Abstract
Background
Active upper respiratory tract infection (URI), orotracheal intubation and use of inhalation anesthetics are known risk factors for perioperative respiratory adverse events (RAE). This study investigated the risk factors of perioperative RAE in children with these risk factors.
Methods
The records of 159 children who underwent general anesthesia with an orotracheal tube and inhalation were reviewed. These patients also had at least one of the following URI symptoms on the day of surgery: clear or green nasal secretion, dry or moist cough, nasal congestion, or fever. RAE such as laryngospasm, bronchospasm, oxygen desaturation and sustained cough were collected before induction, during intubation, during extubation, after extubation and in the postanesthesia care unit.
Results
Forty-five patients had RAE. The patients with RAE were younger than those without RAE. There were more passive smokers and a greater number of intubation attempts in patients with RAE than in those without RAE. The type of surgery and type of inhalation agents were not different between patients with and without RAE. Passive smoking was the only independent risk factor for RAE.
Respiratory adverse events (RAE) are the most common perioperative critical events in pediatric patients [1,2]. Several studies have been performed to identify risk factors for RAE in children [3-7]. Active upper respiratory tract infection (URI) is an independent risk factor for perioperative RAE [3-7]. While most of these studies have described the association between active or recent URI and RAE, only one study has demonstrated the risk factors of RAE in children with an active URI [6]. One of independent risk factors for RAE in children with an active URI is a use of an endotracheal tube [6]. Meanwhile, an orotracheal tube and maintenance of anesthesia with inhalation agents are known risk factors for perioperative RAE [4,6,7] regardless of the presence of URI.
About 30% of children presenting for elective surgery have an active URI [4,6]. URI is the most common reason for cancellations in pediatric patients [8]. However, cancellation of surgery can have emotional and economic impacts on families of pediatric patients [8]. Therefore, most cases proceed after the parents are warned of the risk. In addition, the previous studies demonstrated that even though an active URI increases the risk of RAE, most children with an active URI undergo the elective procedure safely and without increased morbidity [6,9,10].
Therefore, this study retrospectively evaluated the incidence and risk factors of RAE in pediatric patients who already have known risk factors such as active URI, orotracheal intubation and use of inhalation agents.
After gaining approval from the Institutional Review Board (4-2011-0184), the electronic medical records of 159 pediatric patients who underwent surgery at the Eye and ENT Center of our university hospital from June 2010 to July 2011 were retrospectively reviewed. One hundred twenty one patients received eye surgery, 28 patients received tonsillectomy and adenoidectomy and 10 patients received ear surgey. The selected patients also had at least one of the following symptoms on the day of surgery: clear or green nasal secretion, dry or moist cough, nasal congestion, or fever (≥ 38℃) [3-7,11]. Parents of the patients were interviewed by anesthesiologist to determine if the patient had any symptoms or potential factors for perioperative RAE (asthma medication within one year, nocturnal dry cough persisting more than two weeks in the past year, history of allergies, atopy and allergic rhinitis, and passive smoking) [7,12]. These symptoms and risk factors were then described in the anesthesia record. For patients with an active URI, lung sounds were assessed before anesthesia.
Upon arrival in the operating room, standard monitoring devices were applied. General anesthesia was induced with intravenous propofol (2-3 mg/kg). Orotracheal intubation was performed after administration of fentanyl (1 µg/kg) and rocuronium bromide 0.3 mg/kg. Anesthesia was maintained with sevoflurane or desflurane in 50% O2/air. Extubation was performed when the patient was awake or in a state of deep anesthesia.
Preoperative data (age, gender, body mass index, and American Society of Anesthesiologists class), intraoperative data (type of anesthetic induction, number of intubation attempts, type of inhalation agents, timing of extubation, type of surgery, duration of surgery, and duration of anesthesia) and postoperative data (length of stay in the postanesthesia care unit [PACU]) were collected. RAE such as laryngospasm, bronchospasm, oxygen desaturation (SpO2 < 95%) and sustained cough (> 5 sec) [3-7,12] were collected during perioperative periods (before induction, during intubation, during extubation, after extubation, and PACU). These events were described in the anesthetic or PACU records.
Statistical analysis was performed using PASW Statistics 18® (SPSS Inc., Chicago, IL, USA) and SAS software 9.1.3 (SAS Inc., Cary, NC, USA). Categorical variables were evaluated by χ2 test or Fisher's exact test as appropriate. A logistic regression model was used to identify independent risk factors of perioperative RAE. Factors shown to be associated with RAE on univariate analysis (P values < 0.2) were entered into a multivariate logistic regression model to identify independent risk factors. All values were expressed as mean ± SD or the number of patients (percentage). A P value < 0.05 was considered statistically significant.
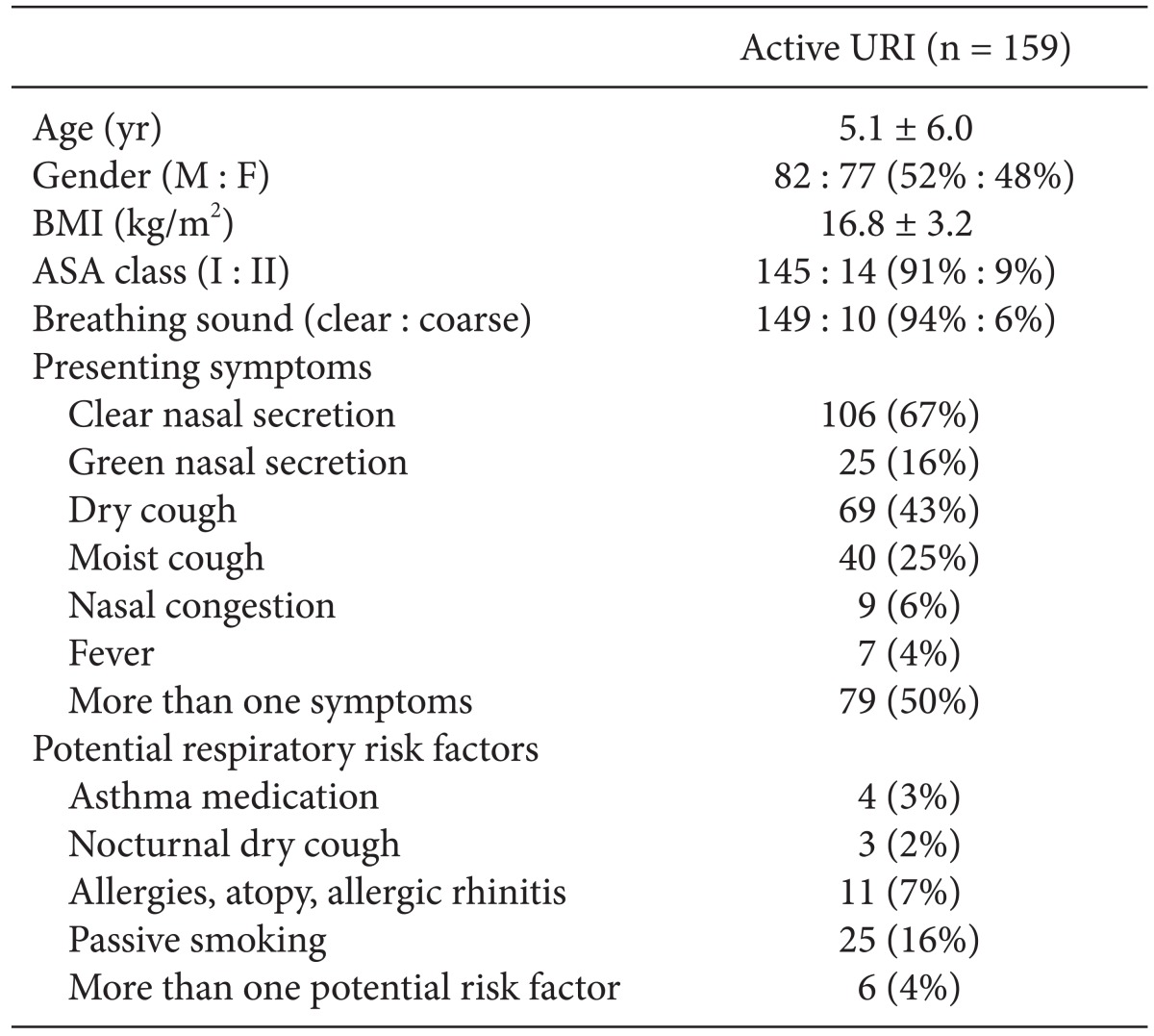
The preoperative characteristics of patients with an active URI are shown in Table 1. The mean age of these patients was 5.1 yr old and the minimum and maximum ages were 9 months old and 12 yr old, respectively. Clear nasal secretion was the most common URI symptom. Seventy nine (50%) patients presented with more than one symptom. Forty-nine (31%) patients had potential respiratory risk factors. Passive smoking was the most common risk factor. Six patients had more than one potential respiratory risk factor.
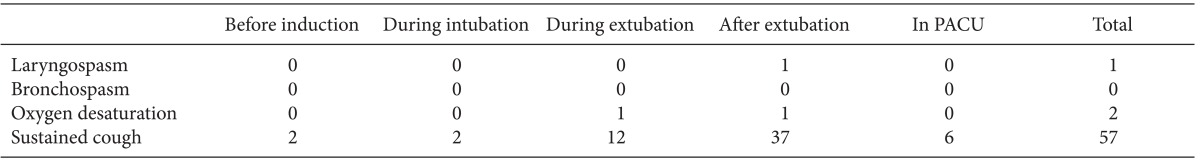
Forty five (28%) patients had RAE during perioperative periods. Table 2 shows details of RAE. One patient had a laryngospasm and two patients experienced oxygen desaturation, while others had a sustained cough. One patient had both oxygen desaturation and a sustained cough. Some patients had a sustained cough at several points during the follow-up period. RAE tended to occur mainly after extubation. All cases of RAE were mild and easily managed without any drug treatment. Laryngospasm was recovered 100% oxygen and positive pressure ventilation and oxygen desaturation was recovered by jaw thrust and mask ventilation. The length of stay in the PACU was similar in patients with and without RAE (34.3 ± 9.8 min versus 33.1 ± 7.7 min, respectively).
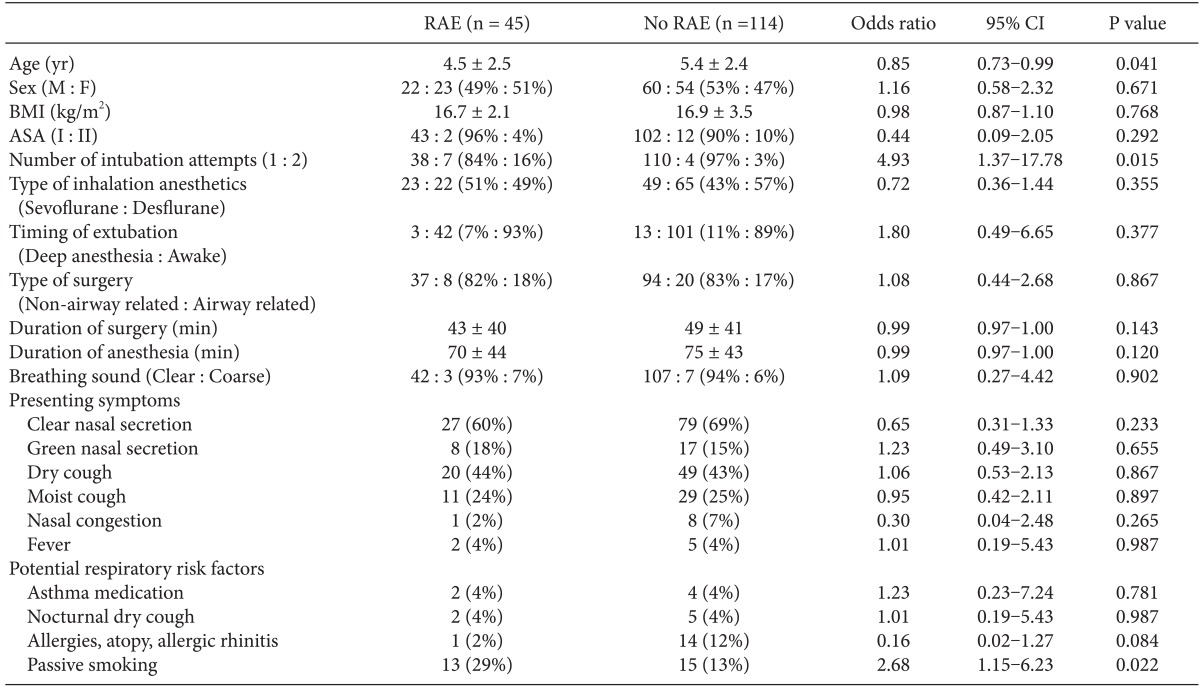
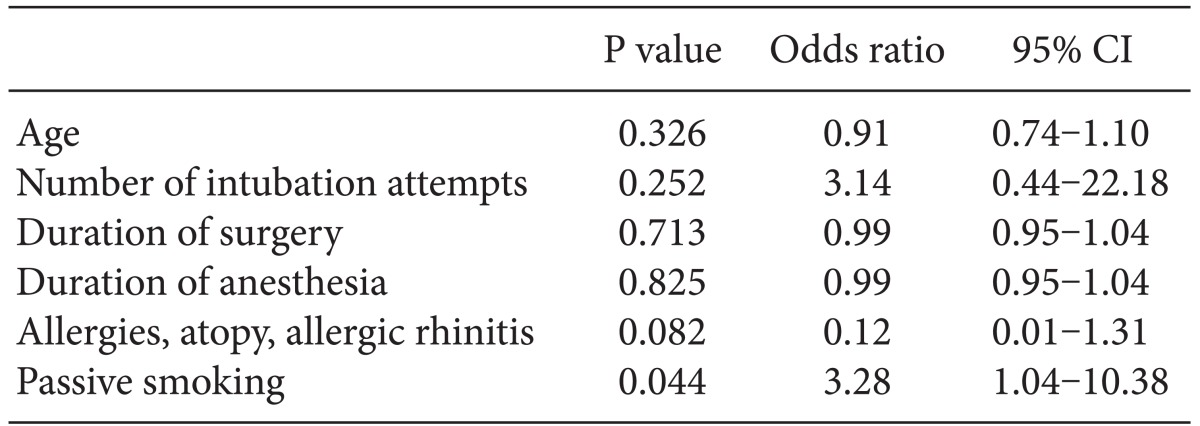
Univariate analysis was performed to identify patient characteristics associated with RAE (Table 3). The patients with RAE were younger than those without RAE (4.5 ± 2.5 yr vs. 5.4 ± 2.4 yr, respectively, P = 0.041). Patients with RAE had a greater number of intubation attempts and were more likely to be passive smokers than patients without RAE. The type of inhalation agents and type of surgery were not significantly different between patients with and without RAE. Multivariate analysis was performed to identify independent risk factors of RAE (Table 4). Passive smoking was the only independent risk factor of RAE.
This study reviewed the perioperative RAE of pediatric patients with an active URI who underwent general anesthesia with an endotracheal tube and inhalation agents. Approximately 25% of the patients experienced perioperative RAE. The most common RAE was a sustained cough and none of the RAE was associated with adverse sequelae. Patients who experienced RAE had a younger mean age, greater number of intubation attempts and were more likely to be passive smokers than patients without RAE. Passive smoking was an independent risk factor for RAE.
Since children suffer an average of six colds per year [13], it is common for an anesthesiologist to meet children with URI. URI is a well-known risk factor for perioperative RAE [3-7]. Although URI is the most common reason for cancellation of surgery in pediatric patients [8], the issue of whether to proceed or postpone the procedure and how long to postpone it has been a source of debate for many years. Several studies demonstrated that most RAE in children with an active URI were manageable and an active URI was not associated with an increase in morbidity [6,9,10]. In the current study, even though one case of laryngospasm and two cases of oxygen desaturation occurred, these complications were properly managed and not related to long-term sequelae. Considering these results, most patients with an active URI could proceed to surgery since cancellation on the day of surgery can have an emotional and economic impact on the families of pediatric patients [8].
Patients with RAE were significantly younger than those without RAE (4.5 ± 2.5 yr vs. 5.4 ± 2.4 yr, respectively) (Table 3). Young age is a well-known risk factor for RAE in children with or without a URI [3,5-7,12]. Previous studies reported that the mean age of patients with RAE was 4.95 ± 4.67 yr, which is similar to results of the current study [7]. The number of intubation attempts has been previously associated with RAE [3,7]. The results of current study are similar to those of previous studies in that patients with RAE had a greater number of intubation attempts than patients without RAE (Table 3).
Multivariate logistic regression analysis indicated that passive smoking is the only independent risk factor of RAE (Table 4). This finding is supported by previous results [4,6,7]. Passive smoking is associated with an increased incidence and severity of asthma and airway hyper-reactivity [14-16]. It is also linked with upper airway cellular and mucociliary dysfunction [17]. In the current study, six patients took asthma medication and two of them were passive smokers. These two patients had RAE. One patient experienced oxygen desaturation after extubation and the other patient had a sustained cough during and after extubation and in the PACU.
Even though some studies have shown that surgery involving the airway is an independent risk factor for RAE [6,7,12], the incidence of RAE was not higher in airway related surgery in the current study. In accordance with previous results [5], extubation in an awake state or under deep anesthesia was not related to RAE (Table 3).
While some studies have demonstrated that copious nasal secretion and congestion are independent risk factors for RAE [4,6], another study showed no association between any particular symptoms and the rate of RAE [5]. In the current study, six symptoms - clear or green nasal discharge, dry or moist cough, nasal congestion, or fever (≥ 38℃) - were evaluated and there were no significant relationships between any individual symptom and perioperative RAE (Table 3). Seventy-nine patients (49.7%) patients had more than one symptom. The incidence of RAE was not different between the patients with one symptom and those with more than one symptom (26.2% vs 30.4%, P = 0.563)
Most cases of RAE occurred after extubation (Table 2). One case of laryngospasm also occurred after extubation in 2 yrs and 2 months old male patients undergoing eye surgery. It was reported that laryngospasm tend to occur mainly after extubation [18]. The incidence of laryngospasm is 0.78-5% depending on surgical type, age, pre-existing conditions, and anesthetic technique [19]. In the previous studies with children, the incidences of laryngospam are 1.4 to 4.2% [3,6,7,12]. The independent risk factors for laryngospasm in children are known as male gender, presence of URI, airway anomaly and congenital heart disease [20]. In the current study, the incidence of laryngospasm was 0.63%. There may be several reasons for the lower incidence of laryngospasm in this study even though all patients had active URI. First, none of the patients was less than 3 months old which increases the incidence of laryngospasm [19]. Second, we only included patients with an endotracheal tube. While some studies demonstrated that endotracheal tube increased RAE when compared with laryngeal mask airway (LMA) [4,21], other studies showed that LMA increased RAE when compared with endotracheal tube [11,20]. Therefore, the incidence of laryngospasm in previous studies [3,6,7,12] including both endotracheal tube and LMA could be different that of this study. Lastly, all cases in this study were performed during day time and none of cases was an emergency. Therefore, the extubation was performed by a staff or senior resident who had an experience of pediatric anesthesia. Indeed, the incidence of RAE is dependent on the experience of an anesthesiologist [7,12].
There are some limitations in this study. One is that the data were collected retrospectively and there is possibility that some of data were not recorded in the anesthesia record. The other limitation is that even though we selected patients who had at least one of the symptoms of clear or green nasal secretion, dry or moist cough, nasal congestion, or fever (≥ 38℃) according to the previous studies [3-7,11], these symptoms are not specific for URI. Therefore it is possible that the patients who didn't have URI could alter results.
In conclusion, passive smoking is the independent risk factor for RAE in children with a URI who underwent general anesthesia with an endotracheal tube and inhalation agents. Most pediatric patients with a URI can proceed with surgery without severe complications.
Acknowledgments
The authors thanks to biostatisticians in the Department of Research Affairs, Yonsei University College of Medicine, for statistical comments and analysis.
References
1. Tay CL, Tan GM, Ng SB. Critical incidents in paediatric anaesthesia: an audit of 10000 anaesthetics in Singapore. Paediatr Anaesth. 2001; 11:711–718. PMID: 11696149.
2. Tiret L, Nivoche Y, Hatton F, Desmonts JM, Vourc'h G. Complications related to anaesthesia in infants and children. A prospective survey of 40240 anaesthetics. Br J Anaesth. 1988; 61:263–269. PMID: 3179147.
3. Bordet F, Allaouchiche B, Lansiaux S, Combet S, Pouyau A, Taylor P, et al. Risk factors for airway complications during general anaesthesia in paediatric patients. Paediatr Anaesth. 2002; 12:762–769. PMID: 12519134.

4. Parnis SJ, Barker DS, Van Der Walt JH. Clinical predictors of anaesthetic complications in children with respiratory tract infections. Paediatr Anaesth. 2001; 11:29–40. PMID: 11123728.

5. Rachel Homer J, Elwood T, Peterson D, Rampersad S. Risk factors for adverse events in children with colds emerging from anesthesia: a logistic regression. Paediatr Anaesth. 2007; 17:154–161. PMID: 17238887.

6. Tait AR, Malviya S, Voepel-Lewis T, Munro HM, Seiwert M, Pandit UA. Risk factors for perioperative adverse respiratory events in children with upper respiratory tract infections. Anesthesiology. 2001; 95:299–306. PMID: 11506098.

7. von Ungern-Sternberg BS, Boda K, Chambers NA, Rebmann C, Johnson C, Sly PD, et al. Risk assessment for respiratory complications in paediatric anaesthesia: a prospective cohort study. Lancet. 2010; 376:773–783. PMID: 20816545.

8. Tait AR, Voepel-Lewis T, Munro HM, Gutstein HB, Reynolds PI. Cancellation of pediatric outpatient surgery: economic and emotional implications for patients and their families. J Clin Anesth. 1997; 9:213–219. PMID: 9172029.

9. Tait AR, Knight PR. The effects of general anesthesia on upper respiratory tract infections in children. Anesthesiology. 1987; 67:930–935. PMID: 3688537.

10. Elwood T, Morris W, Martin LD, Nespeca MK, Wilson DA, Fleisher LA, et al. Bronchodilator premedication does not decrease respiratory adverse events in pediatric general anesthesia. Can J Anaesth. 2003; 50:277–284. PMID: 12620952.

11. von Ungern-Sternberg BS, Boda K, Schwab C, Sims C, Johnson C, Habre W. Laryngeal mask airway is associated with an increased incidence of adverse respiratory events in children with recent upper respiratory tract infections. Anesthesiology. 2007; 107:714–719. PMID: 18073545.

12. Mamie C, Habre W, Delhumeau C, Argiroffo CB, Morabia A. Incidence and risk factors of perioperative respiratory adverse events in children undergoing elective surgery. Paediatr Anaesth. 2004; 14:218–224. PMID: 14996260.

13. Monto AS, Ullman BM. Acute respiratory illness in an American community. The Tecumseh study. JAMA. 1974; 227:164–169. PMID: 4357298.

14. Chilmonczyk BA, Salmun LM, Megathlin KN, Neveux LM, Palomaki GE, Knight GJ, et al. Association between exposure to environmental tobacco smoke and exacerbations of asthma in children. N Engl J Med. 1993; 328:1665–1669. PMID: 8487825.

15. Murray AB, Morrison BJ. The effect of cigarette smoke from the mother on bronchial responsiveness and severity of symptoms in children with asthma. J Allergy Clin Immunol. 1986; 77:575–581. PMID: 3958385.

16. Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ. The Group Health Medical Associates. Asthma and wheezing in the first six years of life. N Engl J Med. 1995; 332:133–138. PMID: 7800004.

17. Richardson MA. Upper airway complications of cigarette smoking. J Allergy Clin Immunol. 1988; 81:1032–1035. PMID: 3286730.

18. Visvanathan T, Kluger MT, Webb RK, Westhorpe RN. Crisis management during anaesthesia: laryngospasm. Qual Saf Health Care. 2005; 14:e3. PMID: 15933300.

19. Olsson GL, Hallen B. Laryngospasm during anaesthesia. A computer-aided incidence study in 136,929 patients. Acta Anaesthesiol Scand. 1984; 28:567–575. PMID: 6496018.
20. Flick RP, Wilder RT, Pieper SF, van Koeverden K, Ellison KM, Marienau ME, et al. Risk factors for laryngospasm in children during general anesthesia. Paediatr Anaesth. 2008; 18:289–296. PMID: 18315633.

21. Tait AR, Pandit UA, Voepel-Lewis T, Munro HM, Malviya S. Use of the laryngeal mask airway in children with upper respiratory tract infections: a comparison with endotracheal intubation. Anesth Analg. 1998; 86:706–711. PMID: 9539588.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download