1. Hunter JM. Rocuronium: the newest aminosteroid neuromuscular blocking drug. Br J Anaesth. 1996; 76:481–483. PMID:
8652315.

2. Ahmad N, Choy CY, Aris EA, Balan S. Preventing the withdrawal response associated with rocuronium injection: a comparison of fentanyl with lidocaine. Anesth Analg. 2005; 100:987–990. PMID:
15781511.

3. Steegers MA, Robertson EN. Pain on injection of rocuronium bromide. Anesth Analg. 1996; 83:203. PMID:
8659757.

4. Cheong KF, Wong WH. Pain on injection of rocuronium: influence of two doses of lidocaine pretreatment. Br J Anaesth. 2000; 84:106–107. PMID:
10740559.

5. Borgeat A, Kwiatkowski D. Spontaneous movements associated with rocuronium: is pain on injection the cause? Br J Anaesth. 1997; 79:382–383. PMID:
9389860.

6. Lui JT, Huang SJ, Yang CY, Hsu JC, Lui PW. Rocuronium-induced generalized spontaneous movements cause pulmonary aspiration. Chang Gung Med J. 2002; 25:617–620. PMID:
12479624.
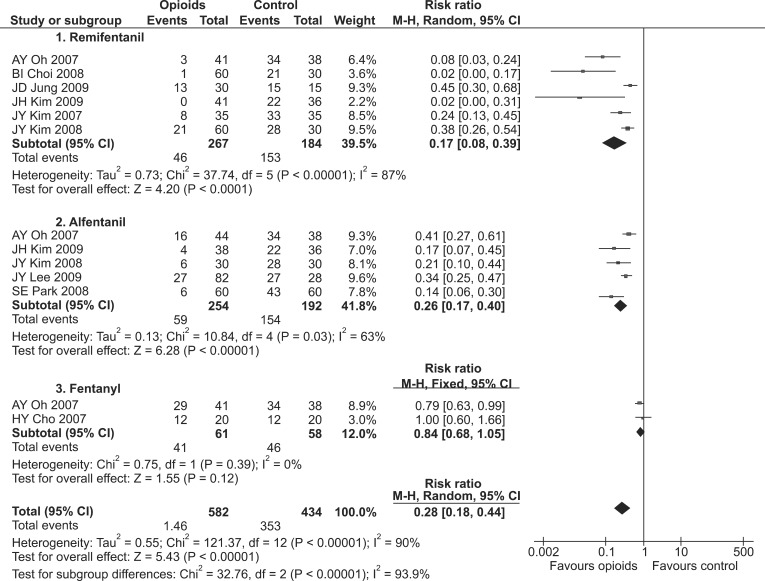
7. Kwak HJ, Kim JY, Kim YB, Min SK, Moon BK, Kim JY. Pharmacological prevention of rocuronium-induced injection pain or withdrawal movements: a meta-analysis. J Anesth. 2013; 27:742–749. PMID:
23519582.

8. Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration;2011. updated March 2011.
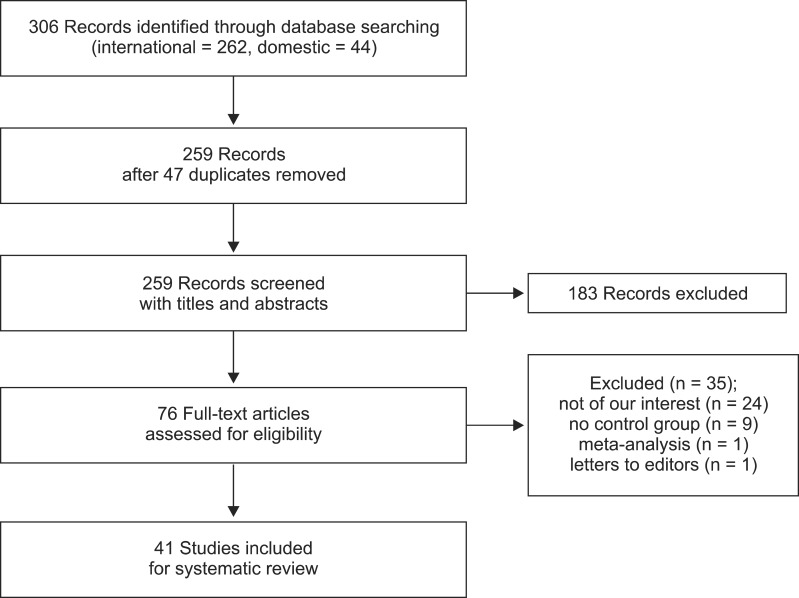
9. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009; 339:b2700. PMID:
19622552.

10. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560. PMID:
12958120.

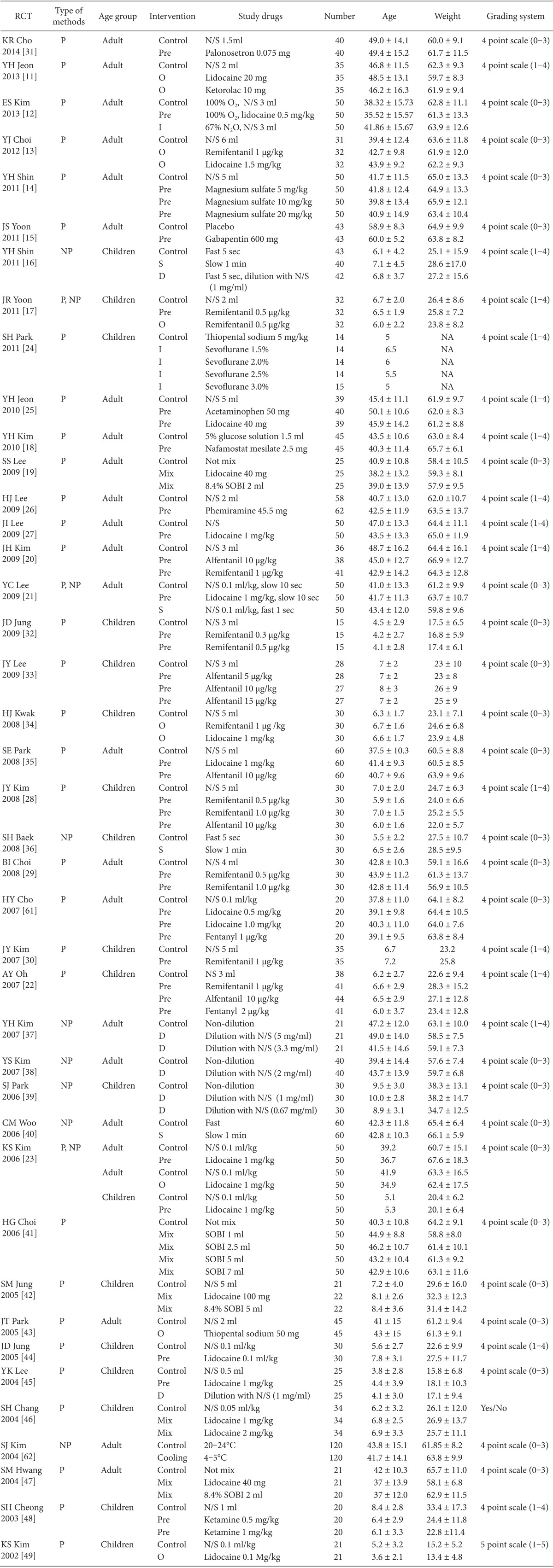
11. Jeon Y, Ha JH, Lee JE, Lee HC, Ryu T, Kwak KH. Rocuronium-induced withdrawal movement: influence of ketorolac or a combination of lidocaine and ketorolac pretreatment. Korean J Anesthesiol. 2013; 64:25–28. PMID:
23372882.

12. Kim E, Kim CH, Kim HK, Kwon JY, Lee do W, Kim HY. Effect of nitrous oxide inhalation on pain after propofol and rocuronium injection. J Anesth. 2013; 27:868–873. PMID:
23982855.

13. Choi YJ, Park HS, Lee H, Yoon SZ. Single pretreatment of remifentanil may reduce pain after propofol and rocuronium injection in rapid sequence induction. Korean J Anesthesiol. 2012; 63:413–418. PMID:
23198034.

14. Shin YH, Choi SJ, Jeong HY, Kim MH. Evaluation of dose effects of magnesium sulfate on rocuronium injection pain and hemodynamic changes by laryngoscopy and endotracheal intubation. Korean J Anesthesiol. 2011; 60:329–333. PMID:
21716962.

15. Yoon JS, Jeon HJ, Cho SS, Lee JD, Kang KO, Ryu SW, et al. Effect of pretreatment with gabapentin on withdrawal movement associated with intravenous rocuronium injection. Korean J Anesthesiol. 2011; 61:367–371. PMID:
22148083.

16. Shin YH, Kim CS, Lee JH, Sim WS, Ko JS, Cho HS, et al. Dilution and slow injection reduces the incidence of rocuronium-induced withdrawal movements in children. Korean J Anesthesiol. 2011; 61:465–469. PMID:
22220222.

17. Yoon JR, Jeon Y, Yoo Y, Shin HJ, Ahn JH, Lim CH. The analgesic effect of remifentanil on prevention of withdrawal response associated with the injection of rocuronium in children: no evidence for a peripheral action. J Int Med Res. 2010; 38:1795–1800. PMID:
21309495.

18. Kim YH, Go YK, Lee JU, Chung WS, Shin YS, Han KC, et al. Pretreatment with nafamostat mesilate, a kallikrein inhibitor, to decrease withdrawal response associated with rocuronium. J Anesth. 2010; 24:549–552. PMID:
20499255.

19. Lee SS, Yoon H. A comparison of the effect of lidocaine or sodium bicarbonate mixed with rocuronium on withdrawal movement, mean arterial pressure and heart rate during rocuronium injection. J Korean Acad Nurs. 2009; 39:270–278. PMID:
19411798.

20. Kim JH, Kim JH, Han SH, Hwang JW, Oh AY. Alfentanil is comparable to remifentanil in preventing withdrawal movement following rocuronium injection. J Clin Anesth. 2009; 21:9–12. PMID:
19232934.

21. Lee YC, Jang YH, Kim JM, Lee SG. Rapid injection of rocuronium reduces withdrawal movement on injection. J Clin Anesth. 2009; 21:427–430. PMID:
19833276.

22. Oh AY, Seo KS, Goo EK, Park YO, Kim SJ, Kim JH. Prevention of withdrawal movement associated with injection of rocuronium in children: comparison of remifentanil, alfentanil and fentanyl. Acta Anaesthesiol Scand. 2007; 51:1190–1193. PMID:
17711566.

23. Kim KS, Kim YS, Jeon WJ, Yeom JH. Prevention of withdrawal associated with the injection of rocuronium in adults and children. J Clin Anesth. 2006; 18:334–338. PMID:
16905077.

24. Park SH, Oh AY, Goo EK, Nahm FS, Min SW, Hwang JW, et al. A short period of inhalation induction with sevoflurane prevents rocuronium-induced withdrawal in children. Acta Anaesthesiol Scand. 2011; 55:87–91. PMID:
21126238.

25. Jeon Y, Baek SU, Park SS, Kim SO, Baek WY, Yeo JS. Effect of pretreatment with acetaminophen on withdrawal movements associated with injection of rocuronium: a prospective, randomized, double-blind, placebo controlled study. Korean J Anesthesiol. 2010; 59:13–16. PMID:
20651992.

26. Lee HJ, Han SJ, Kim H, Lee IO, Kong MH, Kim NS, et al. Antihistamine pretreatment to reduce incidence of withdrawal movement after rocuronium injection. J Korean Med Sci. 2009; 24:879–882. PMID:
19794987.

27. Lee JI, Lim SH, Lee SE, Kim YH, Lee JH, Lee KM, et al. Priming technique can alleviate the withdrawal responses associated with intravenous administration of rocuronium. Korean J Anesthesiol. 2009; 56:628–633.

28. Kim JY, Kwak HJ, Kim JY, Park KS, Song JS. Prevention of rocuronium-induced withdrawal movement in children: a comparison of remifentanil with alfentanil. Paediatr Anaesth. 2008; 18:245–250. PMID:
18230068.

29. Choi BI, Choi SH, Shin YS, Lee SJ, Yoon KB, Shin SK, et al. Remifentanil prevents withdrawal movements caused by intravenous injection of rocuronium. Yonsei Med J. 2008; 49:211–216. PMID:
18452256.

30. Kim JY, Kim JY, Kim YB, Kwak HJ. Pretreatment with remifentanil to prevent withdrawal after rocuronium in children. Br J Anaesth. 2007; 98:120–123. PMID:
17065169.

31. Cho K, Lee SH, Lee W, Chu BK, Kim MH, Lim SH, et al. Effect of pretreatment with palonosetron on withdrawal movement associated with rocuronium injection. Korean J Anesthesiol. 2014; 66:23–27. PMID:
24567809.

32. Jung JD, An TH, Song HS. The dose-dependent effect of remifentanil for withdrawal responses on injection of recuronium in children. Anesth Pain Med. 2009; 4:170–173.
33. Lee JY, Lee KC, Kim HS, Bang MS, Chang YJ. The dose-dependent effect of alfentanil on the rocuronium induced withdrawal in children. Anesth Pain Med. 2009; 4:348–351.
34. Kwak HJ, Kim YB, Kim EJ, Kim JY. Prevention of rocuronium-induced withdrawal movement in children: a comparison of remifentanil with lidocaine. Korean J Anesthesiol. 2008; 54:437–440.

35. Park SE, Park SH, Cho YW, Son HW, Lee JH, Kim DY. Hemodynamic Responses of Pretreatments Designed to Reduce Withdrawal Movements Following Rocuronium Injection: A Comparison of Alfentanil with Lidocaine. Korean J Anesthesiol. 2008; 54:507–512.

36. Baek SH, Woo CM, Lee HJ, Yoon JY, Kwon JY, Shin SW. Rocuronium-induced withdrawal movements associated with different Rocuronium injection method. Paediatr Anaesth. 2008; 18:515–519. PMID:
18312520.

37. Kim YH, Yoon MJ. Dilution of rocuronium with 0.9% NaCl reduces withdrawal movement during anesthetic induction. Anesth Pain Med. 2007; 2:22–25.
38. Kim YS, Lee JA. The effect of dilution with 0.9% normal saline on reducing withdrawal movement induced by rocuronium injection. Anesth Pain Med. 2007; 2:26–29.
39. Park SJ, Lee JY, Jee DL. The effect of rocuronium diluted with 0.9% NaCl on withdrawal response during injection in pediatric patients. Korean J Anesthesiol. 2006; 51:157–161.

40. Woo CM, Baek SH, Kim CH, Kwon JY, Kim HK, Shin SW. Comparison of withdrawal movement and intubating condition by the methods of rocuronium injection. Korean J Anesthesiol. 2006; 51:663–668.

41. Choi HG, Kim DS, Chang TH, Kim SH, Kim KH, Ryu SJ. Appropriate dosage of 8.4% sodium bicarbonate for preventing injection pain of rocuronium during anesthetic induction. Korean J Anesthesiol. 2006; 51:162–166.

42. Jung SM, Kim SH, Lim YS, Kwon HU, Kang PS, Park CW. The effect of sodium bicarbonate or lidocaine mixed with rocuronium on withdrawal movement in pediatric patient. Korean J Anesthesiol. 2005; 48:514–519.
43. Park JT, Choi JC, Yoo YS, Lee YB, Kim SY, Lim HK. The effect of pretreatment with thiopental on reducing pain induced by rocuronium injection. Yonsei Med J. 2005; 46:765–768. PMID:
16385651.

44. Jung JD, An TH, Yang IH, Wee HW, Eun SS, Han SY. The effect of pretreatment with lidocaine on withdrawal movement associated with injection of rocuronium in pediatric patients. Korean J Pediatr Anesth. 2005; 9:31–35.
45. Lee YK, Choi WJ, Kang WC, Leem JG, Yang HS. The effects of lidocaine on pain due to rocuronium. Korean J Anesthesiol. 2004; 46:145–150.

46. Chang SH, Kim HY, Park JY, Lee HW, Lim HJ, Yoon SM. The preventive effect of lidocaine on the withdrawal associated with the injection of rocuronium in children. Korean J Anesthesiol. 2004; 46:665–669.

47. Hwang SM, Oh MS, Lim SY. Effect of sodium bicarbonate or lidocaine mixed with rocuronium on withdrawal movement during rocuronium injection. Korean J Anesthesiol. 2004; 46:160–163.

48. Cheong SH, Kim SY, Lee KM, Choe YK, Kim YJ, Park JW, et al. The effect of pretreatment with ketamine on vascular pain due to an intravenous rocuronium injection in pediatric patients. Korean J Anesthesiol. 2003; 45:447–450.

49. Kim KS, Chae YJ, Pak SY, Cho HB, Kim JS. The effect of pretreatment with lidocaine for the withdrawal movement associated with the injection of rocuronium in children. Korean J Anesthesiol. 2002; 43:572–574.

50. Lockey D, Coleman P. Pain during injection of rocuronium bromide. Anaesthesia. 1995; 50:474. PMID:
7793569.

51. Moorthy SS, Dierdorf SF. Pain on injection of rocuronium bromide. Anesth Analg. 1995; 80:1067. PMID:
7726421.

52. Jalota L, Kalira V, George E, Shi YY, Hornuss C, Radke O, et al. Prevention of pain on injection of propofol: systematic review and meta-analysis. BMJ. 2011; 342:d1110. PMID:
21406529.

53. Akkaya T, Toygar P, Bedirli N, Yazicioglu D, Gumus H. Effects of pretreatment with lidocaine or ketamine on injection pain and withdrawal movements of rocuronium. Turk J Med Sci. 2008; 38:577–582.
54. Asida SM, Megalla SA, Korany A. Effect of fentanyl, lidocaine or, ketorolac on the prevention of pain during rocuronium injection. Egyptian Journal of Anaesthesia. 2009; 25:31–40.
55. Yavascaoglu B, Kaya FN, Ozcan B. Esmolol pretreatment reduces the frequency and severity of pain on injection of rocuronium. J Clin Anesth. 2007; 19:413–417. PMID:
17967668.

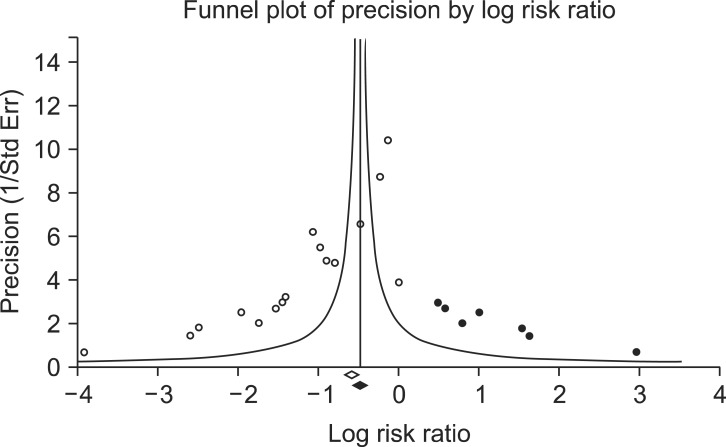
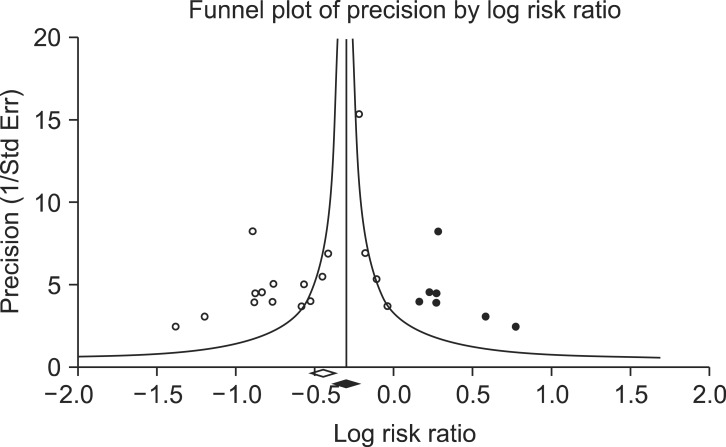
56. Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000; 56:455–463. PMID:
10877304.

57. Wood L, Egger M, Gluud LL, Schulz KF, Juni P, Altman DG, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. BMJ. 2008; 336:601–605. PMID:
18316340.

58. He J, Du L, Liu G, Fu J, He X, Yu J, et al. Quality assessment of reporting of randomization, allocation concealment, and blinding in traditional Chinese medicine RCTs: a review of 3159 RCTs identified from 260 systematic reviews. Trials. 2011; 12:122. PMID:
21569452.

59. Williamson PR, Gamble C, Altman DG, Hutton JL. Outcome selection bias in meta-analysis. Stat Methods Med Res. 2005; 14:515–524. PMID:
16248351.

60. Jüni P, Holenstein F, Sterne J, Bartlett C, Egger M. Direction and impact of language bias in meta-analyses of controlled trials: empirical study. Int J Epidemiol. 2002; 31:115–123. PMID:
11914306.

61. Cho HY, Kim DY, Chung RK. The effect of lidocaine or fentanyl on withdrawal movement during rocuronium injection. Korean J Anesthesiol. 2007; 53:174–179.

62. Kim SJ, Lee HY, An TH. Comparison of withdrawal responses associated with temperature and gender on the injection of rocuronium. Korean J Anesthesiol. 2004; 47:331–335.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download