Abstract
Background
Rocuronium has been well known to produce withdrawal response in 50-80% patients when administered intravenously. Several drugs are administered prior injection of rocuronium to prevent the withdrawal response. We compared the preventive effect of lidocaine, ketamine, and remifentanil on the withdrawal response of rocuronium.
Methods
A total of 120 patients undergoing various elective surgeries were enrolled. Patients were allocated into 4 groups according to the pretreatment drugs (Group N, normal saline; Groups L, lidocaine 40 mg; Group K, ketamine 0.5 mg/kg; Group R, remifentanil 1 µg/kg). Patients received drugs prepared by dilution to 3 ml volume before injection of rocuronium. Withdrawal responses after injection of rocuronium were graded on a 4-point scale. Hemodynamic changes were observed before and after administration of pretreatment drugs and after endotracheal intubation.
Results
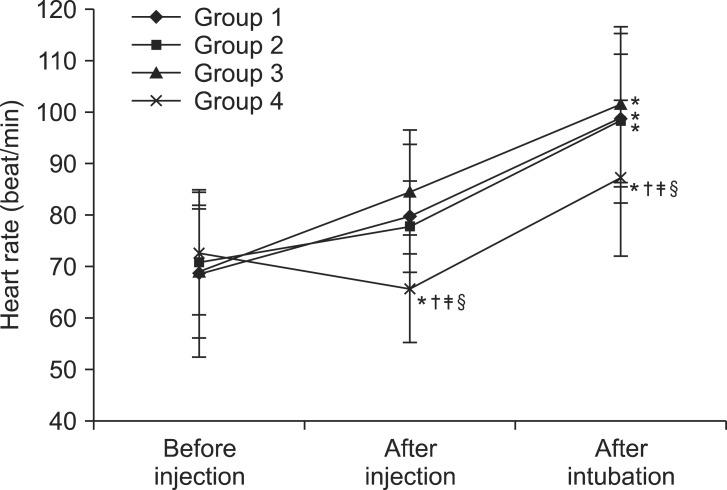
Incidence of withdrawal response was significantly lower in group L (20%), group K (30%), and group R (0%), than group N (87%). Severe withdrawal response was observed in 5 of the 30 patients (17%) in group L, and in 9 of the 30 patients (30%) in group K. There was no severe withdrawal response in group R. Mean blood pressure and heart rate were significantly decreased in group R compared to other groups.
Rocuronium is the most popular neuromuscular blocking agent because of rapid onset, relatively short duration of action, and less adverse effects on hepatobiliary system or autonomic system [1]. It produces sudden flexion movement on injection as a response to a pain [2]. The withdrawal response is a body reaction due to the pain in unconsciousness [3].
Therefore, drugs such as fentanyl, lidocaine, ketamine, remifentanil, tramadol, parecoxib, magnesium sulfate, and ondansetron have been introduced as a pretreatment to prevent the withdrawal response of rocuronium [4]. It has been reported that pretreatment of lidocaine 40 mg successfully reduces injection pain of rocuronium [5,6]. Ketamine (0.5 mg/kg intravenously) also effectively reduces injection pain without mental symptoms such as hallucination before injection of rocuronium [7,8]. Remifentanil (1.0 µg/kg) pretreatment, frequently used during induction of the anesthesia to improve intubation condition and reduce hemodynamic change, also prevents withdrawal response of rocuronium successfully [1].
According to the meta-analysis, opioids, lidocaine, and ketamine have been most frequently used as pretreatment to reduce injection pain of rocuronium [4]. Even though meta-analyses have been performed to compare the preventive effect of withdrawal responses to each drugs, it is an indirect comparison of numerous methods and dosages of pretreatment [4]. In addition, no clinical reports have directly compared the preventive effect of intravenous lidocaine, ketamine, and remifentanil on withdrawal response of rocuronium at an effective dose. Direct comparison can be helpful in the clinical setting, and it could be meaningful to identify which drug is the most effective when administered under the same condition. Therefore, we carried out the study to determine which drug had the most superior effect to reduce withdrawal response of rocuronium.
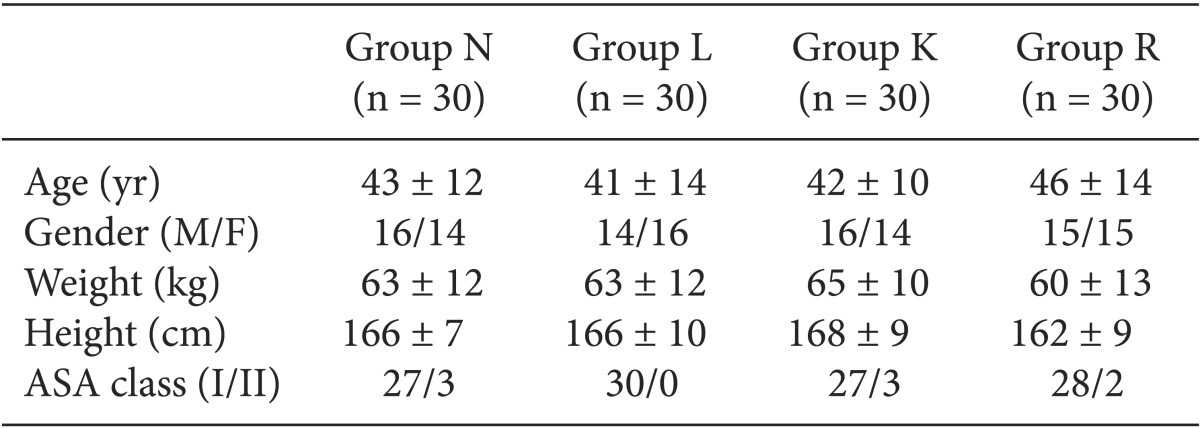
The study was conducted after approval by the Institutional Review Board. A total of 120 patients who were scheduled for elective surgery, aged 20 to 60 years, and American Society of Anesthesiologists class I or II were enrolled. Exclusion criteria were as follows: poor venous access, diabetes, allergies to anesthetic medications, neurologic deficit, psychiatric disorder, vasculitis, thrombosis, prior administration of analgesics within 24 hours, or pregnancy. Informed consent was obtained from all patients after full explanation of aim and method of the study and they were randomized into 3 groups according to pretreatment drugs through a computerized randomization. Patients in group N constituted the control group and received normal saline before injection of rocuronium. Those in group L, group K, and group R received lidocaine 40 mg, ketamine 0.5 mg/kg, and remifentanil 1 µg/kg, respectively [1,5,7]. The dosages of each group were selected from several published reports in which the drugs were administered intravenously and showed most effectiveness in preventing pain response after injection of rocuronium.
All patients received midazolam 0.05 mg/kg intramuscularly 30 minutes before the induction of anesthesia. An 18 gauge venous cannula was kept at the main cephalic vein of the forearm which is proximal to the hand for the infusion of lactated Ringer's solution. After arrival at the operating room, standard monitoring devices such as electrocardiogram, pulse oximetry, and non-invasive blood pressure were attached to the patients. Preoxygenation with a facemask was applied for 5 min before the induction of anesthesia.
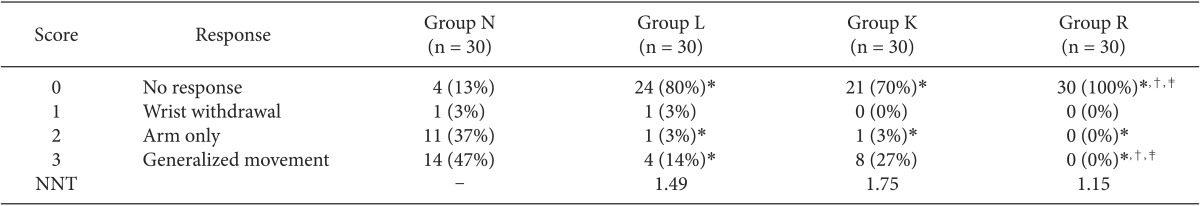
Thiopental sodium (2.5%, 5 mg/kg) was injected for the loss of consciousness, and then ventilation with face mask was started. During ventilation, pretreatment drug was administered intravenously according to the groups. All drugs were diluted to a volume of 3 ml by an assistant nurse who had not participated during the induction of anesthesia for the double blind test. Each drug was administered during 15 seconds by another assistant nurse. Muscle rigidity which was defined as difficult ventilation with face mask due to increased tone of the trunk muscles and opioid induced cough was observed in the case of remifentanil injection. If severe muscle rigidity or cough occurred, the patient was dropped out and rocuronium (1.0 mg/kg) has administered immediately for the rapid sequence intubation. One minute after injection of the pretreatment drug, rocuronium (0.6 mg/kg) was administered for 10 seconds. The 4-point scale was used to assess the severity of withdrawal response during rocuronium injection (Table 1) [9]. Severe withdrawal responses were considered as the response > 2 on the 4-point scale.
After injection of rocuronium, patients were ventilated with sevoflurane 2.5 vol% and 100% oxygen. Endotracheal intubation was done 2 minutes after rocuronium injection. Anesthesia was maintained with sevoflurane (2-4 vol% of end tidal concentration) with O2/N2O mixture (FiO2 = 0.5). Mean blood pressure and heart rate were measured according to the time sequence. Each measurement was done 1 minute before (control) and after the administration of pretreatment drug and 1 minute after endotracheal intubation.
Focal reactions such as erythema, vasculitis, and thrombosis were also observed during the procedure.
Sample size was calculated based on previous studies. The incidences of disappearance of withdrawal response or pain were 75, 60, and 100% after pretreatment with lidocaine [5], ketamine [7], and remifentanil [1], respectively. Sample size was calculated using G*Power software (ver. 3.1.5) which was based on the results of previous studies [1,5,7]. According to the analysis of variance, within-group standard deviation between 4 groups was 0.354 and effect size from variance was 0.437. Using α = 0.05 with a power 90%, the minimum sample size was predetermined as 24 patients per group. After considering drop-out rate as 20%, we included 30 patients in each group.
Statistical analysis was done with SPSS 12.0 (SPSS, Chicago, IL, USA). Incidence of withdrawal response was expressed with number (%) and other data were expressed as mean ± standard deviation (SD). Demographic data were analyzed by ANOVA. Gender and weight which were non-parametrically distributed were analyzed by Kruskal Wallis test. The incidence of withdrawal response and 4-point scale were analyzed by the Chi-square test. P < 0.00833 was considered statistically significant accounting for the Bonferroni correction. Hemodynamic changes were analyzed by repeat measures ANOVA, and when between-group differences were observed, Mann-Whitney U test was used to analyze between pairs of group. Post hoc tests were done with Turkey's HSD. P < 0.05 was considered statistically significant.
There were no dropouts and the data from all 120 patients could be analyzed. There were no significant differences among the groups in demographic data (Table 1).
The incidence of withdrawal response was 87% (26/30), 20% (6/30), 30% (9/30), and 0% in group N, group L, group K, and group R, respectively (Table 2). Severe withdrawal response which is >2 on the 4-point scale occurred in 25 patients (84%) in group N (P < 0.00833). However, it was observed in 5 patients (17%) in group L, in 9 patients (30%) in group K, and in no patient in group R, respectively. The number of patients needed to be treated (NNT) to prevent pain in one who would have had pain was 1.49, 1.75, and 1.15 in group L, group K, and group R, respectively. Lidocaine (40 mg), ketamine (0.5 mg/kg), or remifentanil (1 µg/kg) decreased the withdrawal response significantly and remifentanil (1 µg/kg) was the most effective in the prevention of withdrawal response among the drugs (P < 0.00833) (Table 2).
There were no significant differences in mean blood pressure and heart rate before injection of pretreatment drugs among the groups (Figs. 1 and 2). However, there were significant decreases in group R compared to control and other groups after injection of pretreatment drugs (Figs. 1 and 2). After intubation, mean blood pressure was increased in group N, group L, and group K compared to control (Fig. 1). However, in group R, mean blood pressure was significantly lower compared to other groups (P < 0.05) (Fig. 1). Heart rate increased significantly compared to control in all groups but, it was significantly lower in group R compared to other groups (P < 0.05) (Fig. 2).
No erythema, venous sequels, or adverse event were observed in any patient.
In the current study, we compared the preventive effect of lidocaine, ketamine, and rocuronium on withdrawal response of rocuronium injection. We showed that the 3 drugs decreased the withdrawal response caused by rocuronium injection. However, remifentanil was the most effective drug in prevention of withdrawal response among the drugs.
Pain during intravenous injection of rocuronium and distressing side effect are very common [10,11]. The pain is sometimes severe such as burning sensation [6,10,11], and causes withdrawal movement of the arm which can create secondary injury or pulmonary aspiration due to gastric regurgitation [12]. However, the mechanisms of injection pain of rocuronium are not clear.
Lidocaine is a common used amide local anesthetic agent which has short duration of action. Previous studies have reported that lidocaine is effective in reducing the pain on injection of rocuronium because of its local analgesic effect [6,11]. Cheong and Wong [11] reported that only 7% of patients had complained of pain after rocuronium injection when treated with lidocaine 30 mg before administration of rocuronium. Ahmad et al. [6] reported that pretreatment with lidocaine 40 mg reduced the incidence of withdrawal reaction to 30%. In our study, the incidence of withdrawal response was reduced to 20% after pretreatment with lidocaine 40 mg intravenously. It seems that the preventive effect of lidocaine against injection pain is dependent on the timing between the administration of lidocaine and rocuronium. According to the previous reports, peripheral analgesic effect of lidocaine is rapid and disappears quickly, not lasting beyond 2 minutes [6,11]. The time of administration of rocuronium in this study was 60 seconds after intravenous injection of lidocaine, which was earlier than the study of Ahmad et al. (more than 120 seconds) [6] and later than the Cheong and Wong's study (10 seconds).
Ketamine is a phencyclidine derivative hypnotic agent with strong analgesic properties [7,13]. Ketamine activates N-methyl-D aspartate receptors not only in the vascular endothelium but also in the central nervous system [13]. It may also increase the pain threshold in the central nervous system. Previous reports showed that ketamine administration before rocuronium injection reduced injection pain of rocuronium effectively [7,8,14]. The incidence of withdrawal response after rocuronium administration was 27% when ketamine 0.2 mg/kg has pretreated [14]. In another case, it was reported that rocuronium injection pain occurred in 40% of patients even if ketamine 0.5 mg/kg was used as pretreatment [7]. In our study, pretreatment of ketamine 0.5 mg/kg showed that the incidence of withdrawal response was 30%, comparable to lidocaine. However, severe withdrawal response with generalized movement occurred more frequently in the ketamine group (30%) than the lidocaine group (17%). Thus, lidocaine may be superior to ketamine in preventing rocuronium injection pain. In addition, it is well known that ketamine produces sympathetic stimulation or psychomimetic emergence reactions. However, we did not observe significant increase in blood pressure or heart rate compared to control, and psychomimetic reactions in our patients. We think that this was due to the low dose of ketamine (0.5 mg/kg) [15].
Remifentanil is an opioid agent with analgesic effect. It is very suitable for pretreatment during injection of rocuronium because it has very rapid onset time and rapid clearance [16]. In general, opioid decreases pain through both central and peripheral opioid receptors [16]. However, remifentanil acts mainly on the central opioid receptors for reducing pain during injection of rocuronium. When the venous occlusion technique with a tourniquet on the forearm was used for the remifentanil pretreatment, 9.1% adult patients and 60% pediatric patients showed pain responses [17,18]. Rocuronium showed significant prevention (0% of incidence) of withdrawal response or injection pain of rocuronium when administered intravenously [1], which was in agreement with our results. The incidence of withdrawal response was also 0% in the remifentanil group in our study. Although they have different time interval between remifentanil and rocuronium injection (90 vs. 60 seconds), it seems that 60 seconds may be enough to reach the central effect of remifentanil to prevent rocuronium injection pain in adults. Its peak effect after IV administration, occurs in 70 seconds [1].
Furthermore, remifentanil is frequently used for blunting hemodynamic changes during endotracheal intubation [19,20]. In this study, mean blood pressure and heart rate were significantly lower in the group which had remifentanil 1 µg/kg compared to other groups. The preventive effect of remifentanil on hemodynamic changes during endotracheal intubation is dose dependent. Optimal effect-site concentration of remifentanil for preventing development of hypertension during endotracheal intubation is 3.3 ng/ml [20]. However, calculated effect-site concentration of remifentanil in the current study was 2.21-2.29 ng/ml according to the Minto kinetic model when it was assumed that intubation was done about 2 minutes after remifentanil 1 µg/kg administration [21]. However, remifentanil which was used to reduce pain of rocuronium injection was also effective in blunting hemodynamic changes during endotracheal intubation in our study. The reasons of this difference are not clear, but the following conditions may have affected the results. Firstly, we used the bolus injection instead of target-controlled infusion since we focused on the pain of the rocuronium injection and accordingly modulated the administration method to be equivalent with other drugs. Secondly, time interval between remifentanil injection and endotracheal intubation was shorter in our study than previous study (about 120 vs. 250 second) [20]. It is well known that lidocaine was also effective for blunting the hemodynamic response to endotracheal intubation. However, our study did not show the effectiveness of lidocaine similar to the report of Suzuki et al. [19]. Relative low dose than known effective dose (1.0 mg/kg vs. 1.5 mg/kg) and shorter time after lidocaine injection than recommended timing (2 vs. 3 minutes) could be the reasons why lidocaine was not effective in preventing hemodynamic changes after endotracheal intubation [19].
There are several limitations to the current study. Firstly, latent time of preventive effect after injection of drug may be different according to the drug. Lidocaine acts more strongly on peripheral receptors and the effects are rapid and transient [6,11], whereas, analgesic effect of ketamine or remifentanil works mainly on the central nervous system and lasts longer [13,16]. Thus, the time of drug effects could be different. However, we set the timing of rocuronium injection to 60 seconds after administration of preventive drugs. Secondly, analgesic effects of the 3 drugs used in this study were not equipotent. As mentioned earlier, there is no clear comparison of the analgesic potency of lidocaine, ketamine, and remifentanil during injection of rocuronium. This makes it difficult to set the appropriate dose of each drugs and may lead to discrepancy in the study result. However, this study focused on the comparison of drugs which are used frequently for prevention of rocuronium injection pain in the clinical setting. Thirdly, venous occlusion technique is also used frequently for lidocaine; however, we used intravenous injection only. According to meta-analysis, pretreatment with lidocaine is effective whether venous occlusion is used or not [4]. Furthermore, pretreatment of remifentanil with venous occlusion is not effective as injection only [4]. The aim of this study was to determine the most effective pretreatment drug for rocuronium injection pain in the same condition, thus, we selected intravenous administration only. Finally, individual variations could have affected the withdrawal responses. Those responses following injection of drugs that causes pain can be different according to clinical factors such as gender, age, and cannulation site [22]. Moreover, while the cephalic vein was selected in the study, various anatomical variations exist in individuals [23].
In conclusion, we found that remifentanil (1 µg/kg intravenously) was the most effective drug in the prevention of the withdrawal response on rocuronium injection among the 3 drugs (lidocaine, ketamine, and remifentanil). Moreover, remifentanil reduced the hemodynamic changes after endotracheal intubation, effectively.
Acknowledgments
The present study was supported by grants from the Clinical Medicine Research Institute at Chosun University Hospital, 2012.
References
1. Kim JH, Kim JH, Han SH, Hwang JW, Oh AY. Alfentanil is comparable to remifentanil in preventing withdrawal movement following rocuronium injection. J Clin Anesth. 2009; 21:9–12. PMID: 19232934.

2. Lockey D, Coleman P. Pain during injection of rocuronium bromide. Anaesthesia. 1995; 50:474. PMID: 7793569.

3. Mencke T, Beerhalter U, Fuchs-Buder T. Spontaneous movements, local reactions and pain on injection of rocuronium. A comparison between female and male patients. Acta Anaesthesiol Scand. 2001; 45:1002–1005. PMID: 11576052.
4. Kwak HJ, Kim JY, Kim YB, Min SK, Moon BK, Kim JY. Pharmacological prevention of rocuronium-induced injection pain or withdrawal movements: a meta-analysis. J Anesth. 2013; 27:742–749. PMID: 23519582.
5. Zhang Y, Xiang Y, Liu J. Prevention of pain on injection of rocuronium: a comparison of lidocaine with different doses of parecoxib. J Clin Anesth. 2012; 24:456–459. PMID: 22762978.

6. Ahmad N, Choy CY, Aris EA, Balan S. Preventing the withdrawal response associated with rocuronium injection: a comparison of fentanyl with lidocaine. Anesth Analg. 2005; 100:987–990. PMID: 15781511.

7. Choi JH, Hwang JH, Shin YS. Comparison of the quantitative effect of ketamine on the vascular pain associated with Intravenous rocuronium administration. Korean J Anesthesiol. 2005; 49:30–34.

8. Chang HW, Kim SR, Lee YK. The effect of ketamine for pain on rocuronium injection pain. Korean J Anesthesiol. 2005; 48:479–482.

9. Kim JY, Kim JY, Kim YB, Kwak HJ. Pretreatment with remifentanil to prevent withdrawal after rocuronium in children. Br J Anaesth. 2007; 98:120–123. PMID: 17065169.

10. Moorthy SS, Dierdorf SF. Pain on injection of rocuronium bromide. Anesth Analg. 1995; 80:1067. PMID: 7726421.

11. Cheong KF, Wong WH. Pain on injection of rocuronium: influence of two doses of lidocaine pretreatment. Br J Anaesth. 2000; 84:106–107. PMID: 10740559.

12. Lui JT, Huang SJ, Yang CY, Hsu JC, Lui PW. Rocuronium-induced generalized spontaneous movements cause pulmonary aspiration. Chang Gung Med J. 2002; 25:617–620. PMID: 12479624.
13. Kohrs R, Durieux ME. Ketamine: teaching an old drug new tricks. Anesth Analg. 1998; 87:1186–1193. PMID: 9806706.
14. Liou JT, Hsu JC, Liu FC, Ching-Wah Sum D, Lui PW. Pretreatment with small-dose ketamine reduces withdrawal movements associated with injection of rocuronium in pediatric patients. Anesth Analg. 2003; 97:1294–1297. PMID: 14570640.

15. Hwang I, Noh JI, Kim SI, Kim MG, Park SY, Kim SH, et al. Prevention of pain with the injection of microemulsion propofol: a comparison of a combination of lidocaine and ketamine with lidocaine or ketamine alone. Korean J Anesthesiol. 2010; 59:233–237. PMID: 21057611.

16. Glass PS, Gan TJ, Howell S. A review of the pharmacokinetics and pharmacodynamics of remifentanil. Anesth Analg. 1999; 89(4 Suppl):S7–S14. PMID: 10511072.

17. Kwak HJ, Kim YB, Kim EJ, Kim JY. Prevention of rocuronium-induced withdrawal movement in children: a comparison of remifentanil with lidocaine. Korean J Anesthesiol. 2008; 54:437–440.

18. Ertugrul F. A comparison of the efficacies of different pre-treatment drugs in resolving the injection pain of rocuronium. J Int Med Res. 2006; 34:665–670. PMID: 17294999.

19. Suzuki T, Aono M, Fukano N, Kobayashi M, Saeki S, Ogawa S. Effectiveness of the timing principle with high-dose rocuronium during rapid sequence induction with lidocaine, remifentanil and propofol. J Anesth. 2010; 24:177–181. PMID: 20186439.

20. Kim KO, Chung S, Chang EJ, Lee Y. Optimal effect-site concentration of remifentanil for preventing development of hypertension during tracheal intubation with inhaled desflurane induction. Korean J Anesthesiol. 2011; 60:8–11. PMID: 21359074.

21. Minto CF, Schnider TW, Egan TD, Youngs E, Lemmens HJ, Gambus PL, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology. 1997; 86:10–23. PMID: 9009935.
22. Kang HJ, Kwon MY, Choi BM, Koo MS, Jang YJ, Lee MA. Clinical factors affecting the pain on injection of propofol. Korean J Anesthesiol. 2010; 58:239–243. PMID: 20498771.

23. Shima H, Ohno K, Michi K, Egawa K, Takiguchi R. An anatomical study on the forearm vascular system. J Craniomaxillofac Surg. 1996; 24:293–299. PMID: 8938512.

Fig. 1
Sequential changes of mean blood pressure before and after intravenous injection of normal saline, lidocaine, ketamine, and remifentanil and after endotracheal intubation. There was no significant difference in mean blood pressure before injection of pretreatment drugs (control) among the groups. After injection of pretreatment drugs, mean blood pressure was significantly decreased in group R compared to control and other groups. After intubation, it increased in group N, group L, and group K compared to control. Mean blood pressure of group R after endotracheal intubation was significantly lower than other groups (P < 0.05). Group N: normal saline, Groups L: lidocaine 40 mg, Group K: ketamine 0.5 mg/kg, Group R: remifentanil 1 µg/kg. *P < 0.05 compared with control. †P < 0.05 compared with group N. ‡P < 0.05 compared with group L. §P < 0.05 compared with group K.
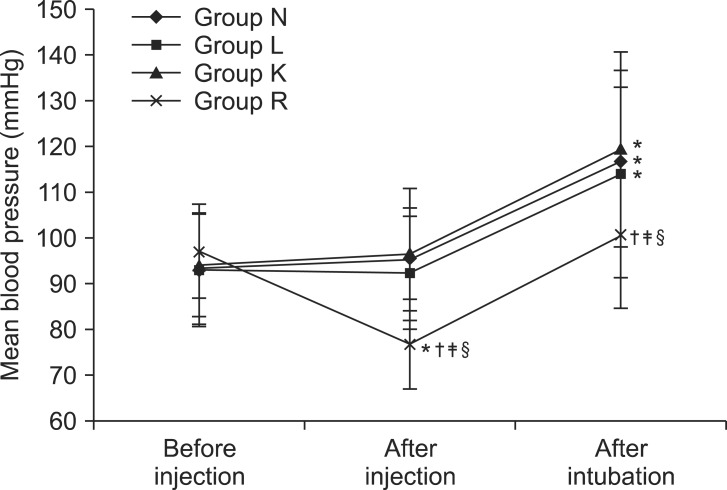
Fig. 2
Sequential changes of heart rate before and after intravenous injection of normal saline, lidocaine, ketamine, and remifentanil and after endotracheal intubation. There was no significant difference in heart rate before injection of pretreatment drugs (control) among the groups. After injection of pretreatment drugs, heart rate was significantly decreased in group R compared to control and other groups. After intubation, heart rate was increased compared to control in all groups, but it was significantly lower in group R than other groups (P < 0.05). Group N: normal saline, Groups L: lidocaine 40 mg, Group K: ketamine 0.5 mg/kg, Group R: remifentanil 1 µg/kg. *P < 0.05 compared with control. †P < 0.05 compared with group N. ‡P < 0.05 compared with group L. §P < 0.05 compared with group K.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download