Abstract
Massive air leakage through a lacerated lung produces inadequate ventilation and hypoxemia. Tube exchange from a single to double lumen endotracheal tube (DLT), and lung separation to maintain oxygenation, are challenging for seriously injured patients. In this case report, we aim to describe how a bronchial blocker (BB) makes it easier to perform a lung separation in this situation; it also increases the overall safety of the procedure. A 35-year-old female (163 cm, 47 kg) suffered from blunt chest trauma due to a traffic accident; the accident caused right-sided lung laceration with massive air leakage. Paradoxically, positive ventilation worsened SaO2 and leakage increased through a chest tube. We introduced BB while the patient was still awake: Left-side one-lung ventilation (OLV) was established and anesthesia was induced. After PaO2 was maximized with OLV, we changed the endotracheal tube to DLT without a hypoxic event. By BB placement, we maintained PaO2 at a secure level, conducted mechanical ventilation and exchanged the tube without deterioration.
Bronchial blocker (BB) is a simple device to facilitate one-lung ventilation; the procedure has a superior advantage over a double-lumen endotracheal tube (DLT), including ease to perform and availability without replacement of tube exchange [1]. From this this point of view, BB is an excellent candidate for unrecognized need of one-lung ventilation in a critically-traumatized patient with hypoxemia. Traumatic lung laceration, which produces inadequate ventilation due to air leakage, is usually managed by chest tube insertion in order to expand the damaged lung. In most cases, chest tube insertion and thoracic drainage is enough to maintain adequate oxygenation; endotracheal intubation, lung separation, and positive pressure ventilation support are required when the air leakage flow rate through traumatic bronchopulmonal fistular is high [2]. We report the case of a patient who required lung separation due to substantial air leakage from lung laceration. Because of a damaging lung laceration, the rate of air leakage was too high, positive pressure ventilation support through already intubated single-lumen endotracheal tube (SLT) produced systemic desaturation in the patient. The patient's arterial oxygen tension already reached the hypoxemic stage, any interruption of ventilation could produce critical arterial hypoxemia. Maintaining the patient's arterial oxygen tension at a safe level was the key to management until surgical correction could be conducted.
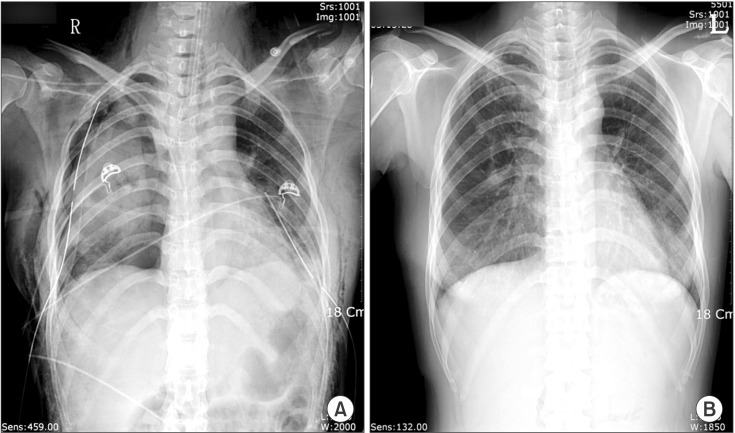
A 35-year-old female (163 cm, 47 kg) suffered from blunt chest trauma due to a traffic accident. On arrival at the emergency department of the local hospital, the patient presented with low-oxygen saturation (SaO2). Thus, a 7.0 mm-ID endotracheal tube was immediately inserted and self respiration was supported with supplemental oxygen through a T-piece. Chest X-rays and computed tomography scans revealed a substantial lung laceration: the pneumothorax and hemothorax of right lung and a fracture of the fourth rib with minimal pneumothorax of left lung (Fig. 1). The patient's SaO2 did not improve despite bilateral underwater-seal chest drainage. Moreover, every time clinicians tried to assist the patient with ventilation, the patient's SaO2 dropped quickly and only spontaneous respiration maintained SaO2 levels around 90%. The hospital's emergency department transferred the patient to our hospital for further management.
Upon arrival at our emergency department, the patient had clear consciousness, showed restlessness, and complained of shortness of breath. Arterial blood gas analysis (ABGA) with 10 L/min of supplemental oxygen through the T-piece, showed pH, 7.5; PaCO2, 32 mmHg; PaO2, 58 mmHg, and SaO2, 92%. Initial vital signs were blood pressure, 110/60 mmHg; pulse rate, 93 beats/min; respiratory rate, 19 breaths/min; and body temperature, 37.4℃. Laboratory test results were within the normal range, except for elevated liver enzymes. Because arterial oxygen tension did not respond to conventional pneumothorax management, and a large amount of air leak with blood was observed through right-side chest drain, we decided to perform an emergency thoracic exploration.
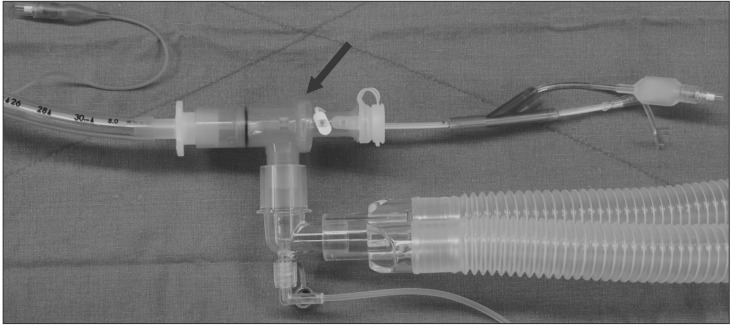
Massive air leakage was thought to be the cause of hypoxemia in this patient [3]. In this situation, it was certain that controlled ventilation worsened the patient's PaO2 without lung separation. Promptly, we decided to apply the one-lung ventilation through the relatively less-injured left lung. We placed bronchial blocker (BB, COOPDECH Endobronchial Blocker Tube, Daiken Medical Co., Ltd., Osaka, Japan) through existing SLT and initiated left-sided one-lung ventilation (OLV). During the procedure, the joint connector permitted spontaneous respiration simultaneously placing BB at adequate site with fiberoptic bronchoscopy (Fig. 2). The balloon of BB was placed at the proximal portion of bronchus intermedius and it was confirmed with a fiberoptic bronchoscope (FOB, LF40P, flexible fiberscope, Olympus, Tokyo, Japan). After five minutes with one lung, assisted ventilation, the patient's SaO2 was raised to around 95% with 100% oxygen; the patient felt more comfortable with OLV. The leaked gas through the chest tube on the right side disappeared, even as we tried with manually assisted ventilation. Blood gas analysis revealed that the patient's PaO2 reached 113 mmHg. We then conducted general anesthesia with hypnotics and muscle relaxant. Fifteen minutes after controlled, positive pressure, left-sided OLV was performed with a minimal positive end-expiratory pressure (PEEP, 5 cmH2O), ABGA showed pH, 7.41; PaCO2, 37 mmHg; PaO2, 241 mmHg, and SaO2, 100%. After confirming a safe level of PaO2, the endotracheal tube was exchanged with a 35-Fr left-sided double lumen tube (BronchoCath™, Mallinckrodt Medical Inc., Athlone Co., Westmeath, Ireland). A10 cmH2O continuous positive airway pressure (CPAP) with 100% oxygen was then applied to the right lung using a CPAP system. After 15 minutes, ABGA results were pH, 7.38; PaCO2, 41 mmHg; PaO2, 251 mmHg; and SaO2, 100%. The patient was then placed in the left lateral decubitus position; open thoracic exploration was started. When the right thoracic cavity was opened through lateral posterior thoracotomy, the left lung totally collapsed despite 10 cmH2O CPAP. Air leak tests revealed two substantial lung lacerations. The duration of OLV was approximately 70 minutes, and arterial oxygen tension was maintained at a safe level during the operation.
Blunt trauma to the thorax produces temporarily increased airway pressure and induces traumatic pneumothorax like a popping balloon. In general, supplementary oxygen and chest tube insertion with an underwater-seal are useful methods for ensuring appropriate levels of ventilation [4].
We treated a patient with multiple substantial lacerations on one-side of the lung; SaO2 was not secured despite the recommended treatment given above. When assisted positive pressure ventilation was applied to the patient, almost all of the inspired gas simply passed through the lacerated right lung where extremely low airflow resistance, resulting in little alveolar ventilation in the left lung and worsened arterial oxygen tension. In this situation, if the patient was paralyzed with muscle relaxants and positive pressure ventilation is initiated in order to conduct general anesthesia, almost all inspired gas escaped through the laceration wounds and arterial oxygen tension gradually worsened. Thus, we decided to perform left-sided OLV before induction of anesthesia. By doing this, we expected to increase alveolar ventilation of the left lung [2,5,6].
Because arterial oxygen tension remained in a mild hypoxic state and the patient had clear consciousness, minimal interruption of spontaneous respiration was the most important aspect of management. Thus, we choose BB insertion through already placed SLT instead of DLT to minimize interruption of spontaneous ventilation and to avoid stimuli that developed during tube exchange or any movement of placed SLT. In this case, the severely traumatized right lung required intensive treatment, such as suctioning and applying CPAP; we could not rule out the possibility of right pneumonectomy, it was thought that OLV with BB might be insufficient to provide adequate management during operation and to secure arterial oxygen tension [7,8,9]. For these reasons, we exchanged BB with SLT to DLT after arterial oxygen tension reached at safe level under controlled ventilation with general anesthesia.
In this report, we performed BB placement - a bridging method for changing SLT to DLT. BB placement has some advantages over tube exchange in this patient. This patient was confronted by severe air leakage and hypoxemia, any interruption of spontaneous respiration can aggravate the situation and positive pressure ventilation may further aggravate it. The BB is easily placed to a desired main bronchus under FOB. During BB placement, a joint connector permits sealed introduction of a FOB and a blocker while spontaneous ventilation with 100% oxygen. In addition, 'awake' tube exchange from SLT to DLT is usually not feasible in restless, unstable patients.
As a conclusion, BB can be applied easily for lung separation in chest trauma patients with massive air leakage. This method provides a safer way than double-lumen endotracheal tube because it is not required sedation for tube exchange or interruption of spontaneous ventilation.
References
2. Richter T, Ragaller M. Ventilation in chest trauma. J Emerg Trauma Shock. 2011; 4:251–259. PMID: 21769213.

3. Dodds CP, Hillman KM. Management of massive air leak with asynchronous independent lung ventilation. Intensive Care Med. 1982; 8:287–290. PMID: 6757297.

5. Nishiumi N, Inokuchi S, Oiwa K, Masuda R, Iwazaki M, Inoue H. Diagnosis and treatment of deep pulmonary laceration with intrathoracic hemorrhage from blunt trauma. Ann Thorac Surg. 2010; 89:232–238. PMID: 20103242.

6. Varon AJ, Smith CE. Essentials of truma anesthesia. Cambridge: Cambridge university press;2012. p. 209–226.
7. Campos JH. Lung isolation techniques for patients with difficult airway. Curr Opin Anaesthesiol. 2010; 23:12–17. PMID: 19752725.

8. Chakravarthy M, Jawali V. Differential ventilation with spontaneous respiration for bilateral emphysema. Asian Cardiovasc Thorac Ann. 2007; 15:e35–e37. PMID: 17540979.

9. Cohen E. Management of one-lung ventilation. Anesthesiol Clin North America. 2001; 19:475–495. PMID: 11571903.

Fig. 1
Chest X-ray findings. (A) The initial chest x-ray taken at the emergency department. This film shows pneumothorax on both lungs and a fracture of the left 4th rib. The chest tubes are inserted in both sides and an endotracheal tube is also seen. Right lung remains partally collapsed even though chest tube insertion with under water seal. (B) Chest X-ray findings just before discharge. Except a rib fracture, significant pathologic findings are not seen.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download