Abstract
Background
Infrequent but serious complications of transforaminal epidural steroid injection (TFESI) occur due to inadvertent intravascular injections. A few studies reported that the different needle types can influence on the occurrences of intravascular incidence in TFESI. This study prospectively evaluated whether short-bevel needle can reduce the incidences of intravascular injection of TFESI compared to long-bevel needles.
Methods
From March 2013 to December 2013, 239 consecutive patients were enrolled and received 249 fluoroscopically guided TFESI using the classic technique. Confirmation of intravascular spread was done initially with real time fluoroscopy and then with digital subtraction angiography method in a same patient. Injection technique for TFESI was the same for both short-bevel and long-bevel needle types.
Results
The incidences of intravascular injections with the long-bevel and short-bevel needles were 15.0% (21/140) and 9.2% (4/140), respectively. More than half of intravascular injections occurred simultaneously with epidural injections (8.0%, 20/249). There were no statistically significant differences between the long-bevel and the short-bevel needles in the rates of intravascular injections (P = 0.17).
Go to : 
Many pain physicians prefer transforaminal epidural steroid injection (TFESI) due to its advantage of the delivering high concentration of medication to the ventral epidural space, which contains a lot of painful substances. However, we should remember that this procedure accompanies minor to devastating complications [1]. Rare but serious morbidity has also been reported, which includes spinal cord infarction, subdural hematoma, paraplegia, qudriparesis, and even death [2,3,4,5,6]. These serious outcomes are secondary to inadvertent intravascular injections or the embolization of corticosteroid particulates via the vertebral or radicular arteries [2,5,6,7].
The incidence of intravascular injections has been reported to be 8.5 to 13.1% of the fluoroscopically guided lumbar TFESI, depending on the level of injection [8,9,10].There is several traditional methods to confirm intravascular penetration. Widely used aspiration test or blood in the needle hub (flash) has a very low sensitivity compared to live fluoroscopy [8,11,12].
Thorough understanding of the associated factors is essential; however, there is only a limited amount of information about them. Nahm et al. [13] and Kim et al. [14] reported that the incidence of vascular injection was significantly increased with cervical and sacral level of injections. Özcan et al. [15] reported that using the blunt needles can reduce the intravascular injection and paresthesia during TFESI. Also, animal studies have demonstrated that the blunt needles are less likely than sharp needles to puncture the vital structures including blood vessels [16]. However, Smuck et al. [17] reported that the short-bevel needles did not reduce the risk of intravascular injection in lumbar TFESI, compared to long-bevel needles.
The physicians' preferences between the short and long-bevel needles are influenced by their usability and the safety concerns. The short-bevel needles can provide the steering and tissue penetrating advantages of the long-bevel needles, with potentially lower risk of damaging other tissues [17].
In this study, we compared the incidence of intravascular injections between the long-bevel and the short-bevel needles.
Go to : 
This study was approved by the ethics committee of our institution, and the written informed consent was obtained from all patients after explaining the risks, benefits, and goals of this study. From March 2013 to December 2013, 239 consecutive patients were enrolled and received 249 fluoroscopically guided TFESI using the classic technique.
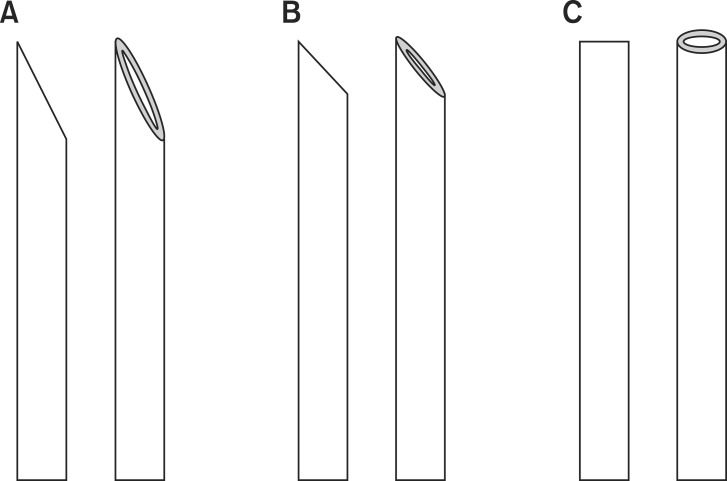
Chiba needle (35°) and Quincke needle (20°) have different bevel angles, so they can be used as good examples of the short-bevel (25-gauge, 9 cm) and the long-bevel needles (25-gauge, 9 cm), respectively (Fig. 1).
Ten patients received 2 level TFESI and the remaining 229 patients received 1 level TFESI. The 2 level TFESI was performed on the same side, using two types of needles. According to a concealed random number table, a needle was selected just before TFESI after sterile preparation. Injection technique for TFESI was the same for both long-bevel and short-bevel needle types.
Inclusion criteria were patients who had low back pain with or without leg pain from spinal stenosis, herniated nucleus pulposus, compression fracture, and failed back surgery syndrome. Exclusion criteria were patients who have known allergies to contrast or local anesthetics or who had experienced coagulopathy. Also, the patients who received either interlaminar or caudal epidural injections were excluded.
All TFESI were performed during the outpatient care by one of the authors of this study, who has more than 8 years of experience in interventional pain management. The patients were prepared and draped in a sterile fashion in a prone position. Using the classic method for TFESI, the injection target was the six-o'clock position of the pedicle in the AP projection. The targeted segmental level was identified under intermittent fluoroscopy, and the inferior endplate was aligned by tilting the C-arm craniocaudally. Then, the C-arm was rotated obliquely to ensure injection at the neural foramen. The skin entry site was infiltrated with 1% lidocaine, and 25-gauge long-bevel or short-bevel spinal needle was advanced under intermittent fluoroscopy toward the six-o'clock position of the pedicle, avoiding the segmental nerve and intervertebral disc. Lateral radiographic imaging was also used, while advancing toward the intervertebral foramen and superolateral to the exiting spinal nerve with a special attention to minimize the risk of disc puncture. Up to 3 ml of contrast dye (Omnipaque 300, GE Healthcare, Little Chalfont, Buckinghamshire, UK) was used to confirm the successful epidural spread. First, to confirm intravascular spread, 1.5 ml of nonionic contrast was injected under the real-time fluoroscopy and was checked for any inadvertent intravascular spread. Subsequently, additional 1.5 ml of nonionic contrast was injected and the digital subtraction angiography (DSA) method was applied to confirm intravascular spread once again. Before going to the DSA mode, we asked the patient to hold their breath for few seconds to obtain adequately subtracted image. After confirmation of the successful epidural contrast spread without appearance of any inadvertent intravascular spread, a mixture of 5 mg of dexamethasone and 3 ml of 0.5% mepivacaine was injected.
In the cases of observed inadvertent intravascular injections, the needle repositioning was repeated two or three times as necessary. If the vascular contrast pattern remained, the needle tip was withdrawn slowly and repositioned more superiorly or inferiorly within the neural foramen. When an intravascular injection was unavoidable in spite of the repeated attempts of needle repositioning, injecting any medication at this level was abandoned.
The observed patterns through the real-time and DSA images were recorded as one of the following categories: epidural, epidural and vascular, or vascular. If the contrast showed a characteristic of fleeting pattern and immediately disappeared without epidural spread, the injection was considered intravascular. If the contrast showed a transient fleeting pattern as well as epidural spread, the injection was recorded as vascular and epidural. In both cases of vascular and vascular/epidural, the needle was repositioned to avoid the intravascular injection of the steroid. The assessments were made for each injection by the practicing physician, and then were confirmed once again by assessment of the stored images.
Data were collected on the patients' age, sex, type of the disease, presence of vascular spread of contrast on real-time fluoroscopic images, DSA, and spinal levels where TFESI was performed. We hypothesized after reviewing other related articles that the probability of vascular injections of contrast would be 15%, [8,9,10,11,12,13,17,18]. Based on an α error level of 0.05, a β error level of 0.2, and a two-sided test, 234 injections were required as a total sample size with 80% power. All statistical analyses were performed using chi-square test and Fisher exact test with SPSS version 17.0 (SPSS, Chicago, IL, USA).
Go to : 
A total of 249 TFESI were performed on 239 patients with the mean age of 62.5 years (range: 26-90 years).
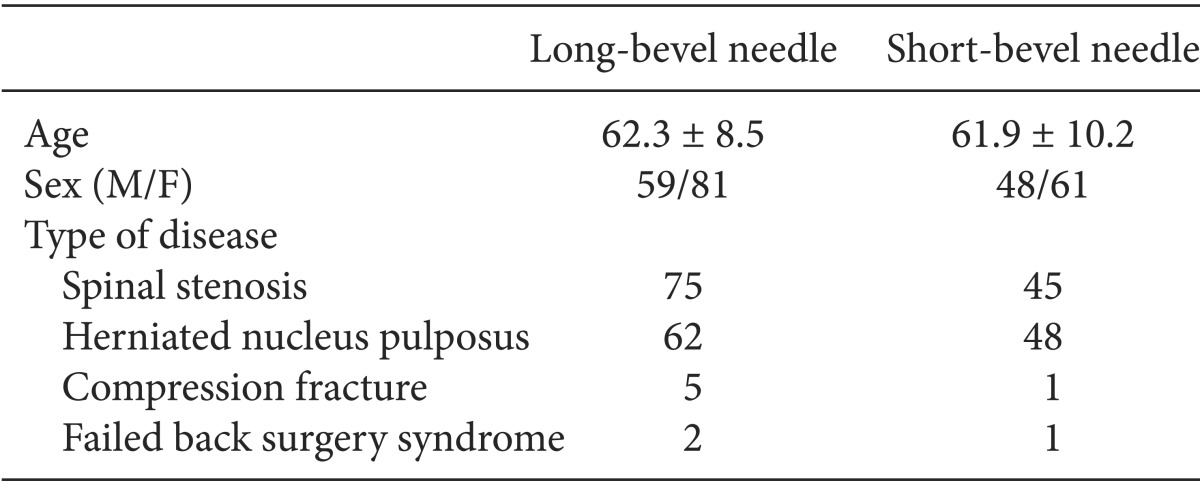
Ten patients received 2 level TFESI and the remaining 229 patients received 1 level TFESI. Among those injections, 110 cases were performed on the right-sides and 139 cases were performed on the left-sides. One hundred twenty patients were diagnosed with spinal stenosis, 110 patients with herniation of nucleus pulposus, 6 patients with compression fracture, and 3 patients with failed back surgery syndrome (Table 1).
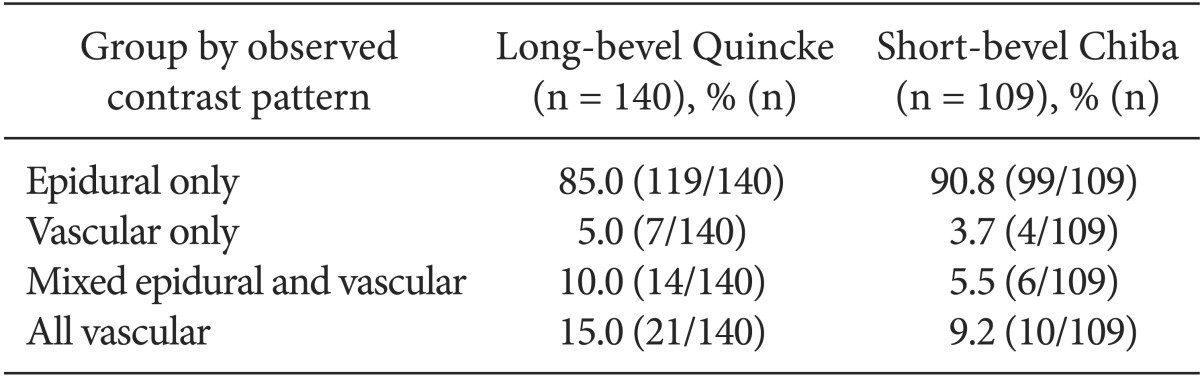
TFESI were performed from L1 to S1 spinal levels. The incidence of overall intravascular injections was 12.4% (31/249) (Table 2).
The injections were also divided into two groups based on the needle types used: long-bevel needles (n = 140) or short-bevel needles (n = 109). The incidences of intravascular injections with the long-bevel and short-bevel needles were 15.0% (21/140) and 9.2% (4/140), respectively. More than half of intravascular injections occurred simultaneously with epidural injections (8.0%, 20/249). There were no statistically significant differences between the needle groups in the rates of intravascular injections (P = 0.17) (Table 3).
Go to : 
Our results showed decreased incidence of intravascular injections with short-bevel Chiba needle (9.2%) compared to long-bevel Quincke needle (15.0%). However, this difference did not reach the statistical significance. The morphological difference in bevel angles, between the long-bevel and short-bevel needles, did not affect the incidence of intravascular injections. In contrast to our results, blunt needle seems to have benefit in reducing the incidence of intravascular injections. And Özcan et al. [15] reported that less vascular penetration and paresthesia occurred when blunt needles were used instead of the sharp needles, during TFESI.
Smuck et al. [17] concluded that in comparison to the long-bevel needles, the short-bevel needles did not reduce the risk of inadvertent vascular injection in lumbosacral TFESI.
Shin et al. [19] compared the intravascular injection rates between Quincke and Whitacre needle types, and they concluded that Quincke needle type demonstrated significantly higher intravascular rate (24.9%) compared to Whitacre needle type (16.7%). Since their study was performed in only S1 TFESI, which is known to have higher incidence of intravascular injections compared to the lumbar area [20,21], the difference of intravascular incidence between the two needle types might be much larger.
The block needles are labeled as blunt or sharp needle types. The short and long-bevel needles belong to the sharp needle type, with different angles of bevel as described previously (20 degrees for long-bevel and 35 degrees for short-bevel) [17]. We expected the short-bevel needle to be more beneficial in reducing the tissue damage, including the inadvertent intravascular injection. However, this study did not demonstrate any benefits of using short-bevel needle in reducing the incidence of intravascular injections. On the contrary, the short-bevel needles provided technical disadvantage, when using as a guide needle during some cases of the TFESI where it is required to puncture the skin and ligament. The blunt needles have been used restrictively due to several drawbacks. In contrast to the sharp needles, the blunt needles do not have any bevel; therefore, we cannot use the steering technique with this needle to reach the target structure [15]. In addition, they are difficult to penetrate through the skin, ligaments, and other fibrous dense tissues during spine procedures.
Smuck et al. [10] reported that most of the intravascular injections during TFESI were appearing simultaneously as both epidural and vascular contrast injection. Accordingly, our result also demonstrated that more than half of the intravascular injections occurred with simultaneous patterns. This pattern of intravascular injection is what leads to the inaccuracy of the realtime fluoroscopy. We used the method of DSA technique, to overcome this inaccuracy of the real-time fluoroscopy.
El Abd et al. [18] reported that the confirmation of intravascular injection with DSA increased the detection rate of vascular puncture. DSA detected additional 5.26% of the intravascular needle placements, following the traditional methods. Theoretically, DSA might enhance the detections of intravascular injections when veins overlie bony structures, distorted by compression fracture or cement, following a surgery. Subtracting the preinjection image from the postinjection image removes most of the bony architecture. This subtracted image can highlight the distribution of an epidurogram and intravascular injection more clearly [14,20]. The disadvantages of DSA includes additional radiation exposure to the patients and the medical staffs, and the high cost of the new and upgraded fluoroscopic equipment [20,21].
Our study includes several limitations. The physician who performed the TFESI made confirmations of the intravascular injections, and we reassessed the intravascular injections using the stored images after the procedures were finished. However, bias cannot be absolutely excluded. In addition, the physician performing TFESI was not blinded to the type of needle being used. When calculating for the proper sample size, we used the overall incidence of intravascular injections rather than the incidence based on different needle type. Therefore, a relatively small sample size might have affected the incidence rates.
In conclusion, short-bevel needles did not demonstrate any benefits in reducing the incidence of intravascular injections.
Go to : 
References
1. Cohen SP, Bicket MC, Jamison D, Wilkinson I, Rathmell JP. Epidural steroids: a comprehensive, evidence-based review. Reg Anesth Pain Med. 2013; 38:175–200. PMID: 23598728.
2. Kennedy DJ, Dreyfuss P, Aprill CN, Bogduk N. Paraplegia following image-guided transforaminal lumbar spine epidural steroid injection: two case reports. Pain Med. 2009; 10:1389–1394. PMID: 19863744.

3. Houten JK, Errico TJ. Paraplegia after lumbosacral nerve root block: report of three cases. Spine J. 2002; 2:70–75. PMID: 14588291.
4. Bose B. Quadriparesis following cervical epidural steroid injections: case report and review of the literature. Spine J. 2005; 5:558–563. PMID: 16153586.

5. McLain RF, Fry M, Hecht ST. Transient paralysis associated with epidural steroid injection. J Spinal Disord. 1997; 10:441–444. PMID: 9355063.

6. Reitman CA, Watters W 3rd. Subdural hematoma after cervical epidural steroid injection. Spine (Phila Pa 1976). 2002; 27:E174–E176. PMID: 11884923.

7. Baker R, Dreyfuss P, Mercer S, Bogduk N. Cervical transforaminal injection of corticosteroids into a radicular artery: a possible mechanism for spinal cord injury. Pain. 2003; 103:211–215. PMID: 12749976.

8. Furman MB, O'Brien EM, Zgleszewski TM. Incidence of intravascular penetration in transforaminal lumbosacral epidural steroid injections. Spine (Phila Pa 1976). 2000; 25:2628–2632. PMID: 11034648.

9. Sullivan WJ, Willick SE, Chira-Adisai W, Zuhosky J, Tyburski M, Dreyfuss P, et al. Incidence of intravascular uptake in lumbar spinal injection procedures. Spine (Phila Pa 1976). 2000; 25:481–486. PMID: 10707395.

10. Smuck M, Fuller BJ, Yoder B, Huerta J. Incidence of simultaneous epidural and vascular injection during lumbosacral transforaminal epidural injections. Spine J. 2007; 7:79–82. PMID: 17197337.

11. Lee CJ, Kim YC, Shin JH, Nahm FS, Lee HM, Choi YS, et al. Intravascular injection in lumbar medial branch block: a prospective evaluation of 1433 injections. Anesth Analg. 2008; 106:1274–1278. PMID: 18349205.

12. Furman MB, Giovanniello MT, O'Brien EM. Incidence of intravascular penetration in transforaminal cervical epidural steroid injections. Spine (Phila Pa 1976). 2003; 28:21–25. PMID: 12544950.

13. Nahm FS, Lee CJ, Lee SH, Kim TH, Sim WS, Cho HS, et al. Risk of intravascular injection in transforaminal epidural injections. Anaesthesia. 2010; 65:917–921. PMID: 20645947.
14. Kim YH, Park HJ, Moon DE. Rates of lumbosacral transforaminal injections interpreted as intravascular: fluoroscopy alone or with digital subtraction. Anaesthesia. 2013; 68:1120–1123. PMID: 23937540.

15. Özcan U, Şahin Ş, Gurbet A, Türker G, Özgür M, Çelebi S. Comparison of blunt and sharp needles for transforaminal epidural steroid injections. Agri. 2012; 24:85–89. PMID: 22865493.

16. Heavner JE, Racz GB, Jenigiri B, Lehman T, Day MR. Sharp versus blunt needle: a comparative study of penetration of internal structures and bleeding in dogs. Pain Pract. 2003; 3:226–231. PMID: 17147672.

17. Smuck M, Yu AJ, Tang CT, Zemper E. Influence of needle type on the incidence of intravascular injection during transforaminal epidural injections: a comparison of short-bevel and long-bevel needles. Spine J. 2010; 10:367–371. PMID: 20171936.

18. El Abd O, Amadera JE, Pimentel DC, Pimentel TS. Intravascular flow detection during transforaminal epidural injections: a prospective assessment. Pain Physician. 2014; 17:21–27. PMID: 24452642.
19. Shin J, Kim YC, Lee SC, Kim JH. A comparison of Quincke and Whitacre needles with respect to risk of intravascular uptake in S1 transforaminal epidural steroid injections: a randomized trial of 1376 cases. Anesth Analg. 2013; 117:1241–1247. PMID: 24047591.
20. Lee MH, Yang KS, Kim YH, Jung HD, Lim SJ, Moon DE. Accuracy of live fluoroscopy to detect intravascular injection during lumbar transforaminal epidural injections. Korean J Pain. 2010; 23:18–23. PMID: 20552068.

21. McLean JP, Sigler JD, Plastaras CT, Garvan CW, Rittenberg JD. The rate of detection of intravascular injection in cervical transforaminal epidural steroid injections with and without digital subtraction angiography. PM R. 2009; 1:636–642. PMID: 19627957.

Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download