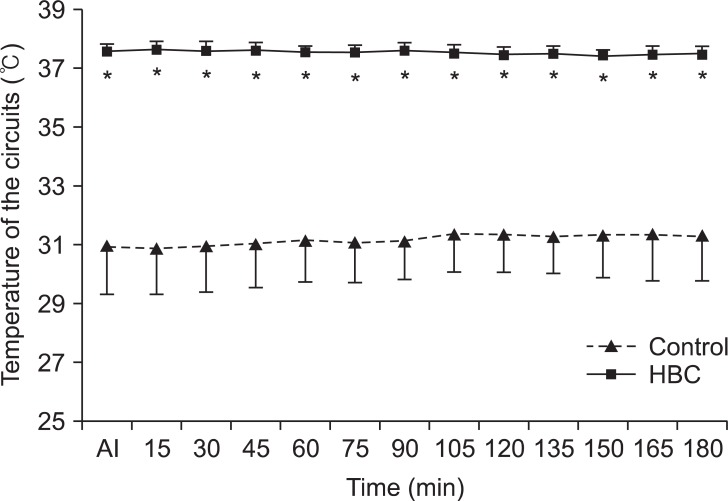
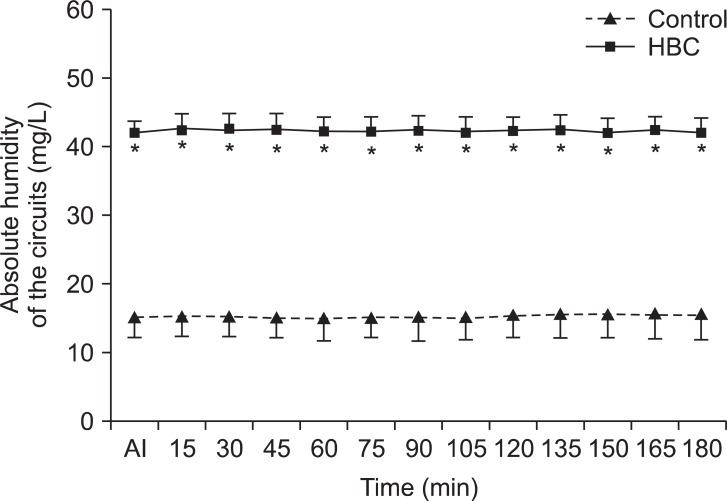
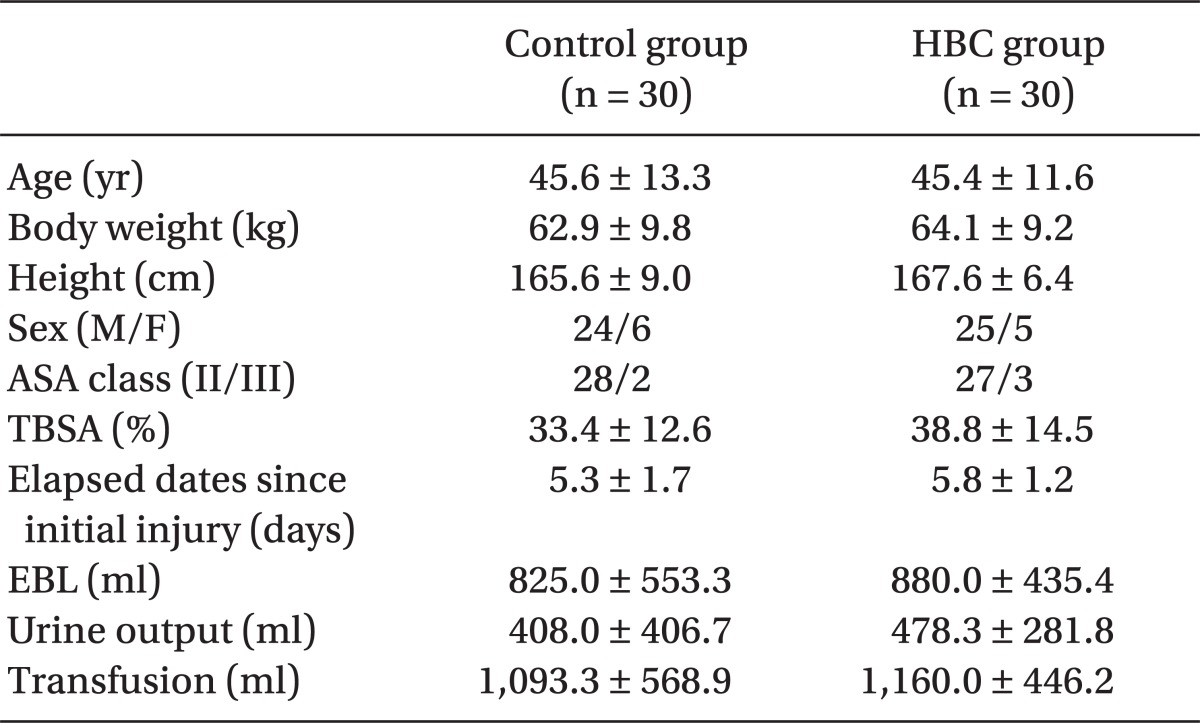
In the present study, the average temperature and absolute humidity of the HBC group were 37.4 ± 0.1℃ and 41.4 ± 0.2 mg/L, respectively, so that the relative humidity was kept at 96%. In contrast, the control group utilizing conventional breathing circuit showed 48% of relative humidity with 31.2 ± 0.2℃ and 15.3 ± 0.2 mg/L for the average temperature and absolute humidity, respectively. This indicated that all of them were significantly lower than that of the HBC group (P < 0.01). According to Williams et al. [
7], ciliary function stopped in rabbits when treating with gases of 50% relative humidity for 30 minutes. After 16 hours with 40% of relative humidity, dogs appeared to have problems in alveolar gas exchange beyond the damages of pneumocytes. In addition, when gases with 60% of relative humidity were utilized in humans for more than 1 hour, the damages were as much as ciliary function impairment, even if they were reversible. In the study, temperature and absolute humidity were 24℃ and 12 mg/L; compared to the results in the control group of the present study (31.2℃, 15.3 mg/L), absolute humidity was relatively higher in the present study, but relative humidity was lower as the temperature of the gases were higher. Since relative humidity is more important than the absolute humidity with regards to the effects of secretions within the airway [
8], relative humidity considering temperature should always be regarded. On the other hand, HBC provided optimum conditions close to physiological environments by holding 98% of relative humidity. Especially in the patients with inspired burns due to flame and smoke, pulmonary complications increase even though the bottom airway is not directly damaged [
3]. As surgery related to burns is generally carried out for more than 3 hours even in the patients without inspired burns, it is necessary to maintain appropriate humidity during anesthesia for a long period of time. From this perspective, HBC would be greatly helpful in patients with severe burns. Right after anesthesia, body heat is transferred to peripheral parts, which possess a little lower temperature from the core parts because of vasodilatations by anesthetics, thereby occurring redistribution hypothermia that the core temperature decreases. This phenomenon lasts for an hour and the core temperature decreases by approximately 1-1.5℃ in the period. Afterward, the body temperature descends almost straightly by more than 3℃ for 2-3 hours, so that it finally reaches the plateau [
9]. Besides, radiation due to the lower atmospheric temperature than that of body temperature, electric heat caused by surgical drapes, and evaporation from the surgical wounds are also the factors determining heat loss. Injection of large volume of cold intravenous fluids also affects temperature changes [
10]. Threshold of temperature control in healthy individuals is 36.5-37.5℃; in case of patients with severe burns; however, it is proportional to the burned area. It is known that the threshold increases by approximately 0.03℃ per total body surface area. As such, in case of burns with more than 25%, the threshold is estimated to elevate by 0.75℃ approximately [
3]. For such reasons, patients with severe burns feel tremble and discomfort at 36.5℃ and may have vasoconstriction in order to maintain higher body temperature. Hypothermia that occurs during anesthesia, even if it is mild, causes many complications, such as wound infection, extending the period of hospitalization, serious cardiac complications, clotting disorders, and delay the discharge from a recovery room [
10]. When hypothermia after anesthesia is recovered slowly in patients with severe burns, it leads to an increase of mortality rate [
3]. This is because that surgery in patients with severe burns of 25% total body surface area may have a great amount of blood loss during a large area of skin tissue removal; also as the wound is spread widely, wound infection and blood clotting disorders, if occurring, are lethal. Therefore, careful monitoring and controlling of body temperature and vital signs are essential for safe anesthesia during the surgery of burned patients. About 90% of metabolic heat dissipates through the surface of the skin and only less than 10% dissipates via respiratory system. Hence, there is no doubt that the effects of heating and dehumidification of airway on maintaining body temperature are limited. Considering the mechanisms of redistribution hypothermia, the best way to maintain body temperature is by either heating the entire body before anesthesia or heating the skin during surgery. However, not only it is practically difficult and dangerous to heat the patients with severe burns whose body temperature has already elevated prior to surgery but also skin heating is unavailable in the case as the surgery is carried out while their entire body is disinfected and exposed without any surgical drapes. Due to such reasons, we made efforts to keep the temperature of the operating room higher than 30℃ and heat all fluids, including disinfecting fluids, that were injected to the patients; however, temperature drop was not completely inhibited. Thus, it was expected that the breathing circuit with heating function would reduce the temperature drop as described in other studies [
4,
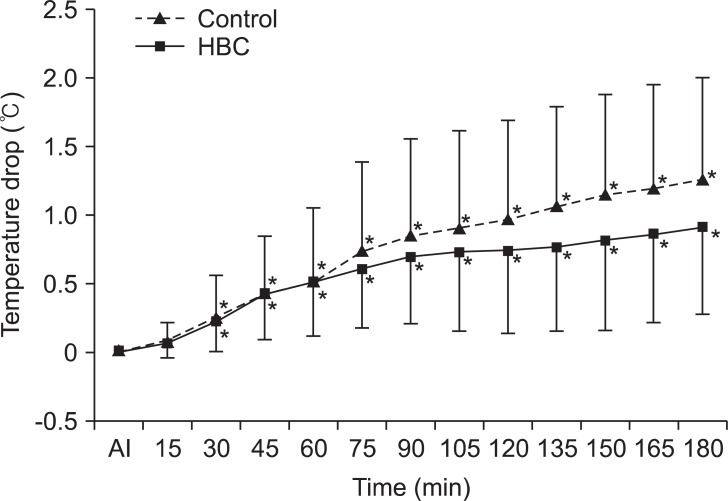
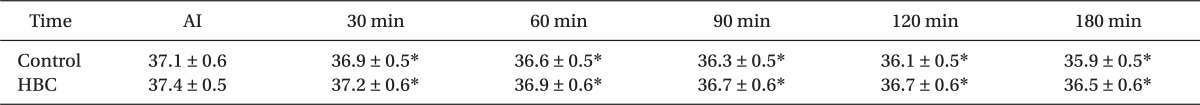
5]; but there was no effect observed in this study. This would be because of the body exposure during the surgery due to extensive skin loss in the burned patients. Even if warm disinfecting fluids are spread throughout the whole body when performing either escharectomy or skin graft, surrounding temperature is maximum 32℃, which is much lower than body temperature; hence, the heat of the body dissipates as the disinfecting fluids evaporate and radiation and conduction proceeds. In this condition, the maintained temperature was not significantly effective compared to the conventional breathing circuit, even though additional heat was applied to maintain them. However, body temperature in patients without burns during anesthesia decreased by 1-1.5℃ within an hour and further by more than 3℃ up till 3 hours; in contrast, the present study was found that the control group and the HBC group showed decreases just by 0.5 ± 0.5℃ and 0.5 ± 0.4℃ at 60 minute anesthesia, and 1.3 ± 0.8℃ and 0.9 ± 0.6℃ at 180 minute anesthesia, respectively. This may be caused by the effects of the various heating methods, including high temperature of the operating room. A study in patients with general anesthesia for lower abdominal surgery [
6] reported that HBC didn't successfully reduce the temperature drop. They also explained the reasons for the exposure of the surgical sites; exposure of lower abdomen, which is the core of the body that causes heat loss as much as counterbalancing the heat in respiratory system. On the other hand, in a study reporting that HBC was effective on the body temperature maintenance [
5], the types of surgery was not notified. In case where several types of surgery were included, the results might not be accurate since the body exposure would not be constantly controlled. Another study investigated [
4] that HBC would decrease the temperature drop in early anesthesia compared to that of conventional circuit by reducing the heat loss due to airway evaporation and conduction in the early stage of hypothermia. The study was carried out in patients who received spinal surgery. After anesthesia, limbs and hips except for backs, the surgical sites, were heated in face-down positions utilizing forced air-warmer at 40-42℃. In result, the temperature drop 60 minutes after anesthesia was greater in the experimental group, but it was similar between the two groups up till 3 hours. In addition, the average temperature drop was approximately 1℃; it was also thought to be because of the additional heating device. Although it is difficult to conclude clearly, given the lack of information regarding the temperature of the operation room in the study, it seems that differences between the results might be because the temperature of the operation room of the present study is generally higher than others, so that it offsets the effects of HBC, thereby affecting the temperature drop of early anesthesia in both groups. Limitation of this study is that the effects of HBC only on body temperature are not able to be compared because of utilization of various heating methods, as mentioned previously. However, this study was considered to be reasonable because the effects of additional heating from breathing circuit were investigated under the same heating conditions in both groups and in the optimum environment to maintain body temperature of the patients for safety. In conclusion, the present study confirmed that HBC utilization during general anesthesia in patients with severe burns did not result in significant reduction of the core temperature drop during surgery. However, the humidity of the inspired gases was capable to be maintained ideally. In the future, more studies may need to be done regarding the methods to reduce the core temperature when performing anesthesia in patients with severe burns during surgery.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download