Abstract
Background
The present study will focus on the rationale for the use of small tidal volume with 6 cmH2O positive end expiratory pressure (PEEP) with the changes of arterial oxygen tension, plateau airway pressure, and static lung compliance during one lung ventilation for endoscopic thoracic surgery.
Methods
Forty-three patients were intubated with a double-lumen endobronchial tube. After positioning the patients in the lateral decubitus, one-lung ventilation was started with 100% oxygen, tidal volume 10 ml/kg without PEEP; arterial oxygen tension, plateau airway pressure, and static compliance were checked as baseline values (T0). Fifteen minutes later, same parameters were measured (T15). The tidal volume had changed to 6 ml/kg with 6 cmH2O PEEP. Fifteen minutes later, the same parameters were measured (T30).
Results
Oxygen tension had decreased at T15 (282.1 ± 83.4 mmHg) compared to T0 (477.2 ± 82.4 mmHg) (P < 0.0001), but was maintained at T30 (270.4 ± 81.9 mmHg). There was no difference in peak inspiratory pressure at T15 or T30 compared to T0, plateau airway pressure was increased at T15 and T30 (P < 0.05) and static lung compliance was decreased at T15 and T30 (P < 0.0001).
Conclusions
In carrying out one-lung ventilation for thoracic surgery using an endoscope, the addition of a PEEP of 6 cmH2O in the dependent lung, while reducing the tidal volume of 6 ml/kg, both oxygen tension and lung compliance are maintained without increasing the plateau airway pressure. Protective lung ventilation is useful for one lung ventilation.
One lung ventilation (OLV) is widely used, because it secures the surgical view by collapsing a lung in the chest area, but it also causes ventilation-perfusion mismatching and increases intrapulmonary shunt, which leads to increasing the alveolar-arterial oxygen difference, and decreasing the arterial oxygen pressure. Consequently, it has been known that for the prevention and treatment of hypoxemia, positive end expiratory pressure (PEEP) should be given to a dependent lung, and continuous positive airway pressure (CPAP) should be given to an independent lung with an increased fraction of inspired oxygen [1]. However, in the case of endoscopic surgery, continuous pressure on the independent lung limits the surgical view [2]. In addition, in the case of normal lung function, the effects of PEEP on a dependent lung and continuous pressure on the lung in surgery have almost the same effect on oxygenation [3]; it is generally recommended that PEEP is used on a dependent lung. However, the recommended level of PEEP is in a wide range of 5-10 cmH2O [4], and to minimize lung damage during surgery, protective lung ventilation (PLV) has recently been suggested with low tidal volume [5].
Therefore, this research has tried to review the results of the approach in which the level of respiration volume is lowered from 10 ml/kg without any PEEP to 6 ml/kg with 6 cmH2O PEEP during endoscopic lung surgery on the lateral position with OLV. This is to determine whether it improves the level of oxygen tension and lung compliance without increasing the airway pressure.
This research has been approved by Institutional Review Board of the hospital, and the objects and methods of research have been explained to the patients and their escorts.
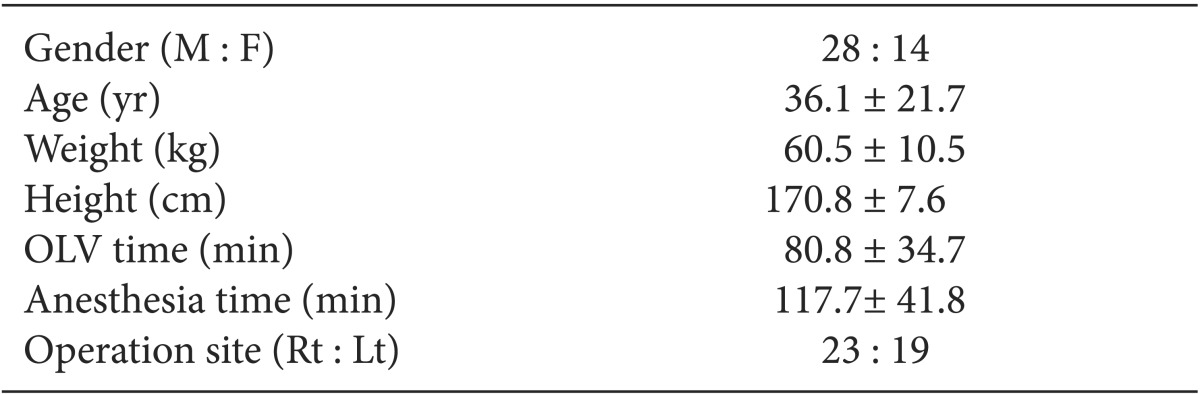
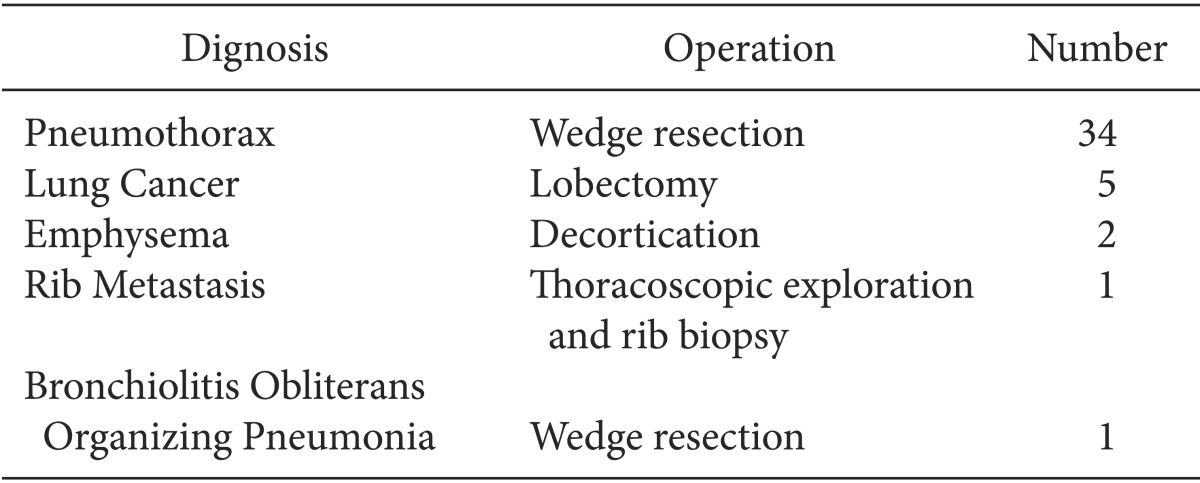
The patients are classified as 1 or 2, according to the physical status classification of the American Society of Anesthesiologists, excluding those with cardiovascular diseases, respiratory diseases or any other systemic disease. The age range is 15-75, and the weight range is 48-78 kg. The gender ratio of men to women is 28 : 14 (Table 1). The population of this research was 43 patients who were supposed to undergo endoscopic thoracic surgery in January-October 2013 (Table 2).
Philips IntelliVue MP70 measured the status of the patients' systolic blood pressure, diastolic blood pressure, mean blood pressure, electrocardiogram, heart rate, and oxygen saturation with a pulse oximeter before anesthetic induction. Then, this research supplied 6 L of oxygen by mask during anesthetic induction.
To cause the loss of consciousness and muscle relaxation, anesthesia induction was conducted with 0.2 mg of glycopyrrolate, 0.06 mg/kg of midazolam, 2 µg/kg of fentanyl, 4 mg/kg of 2.5% thiopental sodium, and 0.6 mg/kg of rocuronium on the condition of 100% oxygen from mask. After confirming the loss of consciousness and muscle relaxation, a left-sided double lumen tube (Covidien-Mallinckrodt™) was intubated (Men: 37 Fr, Women: 35 Fr) to conduct OLV. Then, we inflated the cuff of the trachea and left bronchus, and measured the breath sounds of the patients. Inflation of the bronchial cuff was identified through tracheal lumen by flexible bronchoscopy in carina. Allen test was conducted on the left or right radial artery, and a 22 G arterial catheter was placed.
For the maintenance of anesthesia, from 1.5 to 2.5 vol% of sevoflurane and 4 L/min of oxygen was administered, and extra rocuronium was necessarily used in the case of low muscle relaxation. After changing the patients to a lateral position, we confirmed the position of the double lumen tube by auscultation and flexible bronchoscopy. Ventilation was regulated with a ventilator (Drager CATO edition, Lubeck, Germany) by maintaining 10 mg/kg of tidal volume, and a 8-14 times of respiratory rate for the 30-35 mmHg end-tidal CO2. The I : E ratio was set at 1 : 1.7 and Tip : Ti (%) at 10%. OLV was started, and arterial blood gas analysis was conducted, and peak inspiratory pressure, plateau pressure, and static lung compliance were measured for baseline values (T0), then OLV was conducted for 15 minutes. Tracheal lumen or endobronchial lumen was opened to the collapse of the surgical site, but suction by catheter was not done, and OLV was conducted in the same ventilation setting and then peak inspiratory pressure, plateau pressure, lung compliance, and arterial oxygen tension were measured (T15).
After that, tidal volume was lowered to 6 ml/kg with 6 cm-H2O of PEEP for 15 minutes. We conducted arterial blood and measured gas analysis, peak inspiratory pressure, plateau pressure, and lung compliance again (T30).
At the beginning of anesthetic induction, 10 ml/kg of crystalloid fluid was given. As a limitation, in case the level of oxygen saturation by pulse oximeter dropped under 95 at any time during anesthesia, that experiment would be stopped. Furthermore, any cases of failed collapse are excluded from the results.
This statistical analysis is based on the SPSS program (version 12.0, SPSS Inc, USA), and the comparison of results at the time series was analyzed by repeated measurement analysis of variance and Bonferroni correction. Every result is displayed as a mean ± standard deviation. P values of results under 0.05 were regarded as statistically significant.
Arterial oxygen pressure was recorded as 282.1 ± 83.4 mmHg at T15, and 270.4 ± 81.9 mmHg at T30, compared to 477.2 ± 82.4 mmHg at T0. At T15 and T30, arterial oxygen appeared remarkably decreased (P < 0.001) compared with the T0 comparison between T15 and T30, which has not indicated a meaningful difference (Table 3).
The peak inspiratory pressure was 22.1 ± 4.3 mmHg at T0, 21.7 ± 3.3 mmHg at T15, and 21.6 ± 3.3 mmHg at T30, showing no meaningful change at every point (Table 3).
Plateau pressure at T0 was 18.3 ± 4.0 mmHg, but 19.7 ± 3.1 mmHg and 19.8 ± 3.3 mmHg at each of T15 and T30, showing meaningful increase (P = 0.0349, P = 0.0075). However, the comparison between the cases of T15 and T30 showed no meaningful difference (Table 3).
Lung compliance at T0 was 33.5 ± 7.8 mmHg, 26.5 ± 5.6 mmHg at T15, and 25.7 ± 5.8 mmHg at T30. T15 and T30 cases appeared to be relatively decreased compared to T0, but both T15 and T30 showed no meaningful difference (Table 3).
For years, hypoxemia was considered the most important problem during OLV. Therefore guidelines were published in multiple papers and books, many of them based on the studies by Katz et al. [6], who found that large tidal volumes produced the highest arterial oxygen tension during OLV, leading to the recommendation that tidal volume during OLV should be as high as in two-lung ventilation (8-12 ml/kg). However, the same large tidal volume may have dynamic pulmonary hyperinflation during OLV, and acute lung injury is now known to be a problem after thoracic surgery [7], which may be augmented or ameliorated by the strategies chosen for OLV. Therefore, we tried to review the result of trying to lower the level of respiration volume from 10 ml/kg without any PEEP to 6 ml/kg with 6 cmH2O PEEP during endoscopic lung surgery on a lateral position with OLV, to observe whether it improves the level of oxygen tension and lung compliance without increasing the airway pressure.
Treatment for hypoxemia during OLV is increasing the fraction of inspired oxygen, PEEP on the dependent lung, continuous positive airway pressure on the independent lung, and intermittent ventilation for both lungs. However, surgery using a thoracoscope limits the pressure on independent lung and ventilation with two lungs [2]. In the case of chronic obstructive pulmonary disease patients, auto-PEEP is already formed that CPAP on independent lung is more effective than PEEP on dependent lung. In other case of normal lung condition, PEEP is effective as well as continuous airway pressure on independent [1]. The dependent lung can be collapsed easily when in a lateral position, which can aggravate an imbalance of lung ventilation-perfusion [8]. Therefore, it is reported that PEEP on a dependent lung is favorable for oxygenation [9]. However, previous research studies have indicated that PEEP could improve hypoxemia for patients who show low lung volume and ventilation-perfusion mismatch because of lesions on the dependent lung [10]. For patients whose dependent lung is normal; however, the shunt effect is more favorable than PEEP, according to the statuses of patients on whom the effects of PEEP are limited and difficult to anticipate.
Many research studies have focused on the level of PEEP during OLV to maintain proper oxygenation. Ren et al. [11] insisted that 8 ml/kg tidal volume with 5 cmH2O PEEP is enough for recruiting the dependent lung for patients with normal lung condition, but a 10 cmH2O level of high PEEP is not recommended, with its danger of lung damage from ventilation. Sentürk et al. [9] reported a 4 cmH20 level of low PEEP could also be effective in ventilation with adjusted pressure. Fujiwara et al. [3] reported that 4 cmH2O of PEEP is effective with 10 ml/kg tidal volume. However, Ferrando et al. [12] suggested that with 5-7 ml/kg ventilation volume and maintaining the plateau pressure under 25 cmH2O, adjusted PEEP by patients can improve results more than a flat level PEEP of 5 cmH2O, and suggested that the proper level of PEEP is 10 ± 2 cmH2O. It is reported that normal mammalian tidal volumes are 6.3 ml/kg [6], and a smaller tidal volume of 5-7 ml/kg has been recommended to minimize any mediastinal shift and maximize surgical exposure during videoassisted thoracoscopic surgery [13]. Most PLV protocols also rely on 5-10 cmH2O PEEP to preserve dependent lung unit aeration, prevent atelectasis, and reduce injury from mechanical stress. In this research for OLV, the average plateau pressure showed less than 25 cmH2O in the case of a ventilation volume of 10 ml/kg before PEEP; therefore, we applied 6 cmH2O of PEEP and lowered the tidal volume to 6 ml/kg.
Conducting PEEP to increase oxygenation during OLV is related to hypoxic pulmonary vasoconstriction (HPV) [14]. According to HPV, blood flow in the independent lung decreases from 40-50% to about 25%, which also decreases the shunt-rate, keeps ventilation-perfusion [15], and the effects of HPV could be varied from the duration of OLV [16]. Domino et al. [17] insisted that the reaction of HPV from acute lung collapse due to open thoracic cavity can occurs in 15 minutes, and is maximized at 60 minutes. In particular, in a case with the ventilation of a low-oxygen independent lung, the reaction is maximized in 15 minutes. Therefore, Ren et al. [11] have recommended starting PEEP at the beginning of OLV.
Thoracic surgery should consider all those concerns with hypoxia, overexpansion of lung, and any surgical problems during pulmonary sequestration with double lumen tube in the lateral position. To prevent and treat those problems, we have to recognize the danger of acute lung damage, including barotrauma and volutrauma [18]. In the 1980s, 8-12 ml/kg of huge ventilation volume, which is essential during two-lung ventilation during OLV, was believed to keep a high level of oxygen pressure [19] and was recommended [20]. However, since acute lung damage had been a known consequence of intrathoracic surgery [21], the overexpansion of a lung during OLV has been widely known as one of the reasons of acute lung damage, and PLV has been recommended. PLV is the method keeping the level of ventilation volume under 6 ml/kg with an under 20 cmH2O level of plateau pressure [22]. This method, which was adopted for this research, keeps the ventilation of the dependent lung and conducts PEEP at a 5-10 cmH2O level to reduce the damage from mechanical stresses and atelectasis [23].
The limitations of this research are 1) the duration of OLV is not enough. However, almost-desaturated patients during OLV are observed at 10 minutes [1], while PEEP and PLV are conducted after 15 minutes. 2) Only patients with normal lung condition were in the population; therefore, differences arising from lung diseases were not considered. 3) This research could also try to separate the population into two groups, the first group with only OLV, and the second group with OLV with PEEP and PLV from the start. If this was tried, we could also find the intraoperative and postoperative effects of PLV for OLV.
In conclusion, it is recommended that 6 ml/kg of small tidal volume with 6 cmH2O PEEP at a lateral position with thoracoscopic surgery be conducted for patients without a chronic lung disease, which keeps oxygenation without any changes in airway pressure or static lung compliance.
References
1. Slinger PD, Campos JH. Anesthesia for thoracic surgery. In : Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Young WL, editors. Miller's Anesthesia. 7th ed. Philadelphia: Churchill Livingstone;2010. p. 1851–1853.
2. Grichnik KP, Shaw A. Update on one-lung ventilation : the use of continuous positive airway pressure ventilation and positive endexpirataory pressure ventilation - clinical application. Curr Opin Anaesthesiol. 2009; 22:23–30. PMID: 19295290.
3. Fujiwara M, Abe K, Mashimo T. The effect of positive end-expiratory pressure and continuous positive airway pressure on the oxygenation and shunt fraction during one-lung ventilation with propofol anesthesia. J Clin Anesth. 2001; 13:473–477. PMID: 11704442.

4. Slinger PD, Kruger M, McRae K, Winton T. Relation of the static compliance curve and positive end-expiratory pressure to oxygenation during one-lung ventilation. Anesthesiology. 2001; 95:1096–1102. PMID: 11684977.

5. Slinger PD. Acute lung injury after pulmonary resection: more pieces of the puzzle. Anesth Analg. 2003; 97:1555–1557. PMID: 14633517.

6. Katz JA, Laverne RG, Fairley HB, Thomas AN. Pulmonary oxygen exchange during endobronchial anesthesia: effect of tidal volume and PEEP. Anesthesiology. 1982; 56:164–171. PMID: 7036798.
7. Grichnik KP, D'Amico TA. Acute lung injury and acute respiratory distress syndrome after pulmonary resection. Semin Cardiothorac Vasc Anesth. 2004; 8:317–334. PMID: 15583792.

8. Michelet P, Roch A, Brousse D, D'Journo XB, Bregeon F, Lambert D, et al. Effects of PEEP on oxygenation and respiratory mechanics during one-lung ventilation. Br J Anaesth. 2005; 95:267–273. PMID: 15980044.

9. Sentürk NM, Dilek A, Camci E, Sentürk E, Orhan M, Tuğrul M, et al. Effects of positive end-expiratory pressure on ventilatory and oxygenation parameters during pressure-controlled one-lung ventilation. J Cardiothorac Vasc Anesth. 2005; 19:71–75. PMID: 15747273.
10. Zick G, Elke G, Becher T, Schädler D, Pulletz S, Freitag-Wolf S, et al. Effect of PEEP and tidal volume on ventilation distribution and endexpiratory lung volume: a prospective experimental animal and pilot clinical study. PLoS One. 2013; 8:e72675. PMID: 23991138.

11. Ren Y, Peng ZL, Xue QS, Yu BW. The effect of timing of application of positive end-expiratory pressure on oxygenation during one-lung ventilation. Anaesth Intensive Care. 2008; 36:544–548. PMID: 18714623.

12. Ferrando C, Mugarra A, Gutierrez A, Carbonell JA, Garcia M, Soro M, et al. Setting individualized positive end-expiratory pressure decrement trial after a recruitment maneuver improves oxygenation and lung mechanics during one-lung ventilation. Anesth Analg. 2014; 118:657–665. PMID: 24557111.
13. Sullivan EA. Anesthetic considerations for special thoracic procedures. Thorac Surg Clin. 2005; 15:131–142. PMID: 15707351.

14. Benumof JL, Rogers SN, Moyce PR, Berryhill RE, Wahrenbrock EA, Saidman LJ. Hypoxic pulmonary vasoconstriction and regional and whole-lung PEEP in the dog. Anesthesiology. 1979; 51:503–507. PMID: 391103.

15. Benumof JL. One-lung ventilation and hypoxic pulmonary vasoconstriction: implications for anesthetic management. Anesth Analg. 1985; 64:821–833. PMID: 3893223.
16. Ishikawa S, Makita K, Nakazawa K, Amaha K. Continuous intra-arterial blood gas monitoring during oesophagectomy. Can J Anaesth. 1998; 45:273–276. PMID: 9579269.

17. Domino KB, Chen L, Alexander CM, Williams JJ, Marshall C, Marshall BE. Time course and responses of sustained hypoxic pulmonary vasoconstriction in the dog. Anesthesiology. 1984; 60:562–566. PMID: 6731911.

18. Grichnik KP, Shaw A. Update on one-lung ventilation: the use of continuous positive airway pressure ventilation and positive end-expiratory pressure ventilation-clinical application. Curr Opin Anaesthesiol. 2009; 22:23–30. PMID: 19295290.
19. Katz JA, Laverne RG, Fairley HB, Thomas AN. Pulmonary oxygen exchange during endobronchial anesthesia: effect of tidal volume and PEEP. Anesthesiology. 1982; 56:164–171. PMID: 7036798.
20. Brodsky JB, Fitzmaurice B. Modern anesthetic techniques for thoracic operations. World J Surg. 2001; 25:162–166. PMID: 11338017.
21. Grichnik KP, D'Amico TA. Acute lung injury and acute respiratory distress syndrome after pulmonary resection. Semin Cardiothorac Vasc Anesth. 2004; 8:317–334. PMID: 15583792.

22. Schultz MJ, Haitsma JJ, Slutsky AS, Gajic O. What tidal volume should be used in patients without acute lung injury? Anesthesiology. 2007; 106:1226–1231. PMID: 17525599.
23. Lytle FT, Brown DR. Appropriate ventilatory settings for thoracic surgery: intraoperative and postoperative. Semin Cardiothorac Vasc Anesth. 2008; 12:97–108. PMID: 18635561.

Table 3
Time Course Changes
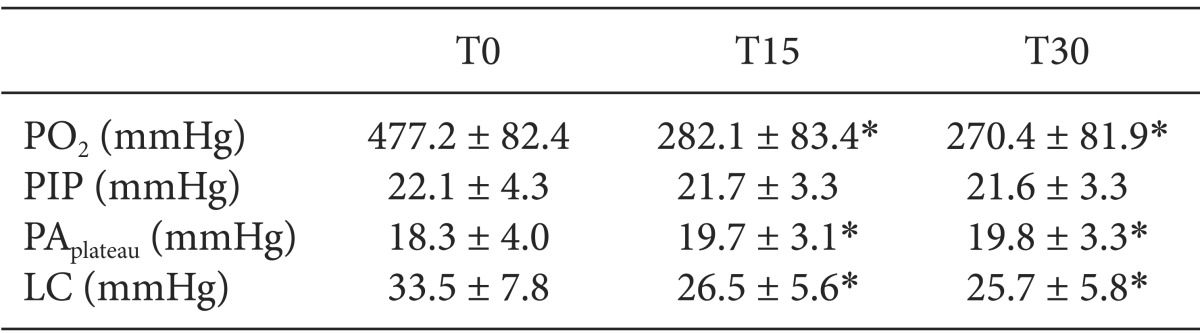
Data are means ± SD. T0: One-lung ventilation started with 100% oxygen. T15: tidal volume 10 ml/kg and PEEP 0. 15 minutes later. T30: tidal volume 6 ml/kg and PEEP 6 cmH2O. 15 minutes later. PO2: Partial pressure of oxygen, PIP: Peak inspiration pressure, PAplateau: Plateau airway pressure, LC: Lung compliance. *Significantly different (P < 0.05) from T0.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download