Abstract
Background
Different tidal volume (TV) settings during mechanical ventilation alter intrathoracic blood volume, and these changes could alter central venous pressure and the cross sectional area (CSA) of the right internal jugular vein (RIJV). The aim of this study was to determine the optimal TV for maximizing the CSA of the RIJV in the supine and Trendelenburg positions in anesthetized patients.
Methods
Forty patients were randomly allocated to a supine group (Group S, n = 20) or a Trendelenburg group (Group T, n = 20) by computer generated randomization. RIJV CSAs were measured repeatedly after increasing the inspiratory volume in 1 ml/kg increments from a TV of 8 ml/kg to 14 ml/kg using ultrasound images.
The right internal jugular vein (RIJV) is a common site for central venous catheterization in anesthetized patients during major surgery, intensive care, or emergency care. Because the RIJV frequently overlaps the carotid artery, carotid artery puncture is the most common complication associated with landmark-guided IJV catheterization. Ultrasound (US) guided cannulation is ideal for preventing accidental arterial puncture, but in its absence or in an emergent situation, another method for facilitating central catheterization is required. Various means, such as, the Trendelenburg position, the valsalva maneuver, or positive end-expiratory pressure (PEEP) are frequently used to increase the cross-sectional area (CSA) of the RIJV [1-3] and facilitate catheterization [4]. However, the Valsalva maneuver or PEEP can interfere with hemodynamic stability during general anesthesia and the Trendelenburg position can cause ventilation and oxygenation difficulties in obese patients. Different tidal volume (TV) settings during mechanical ventilation alter inspiration-associated decreases in right ventricular stroke volume and intrathoracic blood volume [5], and these changes could alter central venous pressure and the CSA of the RIJV. Furthermore, in an animal study, an increase in TV was found to increase central venous pressure [6], which is closely correlated with the IJV CSA [7].
Despite the many reports issued on the practical aspects of central venous catheterization, no previous study has explored the association between the ease of central venous catheterization and tidal volume. We hypothesized that increments in TV would increase the CSA of the RIJV, and that this would simplify catheterization and minimize hemodynamic changes during the procedure.
Accordingly, the aim of this study was to determine the optimal TV required for maximizing the CSA of the RIJV and to document CSA changes induced by incrementally increasing TV in two different positions in anesthetized patients.
This study was approved by the Institutional Review Board and written informed consent was obtained from all eligible study participants.
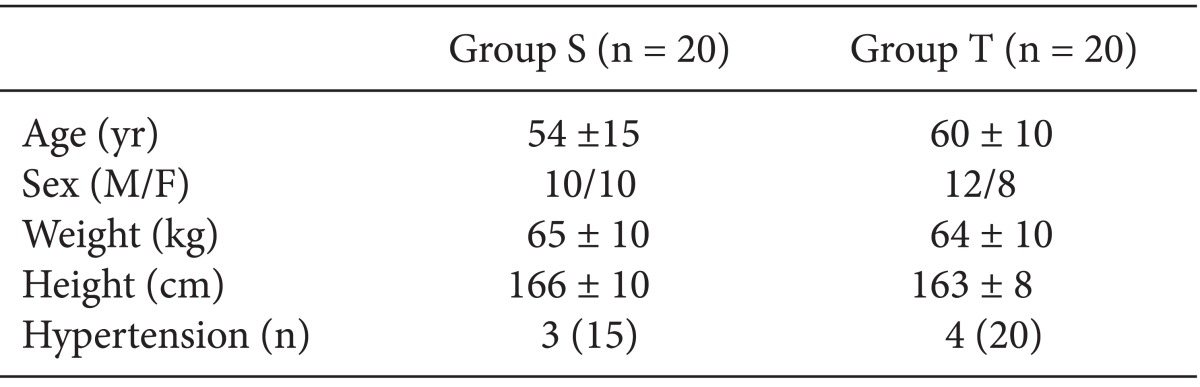
Forty adult patients of American Society of Anesthesiologists physical class I or II, aged 25 to 75 yr, and scheduled for major abdominal surgery were enrolled. Patients with a history of RIJV cannulation, uncontrolled hypertension, congestive heart failure, valvular heart disease, diabetes mellitus, chronic obstructive pulmonary disease, or a cervical spinal disorder were excluded. Patients were randomly allocated to a supine group (Group S, n = 20) or a Trendelenburg group (Group T, n = 20) by computer generated randomization. All patients were administered 300 ml of plasma solution prior to anesthesia. On arrival at the operating room, standard monitors were applied. Anesthesia was induced with propofol 1.5-2.0 mg/kg, rocuronium 0.6 mg/kg, and remifentanil 0.5 µg/kg. After tracheal intubation, anesthesia was maintained with sevoflurane in a 50% oxygen/air mix. Lungs were ventilated (Primus anesthesia workstation®, Dräger, Lübeck, Germany) at a TV of 8 ml/kg and a respiratory rate of 10 breaths/min. After 5 min of intubation, patients were placed either supine or in the 10° Trendelenburg position with head rotated 20° to the left side. On the right side of the neck, transverse ultrasound images (including the RIJV and carotid artery) were obtained at the cricoid level parallel to the clavicle. A high-frequency linear ultrasound transducer (LOGIQe®, GE Healthcare, Wauwatosa, USA) was then placed as lightly as possible to avoid RIJV compression. This measurement was repeated after increasing the inspiratory volume in 1 ml/kg increments from a TV of 8 ml/kg to 14 ml/kg. The ventilatory rate was kept at 10 breaths/min with an I : E ratio of 1 : 2 to maintain a constant respiratory cycle. Ultrasound (US) images were obtained at the end-inspiratory phase of the 5th respiratory cycle at every TV. Peak inspiratory pressure (PIP), mean arterial pressure (MAP), heart rate (HR), and end tidal carbon dioxide (EtCO2) were recorded at all TV levels. When MAP decreased to < 70% of baseline during measurement, TV was decreased to 8 ml/kg and measurements were discontinued. US-measurements were performed by a single experienced anesthesiologist.
After completing all measurements, anesthetic procedures were initiated and surgery was started.
On US images, the CSA of the RIJV were measured using a built-in caliper. Dimensions were measured as previously described [8]. When a mean difference and SD of the RIJV CSA between 8 ml/kg and 14 ml/kg of TV were taken to be 0.6 mm2 and 0.6 mm2 as was determined based on a preliminary study in 6 patients, 16 subjects were required for an α value of 0.05 and a power of 80%. Thus, 20 subjects were included per group to cope with an expected loss of 20%. The statistical analysis was performed using PASW Statistics 13® (SPSS Inc, Chicago, IL, USA). Results are expressed as means ± SDs or as numbers of patients. Patient characteristics were compared using the student's t-test or Fisher's exact test as appropriate. Intergroup comparisons were performed using the independent t test and intragroup comparisons using repeated measures ANOVA with Bonferroni's correction. Statistical significance was accepted for P values of < 0.05.
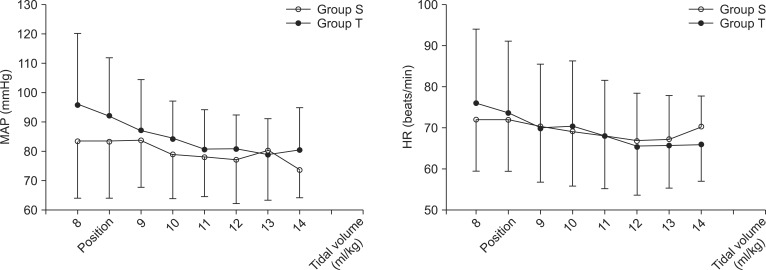
Measurements were obtained in all 40 patients without any hypotensive event (Fig. 1). Patient characteristics showed no significant intergroup difference (Table 1). PIP was significantly higher in Group T than Group S at a TV of 9 ml/kg. PIP was significantly higher for TVs from 11 to14 ml/kg than at baseline value in both groups (P < 0.05) (Fig. 2). EtCO2 was lower than baseline at a TV of 14 ml/kg in group T (37 ± 5 vs. 32 ± 4, P = 0.012) but not in group S (36 ± 6 vs. 32 ± 4, P = 0.153), but no significant intergroup difference was found at any TV level. Furthermore, RIJV CSA was not increased versus baseline by increasing TV in either group and no difference was found between groups (Fig. 2). MAP and HR findings are summarized in Fig. 3. However, no significant changes in MAP or HR were observed on increasing tidal volume from 8 ml/kg to 14 ml/kg in either group.
We conducted this study to determine the optimal TV required to maximizing the CSA of the RIJV to facilitate central venous catheterization in anesthetized patients.
Although US increases the rate of successful RIJV catheterization, it is not always available, and thus, we sought to devise a method for facilitating central catheterization under such circumstances. Our results demonstrate that increases in TV of up to 14 ml/kg are not effective at increasing the CSA of the RIJV. Although PIP was significantly increased by increasing tidal volume, this did not lead to a RIJV CSA increase in either group.
Previous studies have reported that the Trendelenburg position increased RIJV CSA by 15 to 48% in anesthetized adults [9,10]. The disparity between these findings were caused by a greater height difference between the right atrium and the right internal jugular vein, and the promotion of RIJV filling due to reduced return to the superior vena cava [2]. On the other hand, Nassar et al. [11] reported the Trendelenburg position augments RIJV CSA only modestly as compared with the supine position, and found in some patients that it reduced CSA. Thus, it appears that the Trendelenburg position does not predictably increase the IJV CSA. According to our observations, the CSA of the RIJV increased by 6% immediately after adopting the Trendelenburg position and this change was more marked than at other measurement points, although it was not significant (P = 0.695).
The effect of different tidal volume settings is somewhat more complex. In a previous animal study, an increase in TV from 8 ml/kg to 16 ml/kg during hypovolemia was found to increase central venous pressure substantially but not to influence right ventricular end diastolic volume (RVEDV), whereas an increase in PEEP to 15 cmH2O significantly decreased RVEDV [12]. Furthermore, it was observed that only a high PEEP, and not a high TV, significantly changed cardiac filling pressure without hypovolemia. These findings support the observation that applying PEEP can increase RIJV CSA [1,2], but that increases in TV do not, which concurs with our findings. Previous reports have also demonstrated that breath holding at 20 cmH2O [8] or the Valsalva maneuver [13] increase RIJV CSA significantly in the supine and Trendelenburg positions. The two maneuvers are similar in as much as both involve the application of sustained pressure on central venous system. In the present study, US images were obtained at the end-inspiratory phase at each TV, when highest airway pressure was recorded in volume controlled ventilatory cycles only for a short time, which does not apply sustained pressure on the airways or central venous system.
In the present study, MAP and HR were not changed significantly versus baseline when TV was incremented in either group (Fig. 3), which suggests that TVs of < 14 ml/kg do not elevate intrathoracic pressure sufficiently to reduce venous return. Schreiber et al. [14] reported that an increased RIJV CSA in the supine position was further increased immediately after head down tilting. However, no further changes were noted during the following 20 minutes. In the present study, respiratory rate was maintained at 10 breath/min at an I : E ratio of 1 : 2 and TV increases were limited to 14 ml/kg. US images were obtained at the end-inspiratory phase on the 5th respiratory cycle of every TV. It took about 5 minutes for most and did not exceed 20 minutes, and thus, we were able to exclude the effect of time on RIJV CSA.
This study shows that an increase in TV does not increase the CSA of the RIJV within the TV range of 8-14 ml/kg in either the supine or 10° Trendelenburg position. Furthermore, a large TV of 14 ml/kg without inspiratory holding can generate a transient high PIP, but may not effectively compress the SVC and cause RIJV dilation.
References
1. Hollenbeck KJ, Vander Schuur BM, Tulis MR, Mecklenburg BW, Gaconnet CP, Wallace SC, et al. Brief report: effects of positive end-expiratory pressure on internal jugular vein cross-sectional area in anesthetized adults. Anesth Analg. 2010; 110:1669–1673. PMID: 20385614.
2. Marcus HE, Bonkat E, Dagtekin O, Schier R, Petzke F, Wippermann J, et al. The impact of Trendelenburg position and positive end-expiratory pressure on the internal jugular cross-sectional area. Anesth Analg. 2010; 111:432–436. PMID: 20484538.

3. Verghese ST, Nath A, Zenger D, Patel RI, Kaplan RF, Patel KM. The effects of the simulated Valsalva maneuver, liver compression, and/or Trendelenburg position on the cross sectional area of the internal jugular vein in infants and young children. Anesth Analg. 2002; 94:250–254. PMID: 11812678.
4. Suarez T, Baerwald JP, Kraus C. Central venous access: the effects of approach, position, and head rotation on internal jugular vein cross-sectional area. Anesth Analg. 2002; 95:1519–1524. PMID: 12456410.

5. Mesquida J, Kim HK, Pinsky MR. Effect of tidal volume, intrathoracic pressure, and cardiac contractility on variations in pulse pressure, stroke volume, and intrathoracic blood volume. Intensive Care Med. 2011; 37:1672–1679. PMID: 21739340.

6. Smeding L, Plötz FB, Lamberts RR, van der Laarse WJ, Kneyber MC, Groeneveld AB. Mechanical ventilation with high tidal volumes attenuates myocardial dysfunction by decreasing cardiac edema in a rat model of LPS-induced peritonitis. Respir Res. 2012; 13:23. PMID: 22433071.

7. Zhou Q, Xiao W, An E, Zhou H, Yan M. Effects of four different positive airway pressures on right internal jugular vein catheterization. Eur J Anaesthesiol. 2012; 29:223–228. PMID: 22228239.
8. Furukawa H, Fukuda T, Takahashi S, Miyabe M, Toyooka H. Effect of airway pressure and Trendelenburg position on the cross-sectional area of the internal jugular vein in anesthetized patients. Masui. 2004; 53:654–658. PMID: 15242038.
9. Clenaghan S, McLaughlin RE, Martyn C, McGovern S, Bowra J. Relationship between Trendelenburg tilt and internal jugular vein diameter. Emerg Med J. 2005; 22:867–868. PMID: 16299195.

10. Kim JT, Kim HS, Lim YJ, Bahk JH, Lee KH, Kim CS, et al. The influence of passive leg elevation on the cross-sectional area of the internal jugular vein and the subclavian vein in awake adults. Anaesth Intensive Care. 2008; 36:65–68. PMID: 18326134.

11. Nassar B, Deol GR, Ashby A, Collett N, Schmidt GA. Trendelenburg position does not increase cross-sectional area of the internal jugular vein predictably. Chest. 2013; 144:177–182. PMID: 23392444.

12. Oliveira RH, Azevedo LC, Park M, Schettino GP. Influence of ventilatory settings on static and functional haemodynamic parameters during experimental hypovolaemia. Eur J Anaesthesiol. 2009; 26:66–72. PMID: 19122555.

13. Bellazzini MA, Rankin PM, Gangnon RE, Bjoernsen LP. Ultrasound validation of maneuvers to increase internal jugular vein cross-sectional area and decrease compressibility. Am J Emerg Med. 2009; 27:454–459. PMID: 19555617.

14. Schreiber SJ, Lambert UK, Doepp F, Valdueza JM. Effects of prolonged head-down tilt on internal jugular vein cross-sectional area. Br J Anaesth. 2002; 89:769–771. PMID: 12393779.

Fig. 2
Changes in peak inspiratory pressure and cross sectional area of the right internal jugular vein on increasing tidal volume from 8 to 14 ml/kg in 1 ml/kg increments in the supine (Group S; ∘) or Trendelenburg (Group T; •) position. *P < 0.05 vs. Group S, †P < 0.05 vs. baseline value (tidal volume 8 ml/kg). PIP: peak inspiratory pressure, CSA: cross-sectional area.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download