. PMID: 23682230.

5. Kim YC, Kim GM, Lee HS, Hong SI, Cheung DY, Kim JI, et al. A case of hemophagocytic syndrome in an ulcerative colitis patient. Korean J Gastroenterol. 2010; 56:45–48. PMID: 20695130.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download