Abstract
Background
Reduction of nasal bone fracture can be performed under general or local anesthesia. The aim of this study was to compare general anesthesia (GA) and monitored anesthetic care (MAC) with dexmedetomidine based on intraoperative vital signs, comfort of patients, surgeons and nurses and the adverse effects after closed reduction of nasal bone fractures.
Methods
Sixty patients with American Society of Anesthesiologists physical status I or II were divided into a GA group (n = 30) or MAC group (n = 30). Standard monitorings were applied. In the GA group, general anesthesia was carried out with propofol-sevoflurane-N2O. In the MAC group, dexmedetomidine and local anesthetics were administered for sedation and analgesia. Intraoperative vital signs, postoperative pain scores by visual analog scale and postoperative nausea and vomiting (PONV) were compared between the groups.
Results
Intraoperatively, systolic blood pressures were significantly higher, and heart rates were lower in the MAC group compared to the GA group. There were no differences between the groups in the patient, nurse and surgeon's satisfaction, postoperative pain scores and incidence of PONV.
Conclusions
MAC with dexmedetomidine resulted in comparable satisfaction in the patients, nurses and surgeons compared to general anesthesia. The incidence of postoperative adverse effects and severity of postoperative pain were also similar between the two groups. Therefore, both anesthetic techniques can be used during the reduction of nasal bone fractures based on a patient%s preference and medical condition.
Reduction of nasal bone fractures has a shorter operating time and less irritation compared to other operations. However, nasal packing is performed after the operation and respiration is maintained only with the mouth; thus, there could be difficulties in maintaining and managing the airway. This operation can be performed under general or local anesthesia. When using general anesthesia, there is the advantage that cooperation from the patient is unnecessary because the airway can be safely maintained along with complete loss of consciousness and analgesic effect. However, local anesthesia is advantageous in that intubation and mechanical ventilation is not necessary, there is less occurrence of sore throat or dry mouth after the operation, and changes in blood pressure from the anesthesia can be minimized. However, anxiety or pain felt by the patient can be problematic, so sedatives or analgesics are additionally used to minimize anxiety or pain. When performing local anesthesia after sedation, respiratory inhibition or inappropriate airway maintenance can occur during the operation because of the administration of sedatives or analgesics, and this could lead to intubation or general anesthesia.
Dexmedetomidine was introduced as a sedative 20 years ago, and has been mainly used in the sedation of intensive care patients who are already intubated. This drug is a highly selective alpha2-adrenoreceptor agonist, and it has the advantage that there is both a sedation and analgesic effect without inhibiting respiration [1-3]. In addition, the half-life is 2 hours which is shorter than other sedatives, and patients can respond to oral commands and return to an aroused state even during sedation; thus, it is convenient in observing the degree of consciousness of the patient [1].
The purpose of this study was to compare monitored anesthetic case (MAC) performed with dexmedetomidine and general anesthesia focusing on postoperative pain and comparing intraoperative vital signs, postoperative nausea and vomiting, the satisfaction of the surgeon, patient and nurse, operation cost, and total operating time.
After obtaining approval from the hospital Institutional Review Board, the advantages and disadvantages of general anesthesia and monitored anesthesia with dexmedetomidine were explained to the patients before surgery. After obtaining written consent, the patients selected their preferred method of anesthesia.
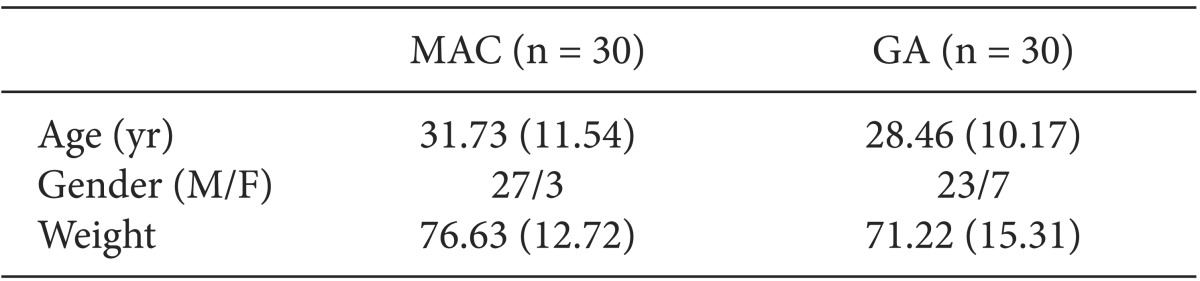
The subjects consisted of patients with American Society of Anesthesiologists physical status (ASA PS) class 1 or 2 and between 20 to 40 years of age scheduled for reduction of nasal fractures, and 30 patients each were included in the general anesthesia and monitored anesthesia group. Patients under 20 or over 40 years of age, patients who used sedatives or analgesics within 24 hours before the operation, patients with psychological or neurological diseases, and patients with uncontrollable hypertension or other heart diseases were excluded.
There was no premedication for both groups. After arriving in the operating room, basic monitoring equipment such as electrocardiogram, peripheral artery oxygen saturation (SaO2), and noninvasive blood pressure were attached, and hemodynamics were measured in 5 minute intervals. Then, 5 L/min of oxygen was administered into the oral cavity of the MAC group using an oxygen cannula. The bispectral index (BIS) was measured, and local anesthesia was performed through nasal packing with 10% Xylocaine gauze for 10 minutes until immediately before the operation. Dexmedetomidine was administered at a loading dose of 1 ug/kg for 10 minutes, and then injected in dosages of 0.3-1 ug/kg/hr. Intraoperative BIS was maintained at 60-80, and remifentanil 0.4 ug/kg was administered 30 seconds before performing closed reduction. When intraoperative oxygen saturation fell below 95%, spontaneous respiration was induced according to the request of the anesthesiologist.
In the general anesthesia (GA) group, propofol 2 mg/kg and rocuronium 0.6 mg/kg was IV injected to induce anesthesia and then intubation was performed. Anesthesia was maintained with 1.2-2.4% sevoflurane and 50% N2O 50% O2 at a fresh gas flow of 4 L/min. Remifentanil 0.4 ug/kg was administered 30 seconds before performing the closed reduction. After the operation, glycopyrrolate 0.005 mg/kg and pyridostigmine 0.2 mg/kg were used to reverse any remaining muscle relaxation.
The time from the start of anesthesia to the end of the anesthesia was recorded for both groups.
In the recovery room, the satisfaction of the patients was measured (scale of 1-5: 1 very bad, 2 bad, 3 normal, 4 good, 5 very good) and the visual analogue scale (0-100 mm visual analog scale [VAS]) was used to measure the pain of the operated area. Additionally, 8 hours after surgery, the satisfaction of the operating surgeon and ward nurse (scale of 1-5: 1 very bad, 2 bad, 3 normal, 4 good, 5 very good) was measured.
Fentanyl 1 µg/kg was administered when pain management was required in the recovery room after surgery. In addition, from the start of the surgery to leaving the recovery room, the occurrence of an infrequent pulse (pulse rate < 60 bpm), systolic blood pressure < 80 mmHg, sore throat or dry mouth were recorded. Additionally, lower than SaO2 90% and lower than 95% were recorded separately.
The vital signs were recorded at the following times: 5 minutes after arriving at operating room (T0, baseline), after intubation of the subjects in the GA group (T1), 5 minutes after starting the administration of loading dose of dexmedetomidine for MAC group (T1), 5 minutes after T1 (T2), 10 minutes after T1 (T3), immediately after closed reduction (T4), and 30 minutes after entering the recovery room (T5).
All results are expressed as the mean (standard deviation). The Student t-test or Mann-Whitney U-test was used to test for differences in demographics, satisfaction, pain score in the recovery room, anesthesia cost and operating/anesthesia time between the two groups. Chi-square test was used to compare the two groups in terms of the frequency of postoperative adverse side effect occurrence, and repeated measures ANOVA and multiple comparative test with Bonferroni's corrections were performed to compare the hemodynamic changes in each group. GraphPad Prism for Windows (version 6.00, GraphPad Software, La Jolla, San Diego, CA, USA, www.graphpad.com) was used for statistical analysis, and findings were considered significant when P < 0.05.
In a study by Sener et al. [4], the pain score of the control group was 40.9 ± 20.1 mm; thus, the pain score of the GA group was set at 40 mm in this study, and it was presumed to be statistically significant if the VAS of the MAC group decreased by 15 mm (37.5%) after the operation. Here, the standard deviation was presumed to be 20 mm. When the primary error was set at 0.05 and the power at 0.80 for both tests, approximately 30 patients were needed for each group to confirm that there was a 15-mm difference in VAS.
From a total of 60 operations, 30 were in the MAC group and 30 in the GA group. There were no significant differences in age, sex, and weight between the two groups (Table 1). There were no significant differences in overall satisfaction of the patient, operating surgeon, and ward nurse between the two groups, and there were also no significant differences in the occurrence of adverse side effects such as postoperative sore throat, dry mouth, nausea, and vomiting (Table 2). The pain score of the operating room and the recovery room were also no significant difference between in the two groups (GA group: 24.66 (17.75); MAC group: 28.84 (18.38), P = 0.13).
In the MAC group, desaturation (SaO2 < 95%) occurred in two patients (6%); however, hypoxemia of SaO2 lower than 90% did not occur.
Regarding intraoperative vital signs, the MAC group had a higher pulse rate and lower blood pressure overall compared to the GA group. The MAC group had a significantly higher pulse rate compared to the GA group from T1 to T4 (P < 0.01, P < 0.01, P < 0.01, P < 0.01) and a significantly lower mean blood pressure, diastolic blood pressure and systolic blood pressure at T2 and T3 (P = 0.01, P = 0.02), at T2 (P = 0.01) and at T2, T3 and T4 (P < 0.01, P < 0.01, P = 0.03) (Fig. 1), respectively.
Regarding change in blood pressure according to time, the GA group had significant differences in measurements at T2, T3, and T4 compared to baseline (T0) for systolic blood pressure, diastolic blood pressure, and mean blood pressure, while the MAC group did not show any significant differences. Both groups showed significant change in pulse rate. Compared to baseline, the pulse rate of the GA group significantly increased while that of the MAC group significantly decreased (Fig. 1).
There was no significant difference between the two groups in total anesthesia time (GA group: 37.91 [11.03] min; MAC group: 31.60 [6.87] min, P = 0.37).
Regarding anesthesia cost, the GA group was charged a total of 300,950 KRW, in which the general anesthesia cost was 73,940 KRW, the airway instrument for airway maintenance such as the airway circuit (MEGA Ace Kit® Ace medical, Seoul, Korea) and endotracheal tube (Mallinckrodt™, Covidien, Dublin, Ireland) were 201,100 KRW, and other drug costs were 25,910 KRW. The MAC group was charged a total of 64,890 KRW, in which the anesthesia cost was 29,690 KRW, and other drug costs including the dexmedetomidine (Hospira, Lake Forest, IL, USA) were 35,200 KRW; thus, the total cost for anesthesia was cheaper in the MAC group.
Dexmedetomidine can control the degree of sedation according to the dosage while minimizing respiratory inhibition, and also has an analgesic effect by suppressing the sympathetic nerve system; therefore, it has recently been used as anesthesia or an anesthesia supplement in various procedures [5-8].
In previous studies which performed sedation with dexmedetomidine, the sedative effect necessary for procedure was maintained while there was no occurrence of respiratory inhibition such as reduced oxygen saturation, increased end-tidal CO2, or decrease in respiration rate to the end of the procedure [7-9]. In this study also, when the sedated state of BIS 60-80 was induced during the operation with dexmedetomidine, there was no occurrence of cases in which SaO2 decreased to 90% or lower. Six percent of the cases showed a SaO2 reduction of 95% or lower, and when this occurred, deep breathing was performed around 4 times according to the orders of the anesthesiologist then an oxygen saturation of 100% was accomplished, immediately. In the recovery room after the operation, there were no occurrences of reduced oxygen saturation or other respiratory complications, and this was the same in the GA group. However, this study was performed on healthy ASA PS 1 and 2 patients with no underlying respiratory diseases. When performing general anesthesia in elderly or in patients with underlying respiratory diseases, intubation and maintaining machine respiration could be factors that increase the occurrence of respiratory complications after operation. oxygen saturation of 100% was accomplished, immediately. In the recovery room after the operation, there were no occurrences of reduced oxygen saturation or other respiratory complications, and this was the same in the GA group. However, this study was performed on healthy ASA PS 1 and 2 patients with no underlying respiratory diseases. When performing general anesthesia in elderly or in patients with underlying respiratory diseases, intubation and maintaining machine respiration could be factors that increase the occurrence of respiratory complications after operation.
Goksu et al. [7] reported that there was a sufficient analgesic effect when dexmedetomidine was used for intraoperative anesthesia. In addition, in other studies, the pain score of patients was significantly lower when dexmedetomidine was used compared to the general anesthesia group or the group with no anesthesia, and this confirms that dexmedetomidine has an analgesic effect [8,10]. In our study, the pain score of the MAC group measured in the recovery room was 28.84 mm showing no significant difference with the GA group (VAS = 24.66 mm) (P = 0.13). Precedent studies generally defined pain as being properly managed when the pain score is 30 mm or lower [7,8,10], and in our study, the mean pain score of both groups was well inside this range. We believe this is because the closed reduction of the nasal bone performed in this study is a relatively non-invasive procedure, and the pain from the operation is not great. Reasons for this are from differences in the operating surgeon, and in the type and method of the surgery.
Dogan et al. [8] reported that the satisfaction of patients was higher in local anesthesia using dexmedetomidine compared to general anesthesia. In our research, there was no difference between groups in satisfaction scores, and the patients were generally satisfied. This is thought to be because the patients chose their preferred method of anesthesia before the operation in this study.
Ríha et al. [11] divided patients undergoing coronary artery bypass into a group that used dexmedetomidine and ketamine and a group that used sevoflurane and sufentanil, and results of measuring CKMB and troponin I after surgery showed that the group that underwent anesthesia using dexmedetomidine and ketamine had significantly lower figures. Roekaerts et al. [12] also reported that in a dog with induced coronary artery stenosis after general anesthesia, the blood flow increased to the ischemic heart muscle and the oxygen requirement of the entire heart muscle decreased after injecting dexmedetomidine. Our study also showed that the MAC group maintained a lower pulse rate and a more stable blood pressure than that of the GA group; thus, when performing closed reduction of nasal bone in patients with underlying cardiovascular diseases, a better prognosis is anticipated with MAC using dexmedetomidine than with general anesthesia [13,14].
Regarding total anesthesia time, the MAC group did not need time for endotracheal intubation, extubation, and awakening so the required time was anticipated to be shorter, but in fact, there was no significant difference between the two groups. This is thought to be because of the time required for the dosage and control until the patient is sedated, and an appropriate BIS (60-80) was maintained when performing MAC.
In general anesthesia, postoperative nausea and vomiting can occur as a side effect of endotracheal intubation or inhalation anesthetic, and also in a study by Fedok et al. [15], the percentage of postoperative nausea and vomiting was significantly lower when local anesthesia was performed compared to general anesthesia. However, in our research, there was no significant difference in the percentage of postoperative nausea and vomiting between the two groups. This is believed to be attributed to the short operation and anesthesia time because the intubation time was shorter and a reduced amount of inhalation anesthesia was used [16,17].
In our study, each anesthesia method was safely performed without any serious complications during or after operation, and there were no differences in the occurrence of nausea, vomiting, sore throat, and thirstiness, or in terms of patient satisfaction. Therefore, in the anesthesia of patients without any particular underlying diseases, it is advisable to select and perform an anesthesia method according to the preference of the patient. However, in terms of hemodynamics, the MAC group was more stably maintained, and together with the advantage that machine respiration is not required, MAC can be the preferred choice of anesthesia for patients who are not systemically healthy. As can be seen from the results, MAC provided sufficient medical treatment to the patient at a reduced cost. However, despite these various advantages of MAC, the medical insurance subsidies for this procedure are not sufficient under the current medical insurance system; therefore, adequate measures and reasonable medical insurance subsidies are required.
This study compared monitored anesthesia using dexmedetomidine and local anesthetic and general anesthesia with sevoflurane and N2O for nasal fractures. Both anesthesia methods were safely performed without the occurrence of any serious complications during and after the operation, and there were no differences in the occurrence of nausea, vomiting, sore throat or thirstiness in the recovery room, and in terms of satisfaction of the patients. Therefore, monitored anesthesia using dexmedetomidine is considered to be a good alternative when patients undergoing short-term or small operations such as nasal fracture correction do not prefer general anesthesia.
References
1. Hall JE, Uhrich TD, Barney JA, Arain SA, Ebert TJ. Sedative, amnestic, and analgesic properties of small-dose dexmedetomidine infusions. Anesth Analg. 2000; 90:699–705. PMID: 10702460.

2. Gerlach AT, Dasta JF. Dexmedetomidine: an updated review. Ann Pharmacother. 2007; 41:245–252. PMID: 17299013.

3. Ebert TJ, Hall JE, Barney JA, Uhrich TD, Colinco MD. The effects of increasing plasma concentrations of dexmedetomidine in humans. Anesthesiology. 2000; 93:382–394. PMID: 10910487.

4. Sener M, Yilmazer C, Yilmaz I, Bozdogan N, Ozer C, Donmez A, et al. Efficacy of lornoxicam for acute postoperative pain relief after septoplasty: a comparison with diclofenac, ketoprofen, and dipyrone. J Clin Anesth. 2008; 20:103–108. PMID: 18410864.

5. Aydil U, Yilmaz M, Akyildiz I, Bayazit Y, Keseroglu K, Ceylan A. Pain and safety in otorhinolaryngologic procedures under local anesthesia. J Otolaryngol Head Neck Surg. 2008; 37:851–855. PMID: 19128715.
6. Hytönen M, Blomgren K, Lilja M, Mäkitie AA. How we do it: septoplasties under local anaesthetic are suitable for short stay surgery; the clinical outcomes. Clin Otolaryngol. 2006; 31:64–68. PMID: 16441807.

7. Goksu S, Arik H, Demiryurek S, Mumbuc S, Oner U, Demiryurek AT. Effects of dexmedetomidine infusion in patients undergoing functional endoscopic sinus surgery under local anaesthesia. Eur J Anaesthesiol. 2008; 25:22–28. PMID: 17666131.

8. Dogan R, Erbek S, Gonencer HH, Erbek HS, Isbilen C, Arslan G. Comparison of local anaesthesia with dexmedetomidine sedation and general anaesthesia during septoplasty. Eur J Anaesthesiol. 2010; 27:960–964. PMID: 20498606.

9. Venn RM, Hell J, Grounds RM. Respiratory effects of dexmedetomidine in the surgical patient requiring intensive care. Crit Care. 2000; 4:302–308. PMID: 11056756.
10. Candiotti KA, Bergese SD, Bokesch PM, Feldman MA, Wisemandle W, Bekker AY. Monitored anesthesia care with dexmedetomidine: a prospective, randomized, double-blind, multicenter trial. Anesth Analg. 2010; 110:47–56. PMID: 19713256.

11. Ríha H, Kotulák T, Březina A, Hess L, Kramář P, Szárszoi O, et al. Comparison of the effects of ketamine-dexmedetomidine and sevoflurane-sufentanil anesthesia on cardiac biomarkers after cardiac surgery: an observational study. Physiol Res. 2012; 61:63–72. PMID: 22188112.

12. Roekaerts PM, Prinzen FW, De Lange S. Beneficial effects of dexmedetomidine on ischemic myocardium of anaesthetized dogs. Br J Anaesth. 1996; 77:427–429. PMID: 8949826.
13. Reich DL, Bennett-Guerrero E, Bodian CA, Hossain S, Winfree W, Krol M. Intraoperative tachycardia and hypertension are independently associated with adverse outcome in noncardiac surgery of long duration. Anesth Analg. 2002; 95:273–277. PMID: 12145033.

14. Wijeysundera DN, Naik JS, Beattie WS. Alpha-2 adrenergic agonists to prevent perioperative cardiovascular complications: a meta analysis. Am J Med. 2003; 114:742–752. PMID: 12829201.
15. Fedok FG, Ferraro RE, Kingsley CP, Fornadley JA. Operative times, postanesthesia recovery times, and complications during sinonasal surgery using general anesthesia and local anesthesia with sedation. Otolaryngol Head Neck Surg. 2000; 122:560–566. PMID: 10740178.

16. Lee DW, Lee HG, Jeong CY, Jeong SW, Lee SH. Postoperative nausea and vomiting after mastoidectomy with tympanoplasty: a comparison between TIVA with propofol-remifentanil and balanced anesthesia with sevoflurane-remifentanil. Korean J Anesthesiol. 2011; 61:399–404. PMID: 22148089.

17. Apfel CC, Kranke P, Katz MH, Goepfert C, Papenfuss T, Rauch S, et al. Volatile anaesthetics may be the main cause of early but not delayed postoperative vomiting: a randomized controlled trial of factorial design. Br J Anaesth. 2002; 88:659–668. PMID: 12067003.
Fig. 1
Changes in hemodynamic variables. GA: general anesthesia, MAC: monitored anesthetic care with dexmedetomidine. T0: baseline, T1: after intubation in the GA group or 5 min after dexmedetomidine infusion in the MAC group, T2 and T3: 5 and 10 min after T1, T4: after closed reduction. *P < 0.05 between MAC group and GA group. †Within group difference compared to baseline (T0) value.
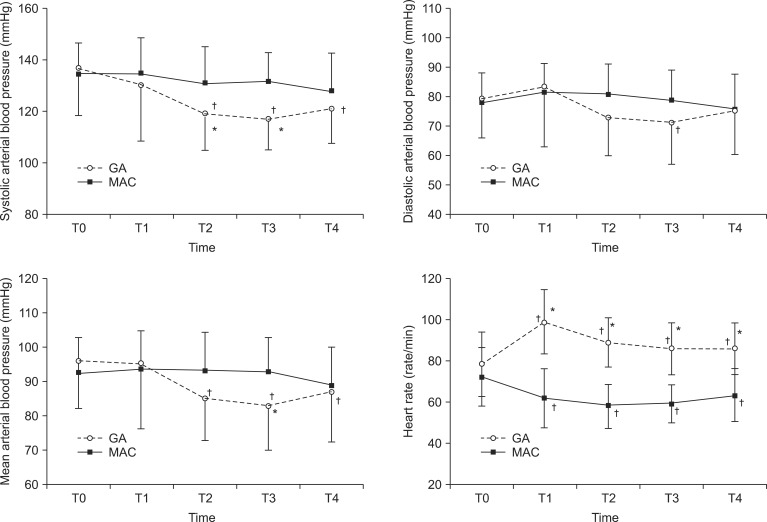
Table 2
Complications and Pain at PACU and Satisfaction of the Patients, Surgeon and Nurse at Day 1 after the Surgery
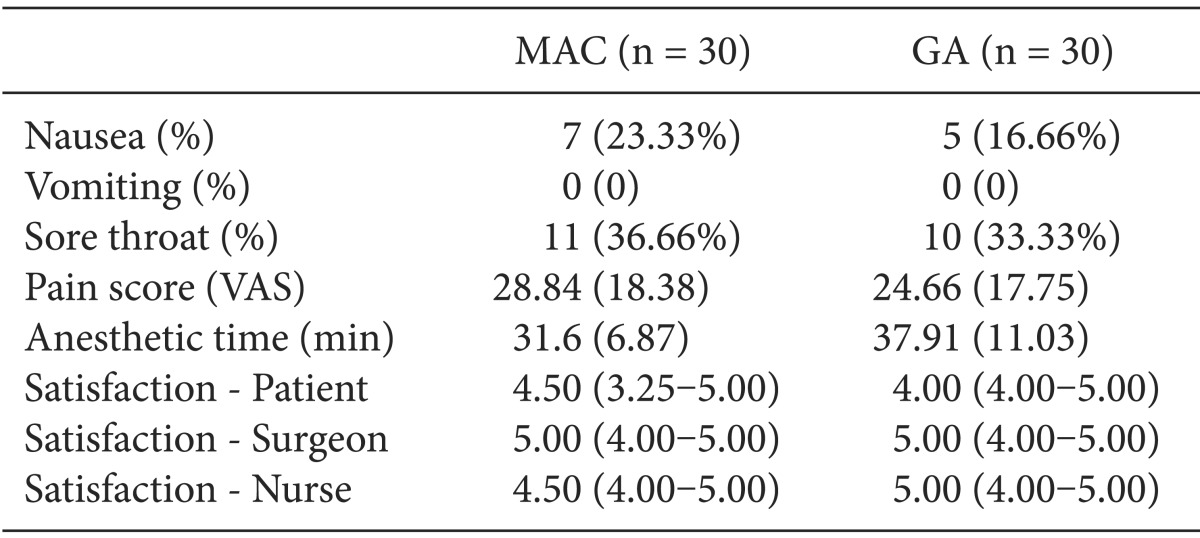
All data are expressed as the mean (SD) except for satisfaction. Data for satisfaction are expressed as the median (interquantile range). VAS: 100 mm visual analogue scale, PACU: postanesthetic care unit, MAC: monitored anesthetic care with dexmedetomidine, GA: general anesthesia, Anesthetic time: total anesthesia time, Satisfaction: 1: very poor, 2: poor, 3: moderate, 4: good, 5: very good.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download