Laparoscopy results in less scar formation due to smaller incision, and less postoperative pain, facilitating earlier ambulation. These characteristics result in decreased pulmonary complication rate and shortened admission time, leading to numerous advantages such as reduction of medical cost. As laparoscopy involves maximal increase in abdominal pressure through continuous flow of carbon dioxide gas into the abdominal cavity, numerous studies have reported the resulting hemodynamic, respiratory and endocrinologic alterations, as well as surgical complications [1]. We have compared the dynamic compliance, peak airway pressure and respiratory resistance, as the abdominal pressure and body position change during laparoscopic gynecologic surgeries.
This protocol involved 50 patients who were classified as having physical status class I or II according to the American Society of Anesthesiologists, and had no underlying cardiopulmonary diseases or planned elective operations. All patients informed consent prior to being included in the study. All patients were premedicated by glycopyrrolate (0.004 mg/kg) and midazolam (0.06 mg/kg) 30 minutes prior to induction. Anesthesia was induced by intravenous thiopental sodium (5 mg/kg) and vecuronium (0.1 mg/kg). Anesthesia was maintained by volume-controlled ventilation with O2 (2 L/min), N2O (2 L/min) and enflurane (1.5-2 vol%). Additional vecuronium (0.02 mg/kg) was administered to maintain constant muscle paralysis as needed. Tidal volume of 10 ml/kg and respiratory rate of 14/minute was maintained with a volume anesthesia ventilator (Ohmeda, Modulus®). Blood pressure, heart rate, oxygen saturation, and end-tidal carbon dioxide pressure (EtCO2) were measured continuously using patient-monitoring devices. The patients were maintained in 15° lithotomy-Trendelenburg position during operation time, and carbon dioxide was injected at the start of and during operation to achieve and maintain steady abdominal pressure at 14 mmHg for H group and 10 mmHg for L group. Dynamic compliance, peak airway pressure, and respiratory resistance were measured with VENTRAK™ (Novametrix Medical System Inc, USA) at 2 minutes after the beginning of mechanical ventilation (control), 3 minutes after position change (immediately before carbon dioxide insufflation) and 5 and 15 minutes after carbon dioxide insufflation. All measurements are presented as mean±standard deviation, and Wilcoxon signed-rank test and Mann-Whitney test were performed for intra- and inter-group comparison of respiratory dynamics. P values less than 0.05 were determined as statistically significant.
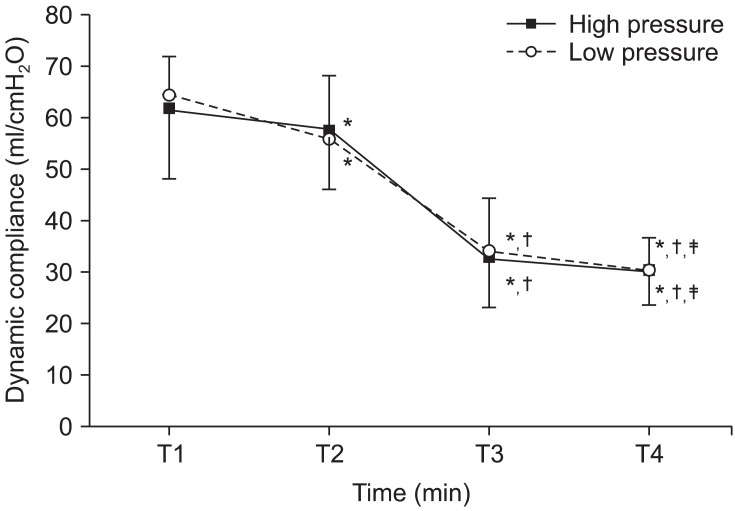
Dynamic compliance in the H group significantly decreased from 61.3 ± 13.2 ml/cmH2O for the control to 57.7 ± 11.6 ml/cmH2O after positional change (P < 0.05), continuing to decrease to 32.5 ± 9.2 ml/cmH2O and 30.3 ± 6.6 ml/cmH2O at 5 minutes and 15 minutes after carbon dioxide insufflation. Dynamic compliance also significantly decreased in the L group at each measurement. There was no significant difference between the H group and L group in dynamic compliance at any measurement point (Fig. 1). In the H group, the peak airway pressure did not change noticeably upon positional change compared to the control, but was significantly elevated with an increasing trend with the passage of time. In the L group, the peak airway pressure was 13.1 ± 2.1 cmH2O for the control, which significantly increased to 14.2 ± 3.2 cmH2O after positional change. The respiratory resistance was not significantly different between the two groups at any measurement point.
The functional residual volume and lung compliance is reduced by 20% upon general anesthesis, with the reduction reaching up to 50% in the case of obesity. When positioned in the Trendelenburg position, the contents of the abdominal cavity shifted toward the head, resulting in poorer functional residual volume, total lung volume, and lung elasticity. Altered functional residual volume led to changes in the character of the lung and the chest wall, which then changed the lung compliance and resistance. Lee et al. [2] reported no difference in the peak airway pressure measured in Trendelenburg and reverse Trendenlenburg positions, while transrespiratory resistance higher in 15° Trendelenburg position compared to 10° reverse Trendelenburg position. However, neither group in our study demonstrated a significant increase in airway resistance after positional change. Kim et al. [3] reported that compared to pelviscopy performed at 10° Trendelenburg position, laparoscopic surgery performed at 10° reverse Trendelenburg position resulted in smaller change in peak airway pressure and lung compliance, suggesting that this may be due to the nature of the reverse Trendelenburg position offsetting the increase in abdominal pressure. In our study, the lung compliance of two groups in the Trendelenburg position decreased by 5.9% and 13.8%, and further decreased by 50.6% and 52.9% when abdominal pressure was maintained at 14 mmHg and 10 mmHg, respectively. Increased abdominal pressured caused by the Trendelenburg position and pneumoperitoneum decreases the functional residual volume even further, and when under mechanical ventilation receiving same tidal volume, leads to change in airway resistance due to increased airway pressure and transpulmonary pressure. Schleifer et al. [4] argued that peak airway pressure rises along with increase in abdominal pressure in laparoscopic gynecologic surgery. Bannister et al. [5] stated that increased abdominal pressure is associated with increased peak airway pressure and decreased lung compliance. This study first attempted to randomize the patients into two groups and apply different degrees of abdominal pressure, 10 mmHg and 14 mmHg. Different abdominal pressures were applied after dividing the patients based on their body weight, from which a comparison of the effect of abdominal pressure was made. Similar results may be expected for fully randomized patient groups with different abdominal pressures applied. Considering that the respiratory mechanism is not different between the two groups, an adequate abdominal pressure according to body weight is believed to be more appropriate than applying a uniform abdominal pressure regardless of body weight, as long as sufficient operating view is obtained.
In conclusion, different abdominal pressures applied to two patient groups undergoing gynecologic laparoscopic surgery did not result in a significant difference in measurements of dynamic compliance, peak airway pressure, and airway resistance in this study.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download