Abstract
Natural orifice transluminal endoscopic surgery (NOTES) is an evolving field of minimally invasive surgery. NOTES reaches the target organ by inserting the endoscope through a natural orifice (e.g. mouth, anus, urethra, vagina) and offers advantages of less postoperative pain and lower complication rate. Since its first description in 2004, NOTES has progressed from use on animal models to humans. We experienced anesthetic care of two patients who underwent transoral NOTES under general anesthesia.
Natural orifice transluminal endoscopic surgery (NOTES) is a new minimally invasive surgery performed using flexible endoscopes without cutaneous skin incision. In NOTES, endoscopes are introduced through natural openings, including the mouth, anus, urethra, and vagina. Access to the thoracic and abdominal cavities is then gained through incisions in internal organs such as the esophagus, stomach, vagina, bladder, and colon [1,2]. Many potential benefits have been suggested for NOTES, including early recovery time, decreased wound infection, less postoperative pain, and improved cosmesis [1,3]. In addition, NOTES has been assessed as potentially useful for morbidly obese patients or patients at high risk for postoperative complications [4]. Since its first description in 2004, NOTES has progressed from use on animal models to humans, and anesthesiologists must appropriately manage patients undergoing NOTES. However, few studies have described anesthetic management during NOTES. Herein, we report the anesthetic management of 2 patients who underwent NOTES.
A 77-year-old man (height, 168 cm; weight, 70 kg) presented at our hospital with black tarry stool. An esophagogastroduodenoscopy was performed and a gastric intestinal stromal tumor 4 cm in size was detected. Thereafter, endoscopic full-thickness gastric resection (EFTGR) was planned. EFTGR can be regarded as a hybrid form of NOTES or as an intermediate form step since a full-thickness incision in the gastric wall is made endoscopically and closure is achieved laparoscopically. We planned the surgery in such a way that endoscopic resection of the tumor would be performed by an endoscopic operator experienced in internal medicine and the laparoscopic dissection and closure of the stomach would be performed by a general surgeon.
The patient had a history of diabetes mellitus and hypertension, and he been taking medicines for these disorders. His preoperative routine laboratory values were within the normal range and a preoperative electrocardiogram (ECG) showed sinus bradycardia of 58 beats/min. The patient was premedicated with 1 mg of butorphanol and 0.2 mg of glycopyrrolate intramuscularly before surgery. His vital signs were stable upon arrival at the operating room and were monitored thereafter using ECG (lead II), pulse oximetry, end-tidal carbon dioxide concentration (ETCO2), and noninvasive blood pressure (BP) determination Because the endoscopes were placed in his mouth, the patient's temperature was measured using a skin temperature probe.
Anesthesia was induced using 120 mg of propofol, 50 mg of rocuronium, and 100 µg of fentanyl and nasotracheal intubation was performed using a nasal RAETM tracheal tube with a 7.5 mm inner diameter (ID), because nasotracheal intubation is convenient for endoscopic procedures. General anesthesia was maintained using O2 at 2 L/min, N2O at 2 L/min, and 1.5-2.5 vol% of sevoflurane, and the concentration of sevoflurane was controlled using the bispectral index. Mechanical ventilation with a tidal volume of 600 ml and a respiratory rate of 10 breaths/min was maintained. After induction, the peak inspiratory pressure (PIP) and ETCO2 were 16-17 cmH2O and 35-37 mmHg, respectively.
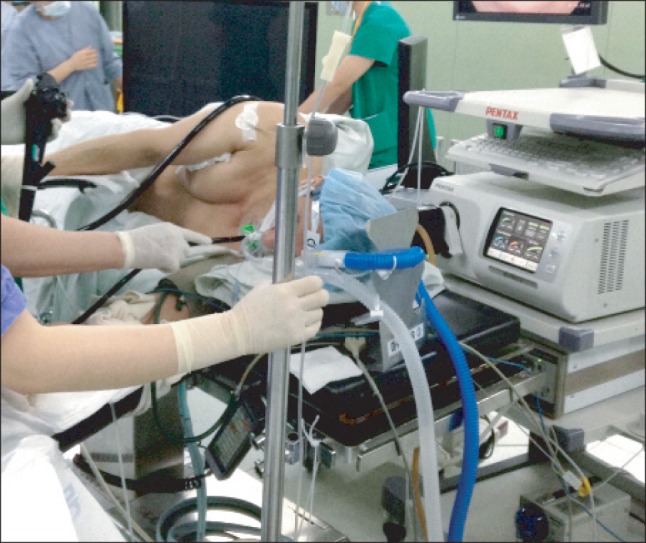
The patient was placed in the supine position while the laparoscopic operator remained on the right side of the patient to insert the port and perform the stomach dissection. A pneumoperitoneum was created using carbon dioxide (CO2) gas at a pressure of 14 mmHg throughout the surgery. After CO2 injection, the ETCO2 increased up to 40 mmHg, and hence, the respiratory rate was controlled; however, no change was made to the tidal volume as the PIP was maintained at 23-25 mmHg. After laparoscopic dissection, the endoscopic operator moved into position near the patient's head to perform an endoscopic full-thickness resection of the tumor with sufficient surgical margins (Fig. 1). During endoscopic resection, visibility was ensured through air insufflations, and the PIP pressure was approximately 5-7 mmHg lower than that measured during the laparoscopic procedure using CO2. After confirming no active bleeding, the endoscope was removed, and the laparoscopic operator performed closure of the stomach and sutured the skin wound.
During the entire procedure, hemodynamic stability was maintained and ETCO2 was maintained at 32-37 mmHg. The time required for the laparoscopy was 70 min and that for the endoscopy was 60 min; the anesthesia time was 160 min. Upon completion of the surgery, the patient was transferred to the general ward. No specific complications were observed during the postoperative period, and the patient was discharged on postoperative day 4.
A 50-year-old man (height, 167 cm; weight, 65 kg) was diagnosed with esophageal achalasia due to swallowing difficulty for several years. He was scheduled for peroral endoscopic myotomy (POEM), which is a technique that was developed in the context of transesophageal NOTES as an endoscopic alternative to laparoscopic esophageal myotomy. The patient had no relevant medical history, and preoperative examination did not reveal any specific conditions. He was premedicated using 1 mg of butorphanol and 0.2 mg of glycopyrrolate intramuscularly before surgery.
In the operating room, routine monitoring was conducted using ECG (lead II), pulse oximetry, ETCO2 measurements and noninvasive BP monitoring. The patient's vital signs were as follows: BP, 110/69 mmHg; heart rate (HR), 65 beats/min; and peripheral oxygen saturation (SpO2), 100%. General anesthesia was induced using 120 mg of propofol, 50 mg of rocuronium, and 100 µg of fentanyl, and nasotracheal intubation was performed using a nasal RAETM tracheal tube with a 7.5 mm ID. For the same reason as in case 1, tracheal intubation was performed through the nose. Anesthesia was maintained using O2 at 2 L/min, N2O at 2 L/min, and 1.5-2.5 vol% of sevoflurane. Volume controlled ventilation was performed using a tidal volume of 600 ml and at a rate of 10 breaths/min.
The patient was placed in the left lateral decubitus position, and the endoscopic operator stood on the left side of the patient. CO2 gas was provided for insufflation during the procedure, using a CO2 insufflator and a standard insufflating tube. Endoscopic CO2 insufflation was controlled with a gas feed of 1.2 L/min. The operation comprised the following steps: (1) creation of the mucosal entry and submucosal tunnel, (2) endoscopic myotomy, and (3) closure of the mucosal entry. First, the endoscopic operator administrated a submucosal injection (0.9% normal saline with indigo carmine dye) at the level of the midesophagus in order to ensure a safe mucosal incision. The mucosal incision was then made on the mucosal surface using an electric knife, and the endoscope was inserted into the submucosal space. The submucosal tunnel was then extended 2 cm below the gastroesophageal junction via the endoscopic submucosal dissection technique. Next, the endoscope was withdrawn to the mucosal incision and a circular muscle myotomy was performed. After completion of the myotomy, the mucosal entry site was closed using several hemostatic clips.
For this patient in particular, the surgical duration was relatively long as the achalasia lesion was large.
During surgery, ETCO2 was maintained at 30-34 mmHg and PIP at 13-15 mmHg. The patient's abdomen was not covered using surgical drapes to ensure visibility so that severe pneumoperitoneum could be recognized immediately (Fig. 2). The patient was hemodynamically stable throughout the entire surgery. The time required for the operation and anesthesia were 120 min and 160 min, respectively. The patient was transferred to the general ward after surgery, and a postoperative chest radiograph showed no pneumomediastinum.
NOTES refers to a surgical procedure in which an internal incision is made using endoscopes inserted through natural orifices (the mouth, anus, vagina, and urethra), instead of through an external incision [1]. Since its first description in 2004, NOTES has progressed from use in animal models to humans, and many studies have shown its use worldwide. Many procedures have been performed using NOTES, some frequently, including cholecystectomy, appendectomy, peritoneoscopy, gastrectomy, colectomy, esophageal myotomy, and nephrectomy. On reviewing articles published so far, the most common procedure involving access via an orifice is the cholecystectomy, and the most common approach is transvaginal [1,5].
NOTES has been recognized as a new revolution in the field of minimally invasive surgery as it has many advantages. The most obvious difference between traditional surgery and NOTES is that no skin incision is performed in the latter, and postoperative pain is therefore reduced. Furthermore, the reduction in pain results in a decrease in the use of postoperative narcotics, which helps avoid related side effects such as postoperative ileus, altered psychological status, and nausea/vomiting. In addition, it reduces wound infection and improves cosmesis [3,6].
Compared to laparoscopic surgery, NOTES enables the effective removal of intraluminal tumors, which are difficult to identify by the laparoscopic approach, and it is also useful in the cases of morbidly obese patients [4]. Some experimental studies in pigs showed no difference between NOTES and laparoscopic surgery with respect to cardiopulmonary parameters and inflammatory mediators [7,8]. However, other studies have shown better pulmonary gas exchange and a reduced perioperative inflammatory response with NOTES [9,10]. These studies, however, do have the limitations of being designed for healthy animals and performed in small samples. Therefore, further studies of NOTES in humans are needed to clarify the cardiovascular and respiratory effects in comparison with laparoscopic surgery.
In anesthetic management, many difficulties are encountered via the airway approach. In our patients, nasotracheal intubation was performed through the nose since the endoscopes were introduced through the mouth. In addition, the endoscopic operator performed the surgery while standing near the head of the patient, which makes use of the airway approach somewhat difficult. Therefore, the correct depth and fixation of the nasotracheal tube during intubation is necessary, and caution should be exercised to maintain adequate eye protection.
Similar to laparoscopic surgery, NOTES requires gas insufflation of the abdominal and thoracic cavity, which aids adequate visualization of the abdominal and intrathoracic organs. In POEM, gas insufflation is necessary for submucosal tunnel formation and to ensure appropriate visualization. The most commonly used gas is CO2, since it is inexpensive, noncombustible, and colorless [7]. Moreover, it is quickly absorbed and excreted by the lungs and is highly soluble in water, which reduces the risk of embolism and is considered safer than air [7,9]. However, CO2 insufflation is associated with respiratory and hemodynamic changes. The degree of detrimental effects is related to the duration of exposure and intra-abdominal pressure. The potentially detrimental effects include decreased pulmonary compliance and renal perfusion, myocardial depression, increased release of catecholamines due to increased intra-abdominal pressure and increased intracranial pressure [7,8]. Therefore, pressure-regulated insufflators should be used to control the pressure during such operations. However, the laparoscopic insufflation devices that are currently used are not suitable for NOTES and no analog devices have developed thus far. Therefore, in patients undergoing NOTES with CO2, the gas feed for insufflation should be consistently controlled and monitored, and an open view of the patient's abdomen should be maintained to ensure that severe pneumoperitoneum can be quickly diagnosed [8,11].
In case 1, laparoscopic closure was performed under CO2 insufflation after endoscopic resection under air insufflation. In case 2, which involved POEM, CO2 insufflation was essential to ensure safe creation of the submucosal tunnel and endoscopic myotomy. Because CO2 gas was used in both cases, indirect monitoring of CO2 retention through ETCO2 monitoring was implemented to reduce related complications. In POEM, the airway pressure in positive pressure ventilation is maintained at a higher pressure than that for endoscopic CO2 insufflation to reduce the risk of mediastinal emphysema and pneumomediastinum [12].
In conclusion, NOTES is a relatively new field of endoscopic surgery and has many advantages over the existing laparoscopic surgery. However, several problems have been identified, including issues with access to the peritoneal cavity, gastric closure, development of new devices, and management of intraperitoneal complications. Furthermore, there are insufficient data on anesthetic management in relation to the technique, and further research is necessary in the future. The present study described anesthetic management in 2 patients, without any particular complications, who underwent NOTES. When administering anesthetic care to a patient undergoing NOTES, anesthesiologists should closely monitor the patient's position as well as ETCO2 to minimize the incidence of mediastinal emphysema and pneumomediastinum and to ensure early detection of pneumoperitoneum-related respiratory and hemodynamic changes.
References
1. Clark MP, Qayed ES, Kooby DA, Maithel SK, Willingham FF. Natural orifice translumenal endoscopic surgery in humans: a review. Minim Invasive Surg. 2012; 2012:189296. PMID: 22720153.

2. ASGE. SAGES. ASGE/SAGES Working Group on Natural Orifice Translumenal Endoscopic Surgery White Paper October 2005. Gastrointest Endosc. 2006; 63:199–203. PMID: 16427920.
3. Granberg CF, Gettman MT. Rationale for natural orifice transluminal endoscopic surgery and current limitations. BJU Int. 2010; 106:908–912. PMID: 20883243.

4. Panait L, Wood SG, Bell RL, Duffy AJ, Roberts KE. Transvaginal natural orifice transluminal endoscopic surgery in the morbidly obese. Surg Endosc. 2013; 27:2625–2629. PMID: 23355168.

5. Auyang ED, Santos BF, Enter DH, Hungness ES, Soper NJ. Natural orifice translumenal endoscopic surgery (NOTES®): a technical review. Surg Endosc. 2011; 25:3135–3148. PMID: 21553172.

6. Schaefer M. Natural orifice transluminal endoscopic surgery (NOTES): implications for anesthesia. F1000 Med Rep. 2009; 1:80. PMID: 20948698.

7. Grabowski JE, Talamini MA. Physiological effects of pneumoperitoneum. J Gastrointest Surg. 2009; 13:1009–1016. PMID: 18766415.

8. Navarro-Ripoll R, Martinez-Palli G, Guarner-Argente C, Cordova H, Martinez-Zamora MA, Comas J, et al. On-demand endoscopic CO2 insufflation with feedback pressure regulation during natural orifice transluminal endoscopic surgery (NOTES) peritoneoscopy induces minimal hemodynamic and respiratory changes. Gastrointest Endosc. 2012; 76:388–395. PMID: 22817790.

9. von Delius S, Sager J, Feussner H, Wilhelm D, Thies P, Huber W, et al. Carbon dioxide versus room air for natural orifice transluminal endoscopic surgery (NOTES) and comparison with standard laparoscopic pneumoperitoneum. Gastrointest Endosc. 2010; 72:161–169. PMID: 20381043.

10. Georgescu I, Saftoiu A, Patrascu S, Silosi I, Georgescu E, Surlin V. Perioperative inflammatory response in natural orifice translumenal endoscopic surgery. Surg Endosc. 2013; 27:2551–2556. PMID: 23389067.

11. Pucher P, Sodergren MH, Alkhusheh M, Clark J, Jethwa P, Teare J, et al. The effects of natural orifice translumenal endoscopic surgery (NOTES) on cardiorespiratory physiology: a systematic review. Surg Innov. 2013; 20:183–189. PMID: 22991384.
12. Eleftheriadis N, Inoue H, Ikeda H, Onimaru M, Yoshida A, Hosoya T, et al. Training in peroral endoscopic myotomy (POEM) for esophageal achalasia. Ther Clin Risk Manag. 2012; 8:329–342. PMID: 22888256.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download