This article has been
cited by other articles in ScienceCentral.
Abstract
Calcification of the cardiac chambers is among the challenges associated with reoperative cardiac surgeries by increasing the risk of systemic embolization. We experienced a case of an unexpected detected mass by intraoperative transesophageal echocardiography during weaning from cardiopulmonary bypass in a patient undergoing trido mitral and tricuspid valve replacement surgery. The surgically removed mass was identified as calcified tissue. This case shows the importance of careful echocardiographic evaluation of the left heart in patients undergoing repeat valve surgery given their greater potential for embolic sources.
Go to :

Keywords: Calcification, Cardiac surgery, Left atrium, Reoperation, Transesophageal echocardiography
With an increase in the aging population, increasing numbers of patients are referred for repeat valve surgery. One of the important risk factors that should not be overlooked in the redo surgeries we encounter is the presence of numbers of potential sources of embolism. The presenting case emphasizes the importance of careful evaluation of the left heart by transesophageal echocardiography (TTE) in patients undergoing redo surgery given their greater potential for embolic sources.
Case Report
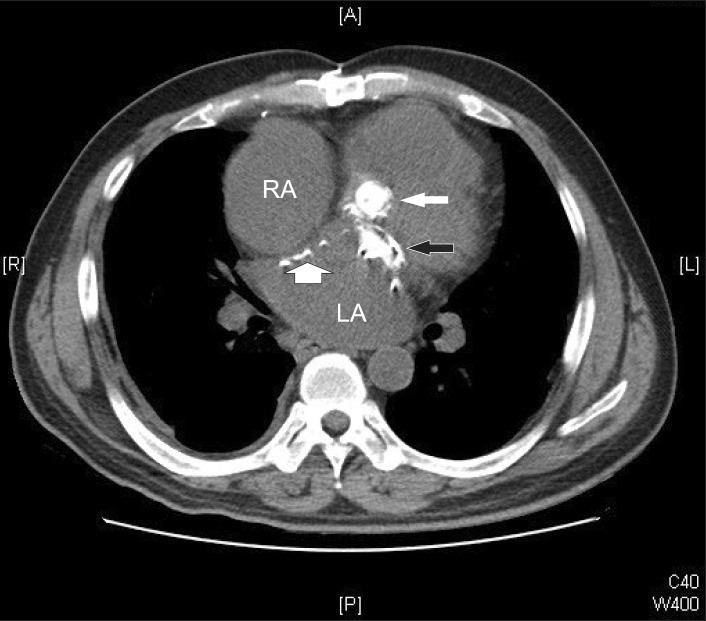
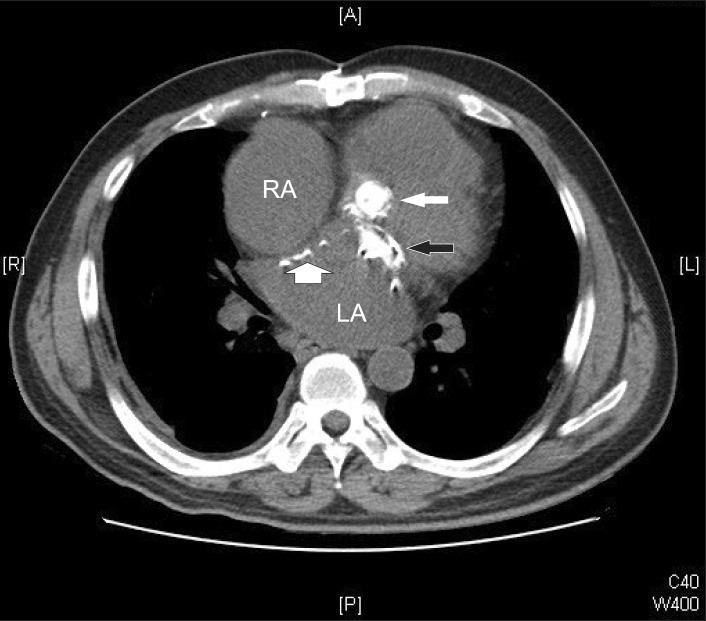
A 55-year-old male patient was referred for trido mitral and tricuspid valve replacement surgery. He underwent mitral and aortic valve replacement for rheumatic heart disease when he was 22 years old. The second mitral and aortic valve replacement was performed 12 years later for prosthesis degeneration. The surgery was performed with the right atrial trans-septal approach because of the severe adhesions of the left atrium (LA). Preoperative transthoracic echocardiography revealed a mitral paravalvular leak of moderate severity and severe tricuspid regurgitation combined with tricuspid stenosis. Chest computed tomography showed dense calcifications of the mitral and aortic prosthesis and the interatrial septum (IAS) (
Fig. 1). He was in atrial fibrillation medicated with oral anticoagulant and no atrial mass was noted. Cardiopulmonary bypass (CPB) was established with femoro-femoral cannulation. The mitral valve was approached by trans-septal incision again and a heavily calcified IAS was noted. After completion of the surgery, weaning from CPB commenced. As the pump flow was gradually reduced, an unexpected hyper-echogenic peanut-sized free-floating left atrial mass was detected on the TEE (
Fig. 2). Immediate aortic cross clamp and cardioplegic arrest were re-instituted in order to prevent its systemic embolization and to remove it. Septostomy and irrigation of the LA revealed that the mass was a 15 × 10 mm sized yellowish bony tissue, which was later confirmed as "dense fibrosis and calcification" (
Fig. 3). The follow-up TEE was clear of any mass, and the CPB was weaned off uneventfully. The patient did not experience any postoperative embolic complications and was discharged on postoperative day 11 in good clinical condition.
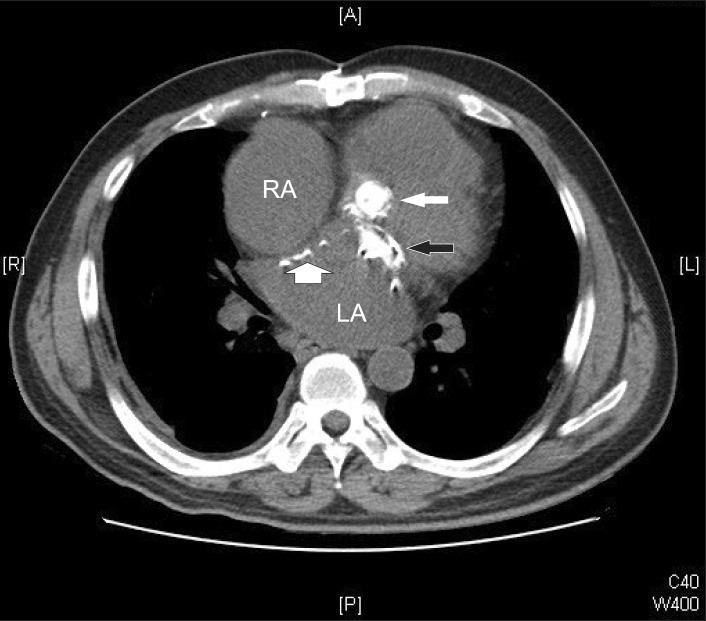 | Fig. 1Computed tomogram showing multiple calcifications of the interatrial septum (thick arrow) and the aortic (thin white arrow) and mitral (thin black arrow) prosthesis. LA: left atrium, RA: right atrium. 
|
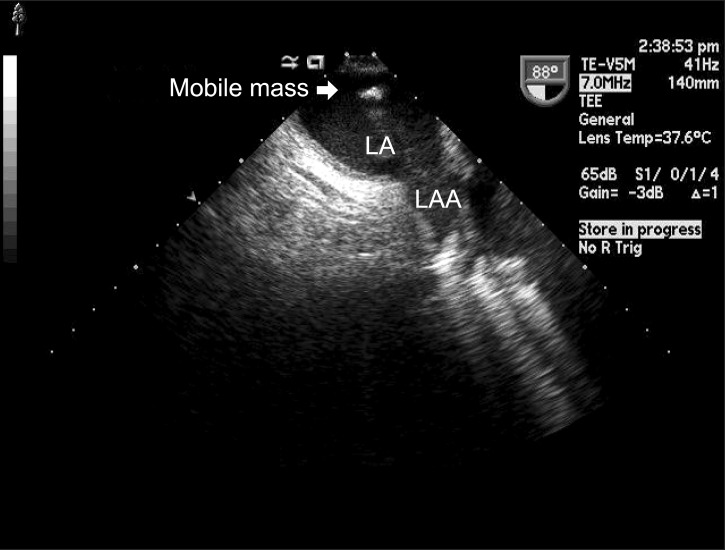 | Fig. 2The midesophageal 2-chamber view showing a hyper-echogenic free-floating left atrial mass. LA: left atrium, LAA: left atrial appendage. 
|
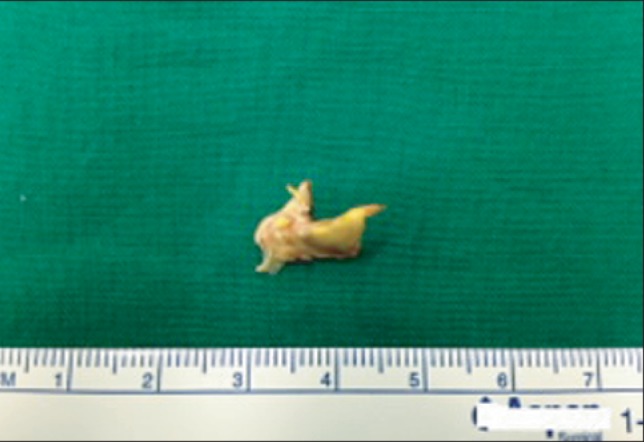 | Fig. 3The surgically removed calcified mass. 
|
Go to :

Discussion
Reoperative cardiac surgeries represent a high-risk entity for the presence of technical complexity, more advanced cardiac pathology, and the existence of more frequent comorbidities [
1]. One of the important issues that should not be overlooked, especially in the redo surgeries, is the presence of unusual embolic sources. The processes of fibrosis, thrombosis, and calcification around a first prosthesis are well postulated [
2]. Removal of a previous prosthetic valve accompanies the release of these materials, all of which should be cleaned out before the aortic cross-clamp is removed.
Cardiac chambers also undergo fibrosis and calcification following valve surgery, because it is damaged by the incisions, retractions, and manipulations. Previously, developments of massive left atrial calcifications associated with mitral valve replacement have been reported [
3,
4]. Besides surgical trauma, rheumatic valve disease itself can lead to calcification of the adjacent heart chambers. In patients with chronic rheumatic mitral disease, LA wall calcification is frequently observed, which is associated with rheumatic involvement of the endocardium and chronic strain forces originating from mitral pathology [
5]. Rarely, a massive LA calcification, a so called "coconut atrium", been reported. It is mostly observed in patients having a history of chronic rheumatic mitral disease with at least one previous surgery [
5]. Although the current case did not have massive calcification of the entire LA wall, the IAS was significantly calcified due to the trans-septal approach of the first redo surgery. To achieve a better surgical approach and easier closure of the incision, the calcified endocardium was dissected and removed during the second redo surgery. Unknowingly, one of the detached pieces of calcium debris that should have been removed was left in the LA despite careful irrigation and evacuation of visible particulate materials by the surgeon. If it had not been detected before the separation from CPB, devastating systemic embolization could have occurred in this patient.
TEE allows for a detailed evaluation of the entire LA by achieving a mid-esophageal (ME) four chamber view, two chamber view, and bi-caval view [
6]. In the supine and Trendelenburg positions during weaning from CPB, particulates in the LA with a greater specific gravity than that of blood migrate posteriorly and superiorly, while air bubbles float up against the septum. In the current case, the mass was detected at the posterior wall of the upper LA on the ME two chamber view with a slight withdrawal of the probe, which would not have been visible in the routinely assessed views. Thus, this case report highlights the importance of a more comprehensive evaluation of the suspected chambers to locate any untoward presence of debris, while taking into consideration potential sources of debris and details of the surgical procedure. To our knowledge, this is the first report describing the detection of missed surgical debris in the LA by TEE during CPB. However, it should be noted that this can possibly occur because there is always room for human error in the operative field. Careful evaluation of the left heart by TEE should not be discontinued until the patient is moved to an intensive care unit bed, especially for patients undergoing repeat valve surgery given their greater potential for embolic sources.
Go to :