Introduction
Succinylcholine has been still used in anesthesia to produce profound neuromuscular blockade of rapid onset and short duration [
1]. Succinylcholine commonly produces frequent adverse effects, including muscle fasciculation and myalgia. Although these effects are minor, myalgia, which can be accompanied by muscle stiffness, can induce significant discomfort in some patients [
2]. Pretreatment with
d-tubocurarine, vecuronium, rocuronium, mivacurium, gallamine, magnesium and atracurium has been considered to prevent muscle fasciculation and myalgia induced by succinylcholine [
3]. Pretreatment with small doses (10% of the 95% reduction in twitch tension [ED
95]) of rocuronium before succinylcholine administration would rarely produce a measurable neuromuscular effect, and therefore would be recommended as an appropriate precurarizing dose in the computer simulation [
4]. However, 0.06-0.1 mg/kg of rocuronium (20-30% of the ED
95 ) has been recommended as a precurarizing dose of succinylcholine 1.5 mg/kg clinically [
5,
6]. Although a larger dose of rocuronium (20% of the ED
95) can greatly suppress succinylcholine-induced fasciculation, the risk of a significant neuromuscular block in three minutes following the precurarization may be increased [
7]. Fukano et al. [
8] reported that 0.03 mg/kg rocuronium was recommended for safe and effective precurarizing dose in 3 min before succinylcholine. However, the effect of this dose to prevent fasciculations and postoperative myalgia from succinylcholine was not evaluated.
The aim of the present study was to identify the optimal dose of rocuronium to prevent succinylcholine-induced fasciculation and myalgia and to evaluate the influence of rocuronium on the speed of onset produced by succinylcholine.
Materials and Methods
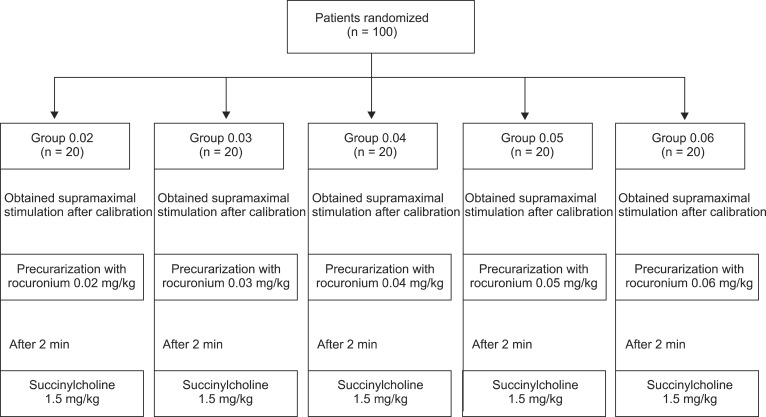
The Hospital Ethics Committee approved this study protocol and written informed consent was obtained from all patients after the aim and potential risks of the study were fully explained to each. One hundred patients, aged 20 to 58 years, with an American Society of Anesthesiologists physical status of I or II undergoing elective surgery with a general anesthesia in the supine position were studied in a double blind randomized study. Patients were excluded for the following reasons: neuromuscular, cardiovascular, hepatic, or renal diseases, an age < 18 or > 65 years, those with body weight 20% greater than ideal body weight, with a history of drug abuse, and with an anticipated difficult intubation. Patients were divided into five groups. Twenty patients were allocated randomly to each pretreatment group: 0.02 mg/kg rocuronium (Group 0.02), 0.03 mg/kg rocuronium (Group 0.03), 0.04 mg/kg rocuronium (Group 0.04), 0.05 mg/kg rocuronium (Group 0.05) and 0.06 mg/kg rocuronium (Group 0.06) (
Fig. 1).
No premedication was given. Monitoring, established on arrival in the operating room, included electrocardiography, noninvasive arterial pressure, oxygen saturation, capnography and a bispectral index (BIS) monitor (Model A 2000, Aspect Medical Systems, Natick, MA, USA). Neuromuscular function was assessed using acceleromyography of the adductor pollicis muscle (TOF-Watch SX®, Organon Ltd., Dublin, Ireland). Before placing the surface electrodes, the skin overlying the ulnar nerve was cleansed with isopropyl alcohol. Two electrodes (Cleartrode™, Ref 1720-003, ConMed®, Utica, NY, USA) were placed over the prepared skin. A force transducer was fixed to the thumb.
General anesthesia was induced with remifentanil 0.5 µg/kg/min injected intravenous over 2 minutes (min) followed by propofol 2-2.5 mg/kg injected intravenous over 30 seconds (s). As soon as a patient lost consciousness, ventilation via facemask with a fresh gas flow at 4 L/min (50% air in oxygen) controlled manually to maintain the end-tidal CO
2 at 30 to 35 mmHg and neuromuscular monitoring began immediately. The fingers were tightly fixed to the armboard after a 5-s 50-Hz tetanic stimulus over ulnar nerve. The calibration and supramaximal stimulation were achieved by the built-in calibration function (CAL 2) of the acceleromyography. Train-of-four (TOF) stimulation (0.2 ms duration at 2 Hz with supramaximal current) was repeated every 15 s. After stabilization of control responses (< 5% variation in the first twitch and TOF), each precurarizing dose of rocuronium was administered via computer-generated randomization. The time course of the TOF ratios was collected on a computer and monitored throughout the endotracheal intubation. At 2 min after the pretreatment of rocuronium, all patients received succinylcholine 1.5 mg/kg. Fasciculations were evaluated by an investigator blinded to the patient's group assignment and were graded according to a four-point rating scale: 0 = no fasciculation, 1 = mild, fine fasciculation of the eyes, neck, face or fingers without limb movement, 2 = moderate fasciculation involving limbs and/or trunk, 3 = severe fasciculation with movement of one or more limbs and/or movements requiring forceful retention [
9]. Onset from the time of administration of succinylcholine to maximum depression of first twitch of TOF stimulation was recorded. Tracheal intubation was performed at the maximum depression of first twitch. Anesthesia was maintained with 1-1.5 minimum alveolar concentration of sevoflurane in order to hold the BIS lower than 50 after endotracheal intubation. Analgesia was provided by 0.05-0.2 µg/kg/min remifentanil during the surgery. The incidence and severity of postoperative myalgia and the consumption of fentanyl in patient controlled analgesia (PCA) was assessed at 24 hours postoperatively by another investigator who was unaware of injection details, using a four-point rating scale and graded as 0 = no muscle pain, 1 = muscle stiffness limited to one area of the body, 2 = muscle pain or stiffness noticed spontaneously complained of by the patient that requires analgesics, 3 = incapacitating generalized, severe muscle stiffness or pain [
10].
Statistical analyses were performed using SPSS statistical software, version 17.0 (SPSS Inc, Chicago, IL, USA). In this study, the sample size calculation was taken from the previous results [
8]. On the basis of a relevant 20% change (SD 17% change) in the onset time (79.5 ± 12.3 s) of succinylcholine with pretreatment of rocuronium 0.03 mg/kg, we calculated that 17 patients in each 5 groups could test the null hypothesis at 0.05 significance with a power of 0.80. We enrolled 20 patients to account for a 10% drop out rate. Analysis of variance (ANOVA) was performed for continuous variables (i.e., age, weight, height, onset time, and fentanyl consumption) and multiple comparisons were made with the Bonferroni post hoc test when the results were significant. Repeated-measure ANOVA was used to compare the TOF ratios between 1 and 2 min after precurarizing dose. The Kruskal-Wallis ANOVA with Tukey test for post hoc analysis was used to determine the significance of differences with respect to incidence and severity of the fasciculation and myalgia. The data were expressed as the mean ± SD (number, %). Differences were considered statistically significant if P < 0.05.
Results
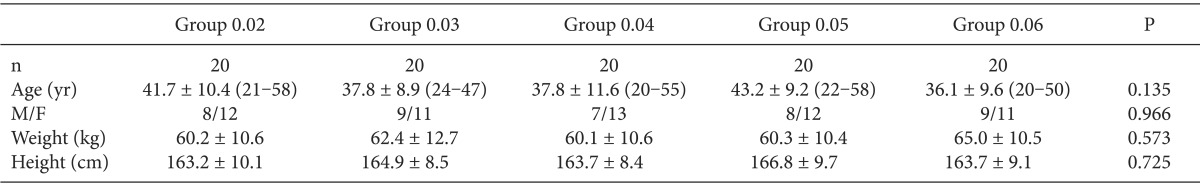
Among the 100 patients recruited in this study none was excluded. There were no differences in patient characteristics between groups (
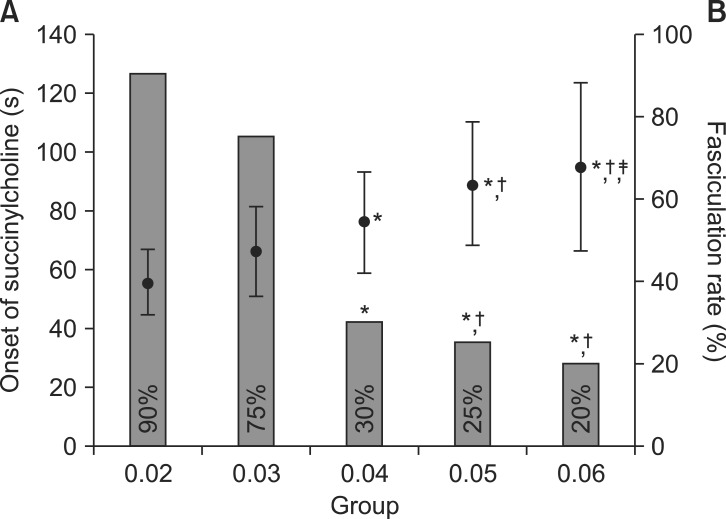
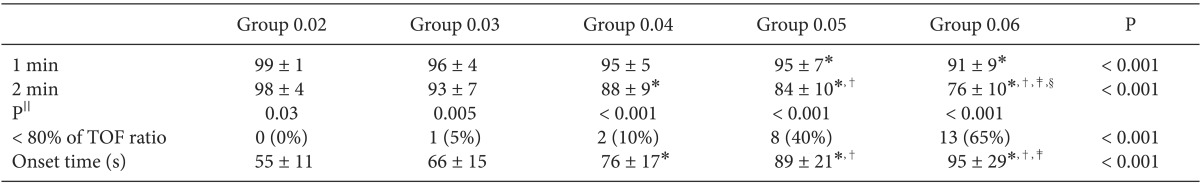
Table 1). An averaged TOF ratio at 2 min was significantly decreased from 98 ± 4% (Group 0.02) to 76 ± 10% (Group 0.06) with increasing the amount of precurarizing dose of rocuronium (P < 0.001) (
Table 2). Less than 80% of TOF ratio was occurred in more than 40% of subjects after precurarizing dose of more than 0.05 mg/kg rocuronium at 2 min (
Table 2). The onset time of succinylcholine was significantly longer from 55 ± 11 s (Group 0.02) to 95 ± 29 s (Group 0.06) with increasing the amount of precurarizing dose of rocuronium (P < 0.001) (
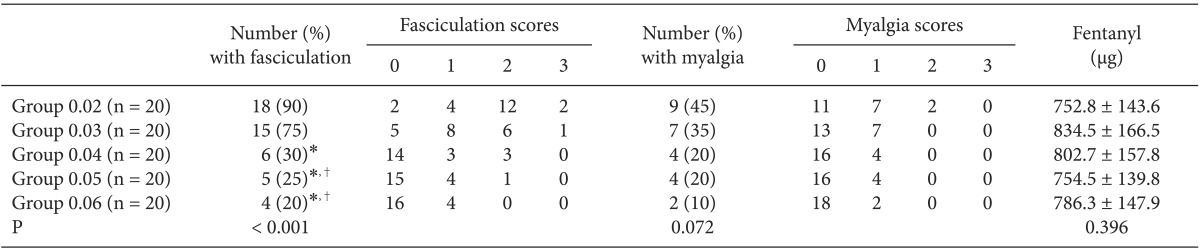
Table 2). The incidence and severity of visible muscle fasciculation was significantly less with increasing the amount of precurarizing dose of rocuronium (P < 0.001) (
Table 3). On postoperative day 1, the incidence and severity of myalgia tend to decrease according to increasing the amount of precurarizing dose of rocuronium, but there was no significance (P = 0.072) (
Table 3). The consumption of fentanyl in PCA within the first 24 hours after the operation was comparable among 5 groups (P = 0.396) (
Table 3).
Fig. 2 depicts the relationship between the onset time after administration of succinylcholine according to the precurarizing dose of rocuronium and fasciculation. The precurarizing dose of rocuronium 0.04 mg/kg showed lower incidence of fasciculation (30%) than Group 0.02 (90%) and Group 0.03 (75%), and maintaining the clinically acceptable onset time (76 ± 17 s) than Group 0.05 (89 ± 21 s) and Group 0.06 (95 ± 29 s).
Discussion
The principal findings of this study were the incidence and severity of visible muscle fasciculation was significantly less with increasing the amount of precurarizing dose of rocuronium (P < 0.001). Those of myalgia tend to decrease according to increasing the amount of precurarizing dose of rocuronium, but there was no significant (P = 0.072). The onset time of succinylcholine was significantly longer with increasing the amount of precurarizing dose of rocuronium (P < 0.001). The precurarizing dose of rocuronium 0.04 mg/kg showed lower incidence of fasciculation than Group 0.02 and Group 0.03, and maintaining the clinically acceptable onset time than Group 0.05 and Group 0.06 (
Fig. 2).
Succinylcholine-induced fasciculation and postoperative myalgia are a well-recognized side effect with the reported incidence of 95% and 50%, respectively [
3]. Myalgia after the use of succinylcholine is most frequent on the first postoperative day [
11]. Succinylcholine-induced fasciculation is widely believed to be the primary cause of myalgia [
12]. The pretreatment with small (nonparalytic) doses of nondepolarizing muscle relaxants best prevent fasciculation intensity and muscle pain after succinylcholine administration [
3]. However, the risk of potentially serious adverse events (blurred vision, diplopia, heavy eyelids, muscle weakness, difficulty in swallowing, and voice disorder) with muscle relaxants is not negligible [
5]. In the previous study, a pretreatment of 0.06 mg/kg rocuronium before succinylcholine injection occurred the depression of an averaged TOF ratio from 100 to 68% [
8]. In this study, we also found an averaged TOF ratio was depressed to 84 ± 10% and 76 ± 10% after rocuronium 0.05 mg/kg and 0.06 mg/kg at 2 min, respectively.
Awake patients in a TOF ratio below 90% observed at the adductor pollicis complained of the unpleasant experience of swallowing difficulty due to decrease the upper esophageal sphincter tone markedly [
13]. It seems possible that the risk of pulmonary aspiration of gastric contents may be increased in patients with a full stomach when the pretreatment of rocuronium is overdosed. When the TOF ratio was 80% in awake patients, forced expiratory vital capacity and forced inspiratory volume in 1 s decreased to 85% of baseline, indicating impaired respiratory muscle strength [
14]. In our study, less than 80% of TOF ratio was occurred in 40 and 65% of subjects after precurarizing dose of rocuronium 0.05 mg/kg and 0.06 mg/kg at 2 min, respectively. It seems very possible that awake patients suffered a respiratory difficulty and muscle weakness.
The precurarizing dose of nondepolarizing neuromuscular blockade reduced the neuromuscular blocking potency of succinylcholine and also delayed the onset of succinylcholine [
15]. In our study, the onset of succinylcholine was 89 ± 21 s and 95 ± 29 s after precurarizing dose of rocuronium 0.05 mg/kg and 0.06 mg/kg, respectively, which delay the timing of tracheal intubation (e.g. rapid sequence induction). It is therefore suggested, from our results, that rocuronium 0.05 mg/kg and 0.06 mg/kg are not the appropriate dose of rocuronium for the safe and effective precurarization.
A pretreatment with small dose (10% ED
95) of rocuronium was recommended for the precurarization in the computer simulation not in the clinical study [
4]. In the previous study [
8], 0.03 mg/kg rocuronium was recommended for safe and effective precurarizing dose in 3 min before succinylcholine. However, the effect of this dose to prevent fasciculations and postoperative myalgia from succinylcholine was not evaluated and the each subject was too small (n = 12). In our study, precurarization with rocuronium 0.02 mg/kg and 0.03 mg/kg obtained the faster onset of succinylcholine-induced neuromuscular block (55 ± 11 s and 66 ± 15 s), respectively, than other groups. However, this simultaneously maintained the succinylcholine-induced fasciculation (90 and 75%) and myalgia (45 and 35%), respectively (
Table 3). It is also suggested that rocuronium 0.02 mg/kg and 0.03 mg/kg are not the appropriate dose of rocuronium for the reduction of the intensity of the fasciculation and myalgia. In the present study, the precurarization with rocuronium 0.04 mg/kg was optimal dose considering with the reduction of the intensity of the fasciculation and the safe and effective precurarization, and maintaining in the clinically acceptable onset time (63 ± 21 s) [
16], although rocuronium 0.04 mg/kg has a disadvantage of increasing the onset time (76 s).
An optimal pretreatment interval of 3 min has been recommended for many commonly used agents such as atracurium and d-tubocurarine [
17]. However, such a lengthy interval is not only impractical with busy operating room lists but it also exposes the awake patient to the potentially unpleasant experiences of difficulty in swallowing, breathing and muscle weakness. To avoid these hazards, we chose 2 min of rapid precurarizing time that reduce the possibility to expose the patients to the side effects of the precurarization.
One limitation of this study is that postoperative myalgia was assessed only up to 24 hours. In the previous study, 92% of patients after surgery reported myalgia within 24 hours [
18]. Although the incidence of postoperative myalgia was not different between 24 hours and 48 hours [
19], it may be accurate to get the results of up to 48 hours.
In conclusion, precurarization with 0.04 mg/kg rocuronium was optimal dose considering that the reduction in the incidence and severity of fasciculation and myalgia with acceptable onset time, and the safe and effective precurarization.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download