Abstract
The survival rate after lung transplantation has increased in recent years, leading to an increase in non-pulmonary conditions that require surgical intervention. These post-transplant surgical procedures, however, are associated with high mortality and morbidity rates. Intra-abdominal conditions are the most common reasons for surgical intervention. We describe here two patients who underwent abdominal surgery under general anesthesia following lung transplantation. One patient underwent cholecystectomy due to cholecystitis after heart-lung transplantation, and the other patient had an exploratory laparotomy for duodenal ulcer perforation after double lung transplantation. Depending on the type of transplant intervention, the physiology of the transplanted lung must be considered for general anesthesia. Knowledge of underlying conditions and immunosuppressive therapy following transplantation are important for safe and effective general anesthesia.
The International Society for Heart and Lung Transplantation has reported that 34,102 adult lung transplantations were performed worldwide from 1995 to 2011. The most common reason for lung transplantation was chronic obstructive pulmonary disease (34%), followed by idiopathic pulmonary fibrosis (23%), and cystic fibrosis (17%). The overall median survival was 5.5 years, with 1- and 5-year survival rates of 79 and 53%, respectively, following lung transplantation, and 63 and 44%, respectively, following heart-lung transplantation [1]. Because the number of lung transplant survivors has increased, the need for surgical intervention for non-pulmonary conditions, such as peptic ulcer perforation, cholecystitis, and necrotising colitis, has also increased. These non-pulmonary conditions are caused by underlying diseases, post-transplant immunosuppressive treatment regimens, and the transplant procedure itself [2]. Safe and effective management of general anesthesia for surgical intervention in these patients requires consideration of the physiology of the transplanted lung and the effect of immunosuppressant agents. We describe here the management of two patients who underwent non-transplant surgery under general anesthesia following lung transplantation.
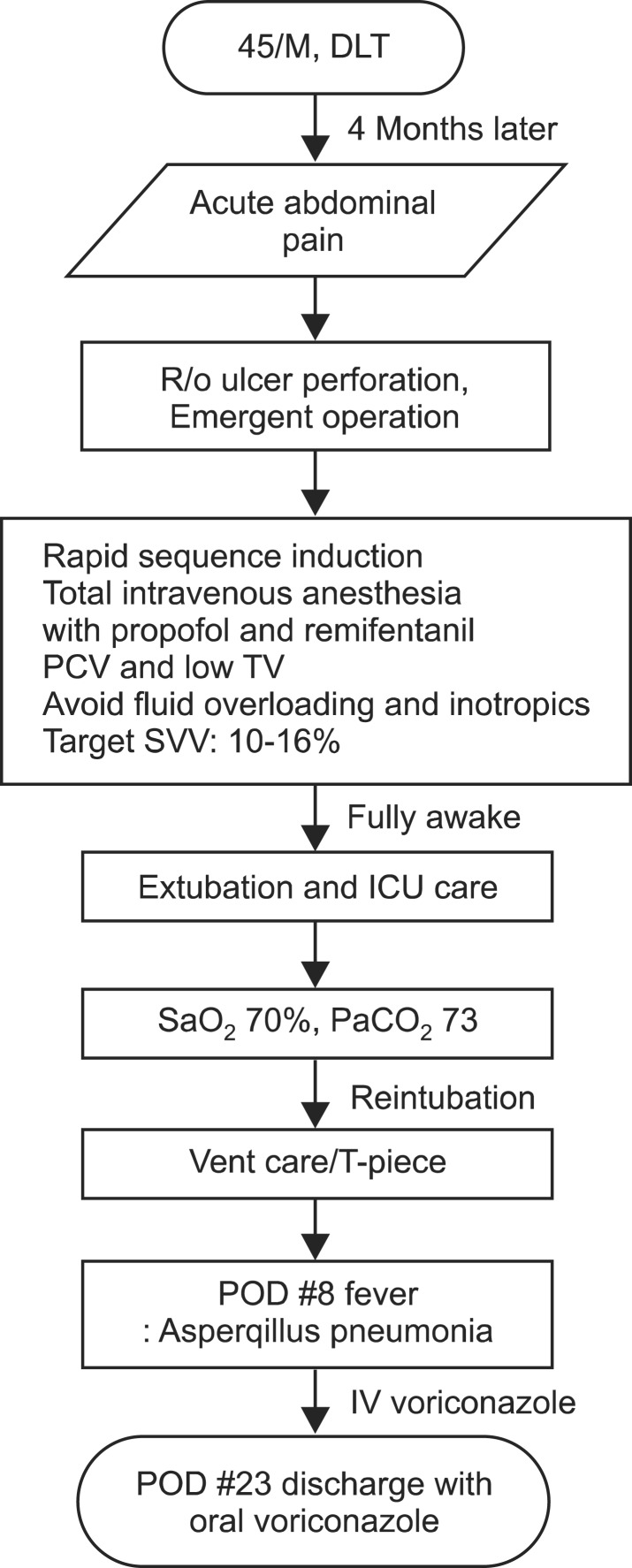
A 45-year-old man (51.5 kg, 161 cm) with idiopathic pulmonary fibrosis had undergone a double lung transplantation 4 months earlier. His antirejection protocol included tacrolimus 1.25 mg/day, prednisolone 7.5 mg/day, and mycophenolate mofetil 500 mg bid. Three months following transplantation, he was diagnosed with steroid-induced diabetes mellitus and cholecystitis. One month later, the patient was admitted to the emergency room for abdominal pain. Abdominal X-rays and computed tomography showed a small bowel perforation requiring an emergency operation. Pulmonary function tests showed moderately restrictive disease; his functional vital capacity (FVC) was 44%, his forced expiratory volume in one second (FEV1.0) was 46%, and his FEV1.0/FVC ratio was 89. Before anesthesia, he gargled his mouth and throat with povidone-iodine. General anesthesia was induced using etomidate 10 mg and succinylcholine 75 mg, and rapid sequence intubation was performed with an 8.0 mm internal diameter single lumen tube. Anesthesia was maintained with propofol, remifentanil and rocuronium. Propofol and remifentanil were administered using a target-controlled infusion (TCI) device (Orchestra®, Fresenius Vial, Brezins, France), which calculates infusion rate according to the patient's body weight and height and measures the plasma concentration of drug, to maintain the effective site concentrations of propofol and remifentanil at 1-1.2 µg/ml and 7-10 ng/ml, respectively; and rocuronium was continuously infused at 20 mg/hr. The ventilator was set to pressure control mode with a peak inspiratory pressure (PIP) between 16-18 cmH2O and a respiratory rate of 12 breaths per minute to protect the transplanted lung. A tidal volume of approximately 300 ml was achieved, with a positive end-expiratory pressure (PEEP) of 5 cmH2O. Direct intraarterial pressure with stroke volume variation was monitored, as well as pulse oximetry, temperature, end-tidal carbon dioxide tension, and non-invasive blood pressure. A central venous catheter was placed in the right jugular vein, with initial central venous pressure of 15 mmHg. Intraoperative arterial blood gas analysis (ABGA) indicated pH 7.37, PaCO2 34 mmHg, PaO2 274 mmHg, HCO3- 19.7 mEq/L, and 100% O2 saturation (SaO2) with 0.5 fraction of inspired oxygen (FiO2). The surgical finding was duodenal ulcer perforation and primary closure was performed. The total operating time was 2 hours and 35 minutes. The total amounts of intraoperative fluids were 400 ml of plasmalyte and 500 ml of 6% hydroxyethyl starch in saline. Urine output during the surgery was 130 ml and estimated blood loss was less than 100 ml. Norepinephrine 0.5 µg/kg/min was infused intraoperatively to maintain his mean arterial pressure above 60 mmHg. Central venous pressure was 15 mmHg at the end of the surgery and did not change during the operation, and stroke volume variation was maintained between 10 and 16%. The patient's trachea was extubated at the end of the surgery with a tidal volume greater than 300 ml, during spontaneous ventilation, and when fully awake. However, the patient required re-intubation in the intensive care unit 1 hour later due to respiratory failure. His SaO2 fell down below 70% despite ambu-bagging with 15 L/min of O2, with ABGA showing a pH of 7.03 and a PaCO2 of 73 mmHg. He was maintained on mechanical ventilation in pressure control mode and PEEP for 7 hours and changed to T-piece at dawn, with ABGA showing pH 7.36, PaCO2 36 mmHg, PaO2 163 mmHg, HCO3- 20 mEq/L, SaO2 99%, and FiO2 0.5. He was extubated on the morning of postoperative day 1. After extubation, the patient complained of dyspnea and a high-pitched stridor was heard. Dexamethasone 10 mg was injected intravenously and his respiration was maintained with nasal prong O2 2 L without difficulty. The patient's immunocompressive protocol was maintained throughout the perioperative period. However, fever was observed and the patient was diagnosed with aspergillus pneumonia on postoperative day 8. The pneumonia was treated with intravenous voriconazole and the patient was discharged on postoperative day 23 with oral voriconazole (Fig. 1).
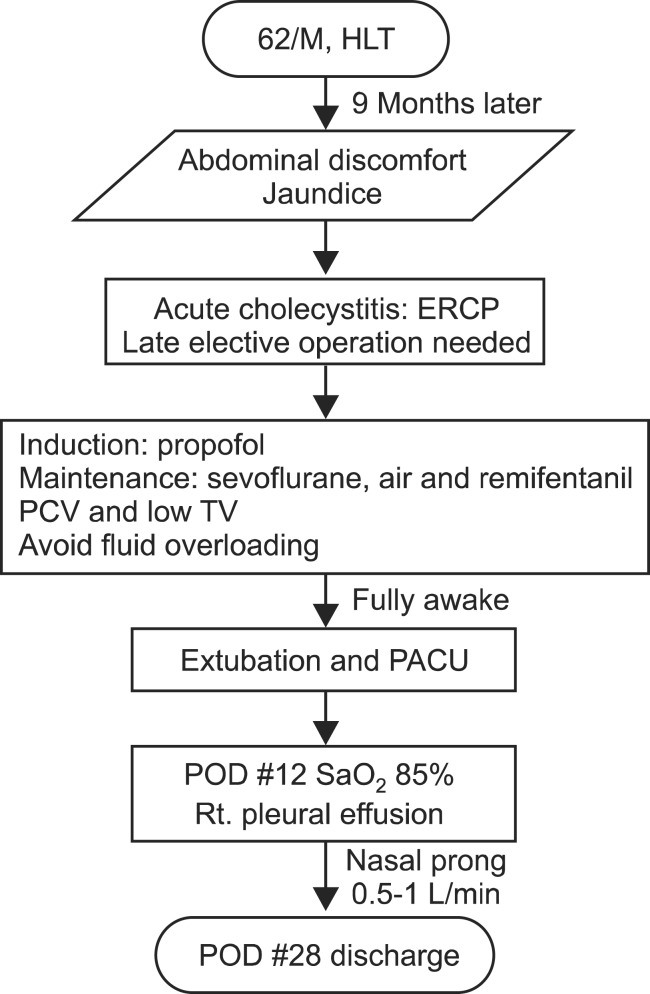
A 62-year-old male patient (50 kg, 164.5 cm) with idiopathic pulmonary fibrosis, severe resting pulmonary hypertension and a 45 mmHg pressure gradient between the right ventricle and right atrium had undergone heart-lung transplantation 9 months earlier. He experienced an acute kidney injury after the transplantation, for which he received continuous renal replacement therapy in the intensive care unit, but progressed to endstage renal disease without recovery. He was hospitalized for 7 months after the transplantation for repeated infections with aspergillus and cytomegalovirus, gastroduodenal bleeding, and for rehabilitation treatment. His immunocompressive protocol consisted of tacrolimus 2 mg/day, prednisolone 7.5 mg/day and mycophenolate mofetil 500 mg bid. One month after discharge, the patient was re-admitted to the hospital for abdominal discomfort and jaundice. Ultrasonography suggested acute cholecystits resulting from gall bladder sludge and endoscopic retrograde cholangiopancreatography was chosen for treatment. However, due to his liver enzyme levels being elevated over 150 mg/dl, open cholecystectomy was performed instead. His pulmonary function test showed severe restrictive disease; his FVC was 26%, his FEV1.0 was 31%, and his FEV1.0/FVC ratio was 91. General anesthesia was induced with propofol 60 mg and vecuronium 4 mg, and maintained with 1.5-2% sevoflurane and remifentanil 3-7 ng/ml with TCI. A single lumen 8.0 mm internal diameter endotracheal tube was used for intubation and the ventilator was set to pressure control mode of 20-22 cmH2O PIP and a respiratory rate of 14 breaths per minute with 5 cmH2O PEEP. The total operating time was 1 hour and 40 minutes, with a total of 700 ml of Ringer's lactate solution fluid infused during the operation. Estimated blood loss was less than 50 ml, but urine output was not checked as there was no Foley catheter. His trachea was extubated at the end of surgery. On postoperative day 12, the patient's SaO2 decreased below 85%, and nasal prong O2 0.5-1 L/min was administered. ABGA revealed pH 7.288, PaCO2 56.2 mmHg, PaO2 102 mmHg, HCO3- 27.2 mEq/L, and 97% SaO2 with 1 L/min O2 delivered via nasal prongs. A chest X-ray showed right pleural effusion, but the patient improved after receiving intravenous furosemide for 1 week. The patient continued to receive immunosuppressive agents throughout the perioperative period and was discharged 4 weeks after surgery (Fig. 2).
Lung transplantation has become a reliable option for treatment of end-stage respiratory disease in recent years, with improved outcomes credited to aggressive perioperative care. However, lung transplantation survivors still face high morbidity and mortality and usually need continuous medical treatment throughout their lives. The most common causes of death are graft failure and non-cytomegalovirus infection within the first year, and bronchiolitis obliterans syndrome and non-cytomegalovirus infection after the first year. The risk factors for complications within the first year include the patient's underlying lung disease, acute rejection, and infection. The risk factors after 1 year are similar, but may also include immunosuppressive therapy. Immunosuppression can be divided into induction and maintenance therapy, with agents used similar following lung and heart-lung transplantation. Induction agents include interleukin-2 receptor antagonist, alemtuzumab, anti-thymocyte globulin and anti-lymphocyte globulin, but the use of induction therapy is decreasing. Maintenance therapy consists of combination regimens, with the most frequently commonly used being tacrolimus- and cyclosporine-based regimens. The optimal regimens include tacrolimus plus either mycophenolate mofetil or azathioprine. Immunosuppressive agents, however, contribute to the development of diabetes, hypertension, renal dysfunction, osteoporosis, and malignancy. Hypertension and diabetes have been shown to develop in 82.9 and 40.5% of patients, respectively within 5 years of lung transplantation [1,2,3].
Although the incidence of patients requiring surgical intervention after lung transplantation has not been determined, it is generally higher than for non-transplant patients. These findings are similar to those observed following the transplantation of other organs, with post-transplantation complications resulting from patients' immunocompromised status, their underlying diseases, and the transplantation procedure itself. For example, the incidence of major non-pulmonary surgical procedures in lung transplant recipients was found to be 17.7% [2]. The mortality rate during the first month after lung transplantation was 50%, but only 9.1% after 1 month. Emergency operations were associated with a 35.7% mortality rate, compared with 0% for elective operations. The incidence of abdominal processes among lung transplant recipients was reported to be 21%, with bowel obstruction being the most common cause, followed by peptic ulcer and cholestasis [4].
It is important to determine a patient's general status, medications, and transplanted lung physiology before general anesthesia. Pulmonary function tests, exercise tests, and re-hospitalization can be helpful in evaluating the functional status of the patient after lung transplantation. Medications, including immunosuppressants, antihypertensives, and diuretics, should be continued up to the day of surgery and restarted as soon as possible following surgery [3,5].
The physiology of the transplanted lung should also be considered when selecting ventilator modes and parameters for general anesthesia. During the first month after transplantation, the total vital capacity and the first second forced expiratory volume usually decrease, thereafter increasing gradually, while PaCO2 values tend to normalize within 15 days. Lung denervation during transplantation has minimal effect on airway tone and hypoxic pulmonary vasoconstriction. As lymphatic drainage is interrupted during trachea and bronchial resection, the transplanted lung is highly susceptible to volume overload; therefore, extreme caution must be exercised to avoid fluid overloading and pulmonary edema [3,6,7,8].
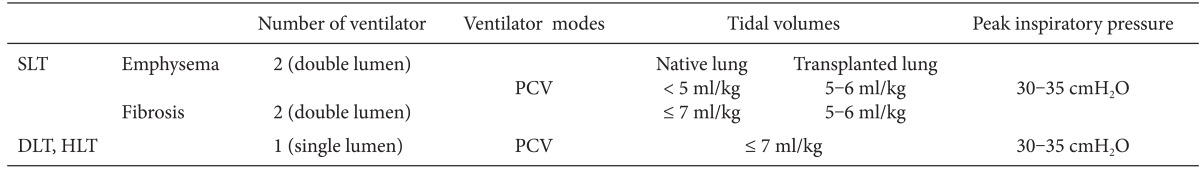
Barotrauma is another important factor to consider during general anesthesia in the transplanted lung. In double lung transplantation, consideration of ventilation management to avoid one-sided lung hyperinflation is not needed. However, in single lung transplantation, the compliance of the native lung differs from that of the transplanted lung, with ventilator flow directed towards the more compliant lung. Emphysema patients who receive a single lung transplant may develop over distension of the native lung; pulmonary fibrosis patients who receive a single lung may experience over distension of the transplanted lung. Two ventilator machines may be required, one for each lung, in patients with a single transplanted lung who also have a diseased native lung. Hyperinflation of one lung can result in mediastinal shifting and pneumothorax. To protect the less compliant lung, a low tidal volume of less than 7 ml/ideal body weight, pressure control mode, PEEP, and a high respiratory rate are recommended. Tidal volume should be reduced to avoid hypocapnia, especially during single lung ventilation. Limiting PIP to 30-35 cmH2O and plateau pressure to 20-25 cmH2O is recommended to avoid barotrauma at the anastomosis site and alveoli (Table 1). A PEEP of 5-8 cmH2O is indicated for patients who undergo double lung transplantation [3,9,10].
Although propofol, thiopental sodium, and etomidate can be used to induce anesthesia, etomidate is preferred when there is a risk of hemodynamic instability. TCI with propofol plus remifentanil, or a volatile agent plus remifentanil, is suitable for maintaining anesthesia. Cisatracurium, rocuronium, vecuronium, and mivacurium are all suitable for neuromuscular blockade, but the recovery time and amount should be considered [11]. Care should be taken with tracheal intubation in double lung transplant recipients because of possible injury to the anastomosis site. Since bronchodilators are not effective with repeated graft rejection, deep anesthesia should be maintained to avoid bronchospasm due to airway hyper-reactivity [12].
For our two patients, we used different kinds of neuromuscular blocks, anesthetic induction agents, and maintenance methods. Neuromuscular blockers such as rocuronium and cisatracurium were suitable for muscle relaxation, and induction agents such as propofol and etomidate induced rapid loss of consciousness without hemodynamic instability. Both maintenance methods, propofol plus remifentanil and sevoflurane plus remifentanil, provided suitable hemodynamic stability. As both our patients had undergone double lung transplantation, we used a single lumen tube and a single ventilator machine for abdominal surgery. We used a pressure control mode to protect the graft and maintain low tidal volumes of less than 7 ml/kg with PIP less than 30 cmH2O. Since the tracheal anastomosis site may be injured in double lung transplant recipients, caution is needed when performing endotracheal intubation. Fiberoptic bronchoscope, videoscope, and optiscope are helpful in examining the anastomosis site while intubating. Since the anastomosis sites of the trachea were intact in both our patients, intubation was not problematic. In patients who undergo single lung transplantation, two ventilator machines would be used via a double lumen tube to isolate the native and engrafted lungs. In Patient 1, we inserted arterial and central venous catheters to monitor hemodynamic changes due to the emergency nature of the surgery; however, in general, invasive procedures should be minimized to avoid infection. Also, fluid was infused cautiously to avoid pleural effusion, with inotropic agents chosen to elevate the mean arterial pressure. Central venous pressure and stroke volume variation were monitored to assess volume status. Stroke volume variation is reportedly affected by the depth of tidal volume, with this variation lower in patients with low tidal volume [13]. Even when tidal volume is lower, measuring stroke volume variation from the beginning of the operation can predict intravascular volume status compared with baseline. Awareness of this limitation is important, as is follow up of the accuracy of dynamic indices. This patient's postoperative respiratory failure was considered to result from the inappropriate recovery of spontaneous respiration and laryngeal edema. He recovered after prolonged mechanical ventilation and dexamethasone injection. We did not administer intraoperative steroid injections to either patient due to the short operating time and their routine treatment with steroids, but additional steroids may be necessary during long and stressful procedures.
As the number of patients undergoing lung transplantation increases, so will those who require general anesthesia for non-pulmonary surgery. A review of each patient's general status and medications, as well as an awareness of any complications developing after transplantation, must be considered. Intraoperative ventilator settings should depend on whether a patient has received a single or double lung transplantation, and a strict perioperative aseptic technique of postoperative lung care is required to recover normal lung function. Measures to protect the transplanted lung include a pressure control mode ventilator with PEEP, a low tidal volume of less than 7 ml/kg with PIP less than 30 cmH2O, single lumen ventilation in double lung transplant recipients and double lumen ventilation with two ventilators in single lung transplant recipients, and minimal fluid therapy.
References
1. Christie JD, Edwards LB, Kucheryavaya AY, Benden C, Dipchand AI, Dobbels F, et al. The Registry of the International Society for Heart and Lung Transplantation: 29th adult lung and heart-lung transplant report-2012. J Heart Lung Transplant. 2012; 31:1073–1086. PMID: 22975097.

2. Wekerle T, Klepetko W, Wisser W, Senbaklavaci O, Artemiou O, Zuckermann A, et al. Incidence and outcome of major non-pulmonary surgical procedures in lung transplant recipients. Eur J Cardiothorac Surg. 1997; 12:718–723. PMID: 9458142.

3. Feltracco P, Falasco G, Barbieri S, Milevoj M, Serra E, Ori C. Anesthetic considerations for nontransplant procedures in lung transplant patients. J Clin Anesth. 2011; 23:508–516. PMID: 21911200.

4. Miller CB, Malaisrie SC, Patel J, Garrity E, Vigneswaran WT, Gamelli RL. Intraabdominal complications after lung transplantation. J Am Coll Surg. 2006; 203:653–660. PMID: 17084326.

5. Studer SM, Levy RD, McNeil K, Orens JB. Lung transplant outcomes: a review of survival, graft function, physiology, health-related quality of life and cost-effectiveness. Eur Respir J. 2004; 24:674–685. PMID: 15459149.

6. Paradis I, Yousem S, Griffith B. Airway obstruction and bronchiolitis obliterans after lung transplantation. Clin Chest Med. 1993; 14:751–763. PMID: 8313678.

7. Robin ED, Theodore J, Burke CM, Oesterle SN, Fowler MB, Jamieson SW, et al. Hypoxic pulmonary vasoconstriction persists in the human transplanted lung. Clin Sci (Lond). 1987; 72:283–287. PMID: 3545645.

8. Sugita M, Ferraro P, Dagenais A, Clermont ME, Barbry P, Michel RP, et al. Alveolar liquid clearance and sodium channel expression are decreased in transplanted canine lungs. Am J Respir Crit Care Med. 2003; 167:1440–1450. PMID: 12738601.

9. Samarutel J. Evidence-based medicine for lung-protective ventilation: the emperors new clothes for doubtful recommendations? Acta Anaesthesiol Scand. 2010; 54:42–45. PMID: 19878102.
10. Montes FR, Pardo DF, Charrís H, Tellez LJ, Garzón JC, Osorio C. Comparison of two protective lung ventilatory regimes on oxygenation during one-lung ventilation: a randomized controlled trial. J Cardiothorac Surg. 2010; 5:99. PMID: 21044330.

11. Sarkar M, Laussen PC, Zurakowski D, Shukla A, Kussman B, Odegard KC. Hemodynamic responses to etomidate on induction of anesthesia in pediatric patients. Anesth Analg. 2005; 101:645–650. PMID: 16115968.

12. Subramony SH, Carpenter DE, Raju S, Pride M, Evans OB. Myopathy and prolonged neuromuscular blockade after lung transplant. Crit Care Med. 1991; 19:1580–1582. PMID: 1683618.

13. Reuter DA, Bayerlein J, Goepfert MS, Weis FC, Kilger E, Lamm P, et al. Influence of tidal volume on left ventricular stroke volume variation measured by pulse contour analysis in mechanically ventilated patients. Intensive Care Med. 2003; 29:476–480. PMID: 12579420.

Fig. 1
Flow chart of case 1 emergency operation course. DLT: double lung transplantation, PCV: pressure control mode, TV: tidal volume, SVV: stroke volume variation, ICU: intensive care unit, SaO2: O2 saturation, PaCO2: arterial carbon dioxide tension, POD: postoperative day.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download