We began this study after receiving approval from the Institutional Review Board of our hospital and obtaining informed consent from all the patients. Twenty-seven patients who were classified as American Society of Anesthesiologists physical status 1 and 2 and underwent thoracic surgery in the lateral decubitus position with at least 1 h OLV were enrolled (
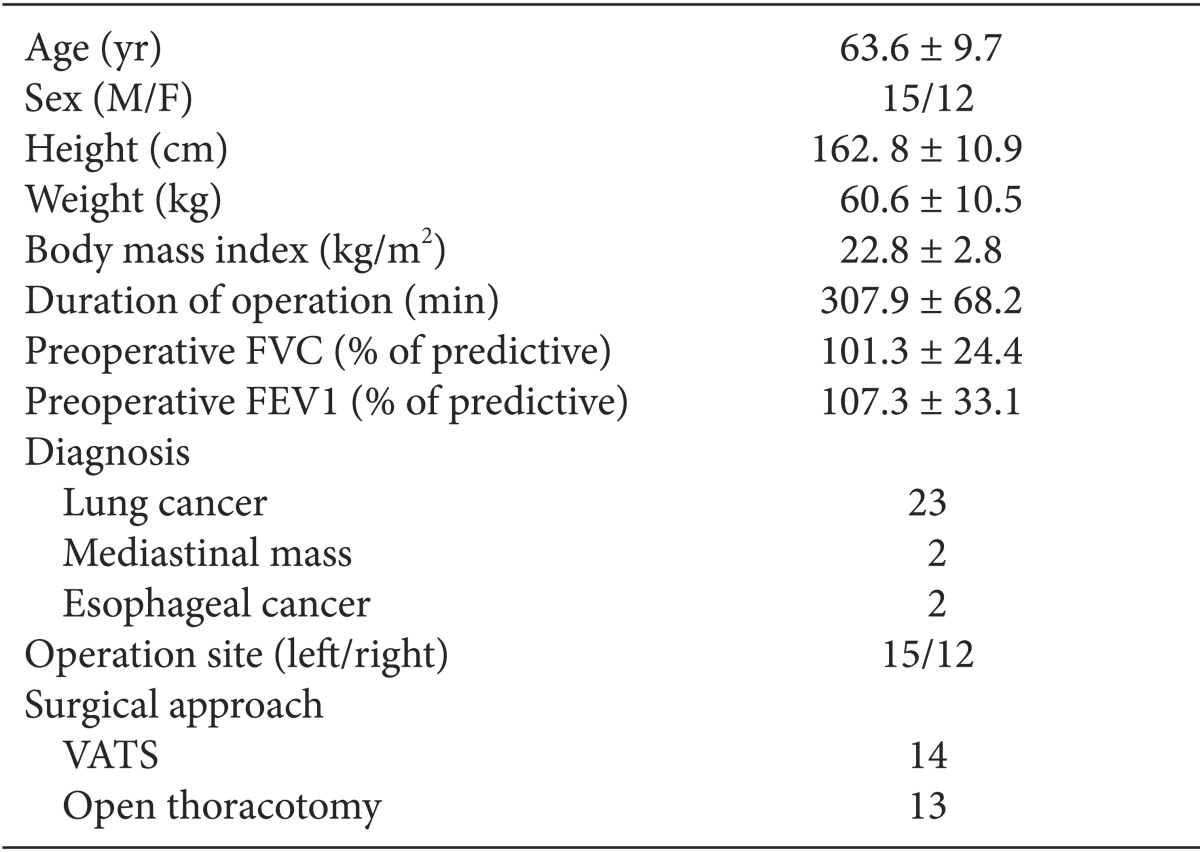
Table 1,
Fig. 1). The exclusion criteria were previous lobectomy, uncompensated cardiac disease, tracheostomy state, and predicted forced expiratory volume in 1 second (FEV1) below 70%. All patients were intramuscularly injected with 0.2 mg glycopyrrolate and 1 mg midazolam as premedication 30 min before arriving in the operating room. The patients were furnished with electrocardiogram (ECG), noninvasive blood pressure, pulse oximetry, and bispectral index (BIS) monitoring equipment before the induction of anesthesia. Anesthesia was induced and maintained with an effect-site concentration of 4 µg/ml propofol and 4 ng/ml remifentanil using target controlled infusion (TCI). After loss of consciousness, 0.6 mg/kg rocuronium was administered for intubation, and 0.08 mg/kg/hr vecuronium infusion was followed 30 min after intubation. All patients were intubated with a double-lumen endobronchial tube (DLT, Silbroncho®, Fuji System Corp, Tokyo, Japan), and the proper position of the DLT was confirmed using a fiberoptic bronchoscope. All of the patients were intubated with left-side DLT if there was no contraindication. After intubation, a radial artery cannulation was performed on the contralateral side arm of the operation, and a central venous catheter was placed in the ipsilateral subclavian vein. Initially, two-lung ventilation with VCV was performed using 1.0 fraction of inspired oxygen concentration (FiO
2), a TV of 8 ml/kg of actual body weight, and 12 /min respiration rate. The respiration rate was adjusted to maintain an end-tidal carbon dioxide concentration (ETCO
2) of 35-40 mmHg. After changing the patient to a lateral decubitus position, the location of the DLT was reassessed with a fiberoptic bronchoscope. OLV was subsequently performed with VCV or PCV-VG (Avance, GE healthcare, Wauwatosa, WI, USA) according to an allocation sequence. An independent statistician randomized the ventilation sequence using a computerized random number generator. VCV was set to deliver a TV of 8 ml/kg of actual body weight without positive end-expiratory pressure (PEEP), and the respiration rate was adjusted to maintain an ETCO
2 of 35-40 mmHg using 1.0 FiO
2. The maximum airway pressure (P
max), at which time the ventilator will alarm and end inspiration, was adjusted to 40 cmH
2O. An inspiration to expiration ratio of 1 : 2 was used, and no inspiratory time pause was used. PCV-VG was performed using 1.0 FiO
2, a TV of 8 ml/kg of actual body weight without PEEP, 40 cmH
2O P
max, and an inspiration to expiration ratio of 1 : 2; the respiration rate was adjusted to maintain an ETCO
2 of 35-40 mmHg. The rise rate, which indicates how quickly the ventilator reaches the targeted airway pressure, was adjusted to 5 sec. In the PCV-VG mode, the present anesthetic machine delivers the first breath to the patient using a VCV setting to identify the patient's lung compliance, and then the inspiratory pressure level is automatically calculated and determined for the subsequent breaths in the PCV-VG setting. The P
peak, mean inspiratory pressure (P
mean), TV
E, systolic and diastolic blood pressures (SBP, DBP), heart rate (HR), arterial oxygen tension (PaO
2), and arterial carbon dioxide tension (PaCO
2) were measured and recorded after performing each mode of mechanical ventilation for 30 min in the lateral decubitus position. Afterwards, the ventilation was changed to another mode and maintained until the surgery was completed. When the ventilation mode was changed from VCV to PCV-VG or from PCV-VG to VCV 30 min after OLV, the TV and respiration rate of the previous mode were maintained. Thirty minutes after changing the ventilation mode, all measurements were performed again. When the peripheral oxygen saturation (SpO
2) decreased below 90% or PaO
2 decreased below 80 mmHg, both of which are defined as hypoxemia, the experiment was terminated. When hypoxemia occurred, two-lung ventilation with 1.0 FiO
2 was performed, and the patient was excluded from this study. Hypoxemia was treated according to standard hypoxemia treatment protocols, including DLT position readjustment using a fiberoptic bronchoscope, lung recruitment maneuver, change of TV, and the application of PEEP or continuous positive airway pressure.
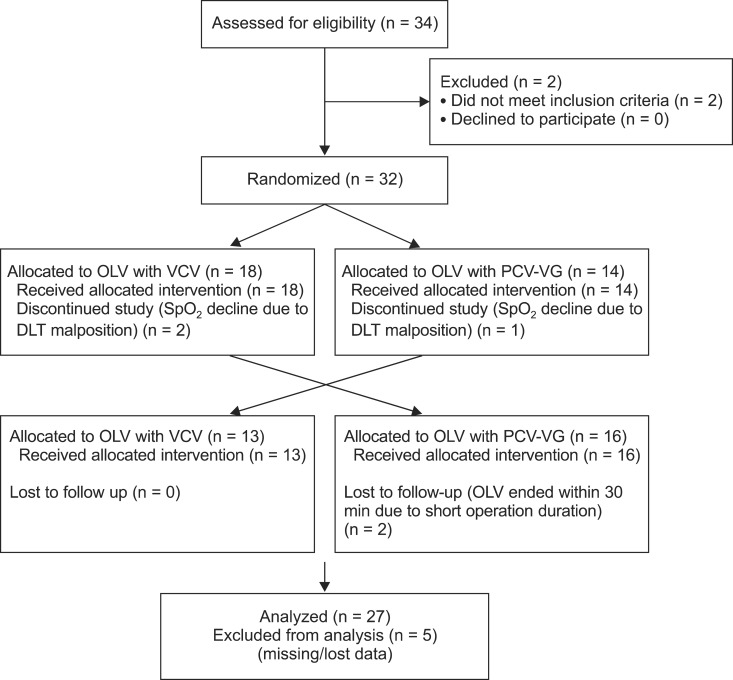 | Fig. 1Consort diagram depicts the flow of participants. 
|
Table 1