This article has been
cited by other articles in ScienceCentral.
Abstract
Adrenal insufficiency, which is related to hemodynamic instability and increased mortality, has been reported in patients with advanced liver disease regardless of the presence of septic conditions. In this regard, the hepatoadrenal syndrome has been recently proposed as adrenal insufficiency in critically ill patients with liver disease. We describe here a 67-year-old female patient with hepatic failure and adrenal insufficiency. The patient showed stable vital signs and no evidence of sepsis preoperatively. Despite hydrocortisone replacement and inotropics administration, severe intraoperative hemodynamic instability was observed. Hydrocortisone administration was continued postoperatively, nevertheless inotropics could not be tapered. On postoperative day 11, the patient died due to pneumonia and septic shock. Hepatoadrenal syndrome may have played a key role in her severe hemodynamic fluctuation and poor outcome, reinforcing the importance of adrenal function in the liver transplantation surgery.
Go to :

Keywords: Adrenal insufficiency, Hepatic failure, Hepatoadrenal syndrome, Liver transplantation
Adrenal insufficiency is related to catecholamine-resistant hemodynamic instability and is associated with high mortality rates in critically ill patients [
1,
2]. Adrenal insufficiency has been observed in patients with advanced liver disease, with or without septic conditions [
3,
4]. Moreover, 62% of critically ill patients with liver failure have shown subclinical adrenal insufficiency [
5], and 92% of patients undergoing liver transplantation with steroid-free immunosuppression have been diagnosed with adrenal insufficiency [
3]. It has been revealed that both sepsis and end-stage liver disease have a number of common pathophysiologic mechanisms, such as endotoxemia, increased levels of pro-inflammatory mediators, and decreased apoprotein-A/high-density lipoprotein levels [
3,
5-
7]. Recently, a new disease concept, "hepatoadrenal syndrome", has been proposed specifically according to the finding of the adrenal insufficiency in critically ill patients with liver disease [
3], although whether adrenal insufficiency in liver disease is specific to liver failure is not known exactly [
8].
We describe here a patient with suspected hepatoadrenal syndrome who was diagnosed preoperatively with adrenal insufficiency in the absence of overt sepsis and subsequently developed severe hemodynamic instability during and after living donor liver transplantation.
Case Report
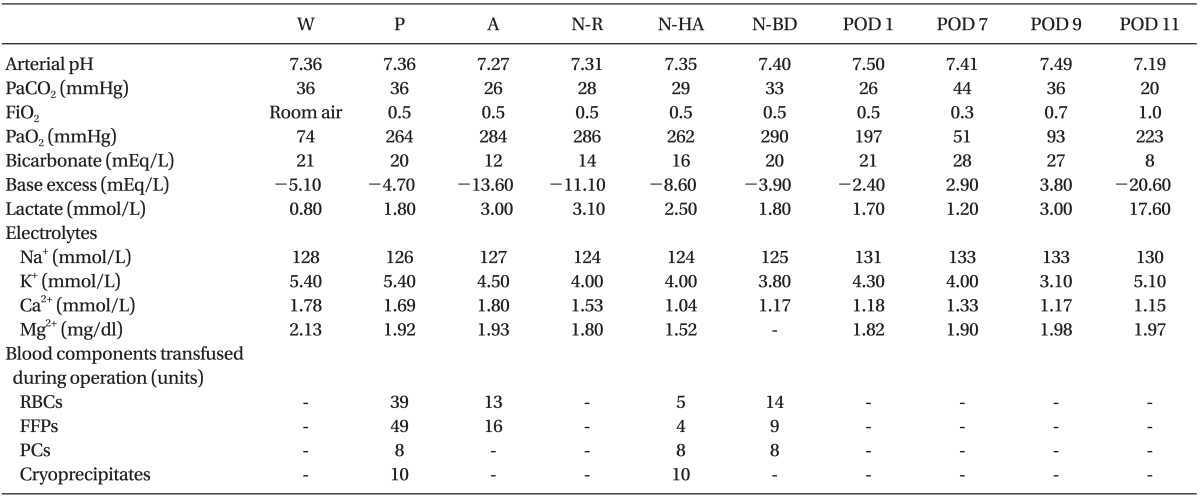
A 67-year-old female patient with adrenal insufficiency in drug-induced hepatic failure previously had a cancer on the left breast, which had been treated by modified radical mastectomy followed by an unknown regimen of adjuvant chemotherapy. Thereafter, she had experienced jaundice with mental change and had been diagnosed with drug-induced liver failure. Despite supportive care, her stuporous mental status did not return, making her a candidate for liver transplantation. Although she was semicomatose, her vital signs were stable and there was no evidence of sepsis. Laboratory analysis revealed unexplained hyponatremia of 121-124 mmol/L and K
+ concentration of 4.8-5.4 mmol/L (
Table 1). A rapid adrenocorticotropic hormone (ACTH) stimulation test was performed to diagnose adrenal insufficiency. Her preoperative random total cortisol concentration was 9.0 µg/dl (adrenal insufficiency: < 10 µg/dl). Thirty minutes after stimulation with 250 µg synacthen, her delta cortisol concentration was 4.9 µg/dl (adrenal insufficiency: < 9 µg/dl). The concentrations of all the other hormones were within the normal ranges. Based on guidelines for the diagnosis of corticosteroid insufficiency in critically ill patients [
9], she was diagnosed with adrenal insufficiency. The patient was started on hydrocortisone therapy (50 mg, tid) preoperatively, and it was maintained during liver transplantation.
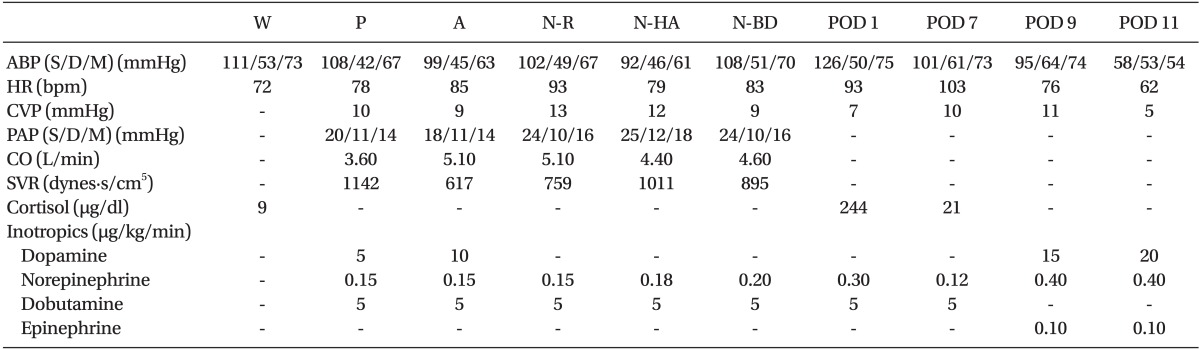
Table 1
Hemodynamic Variables, Cortisol Level and Doses of Infused Inotropics during the Perioperative Period in a Liver Transplant Recipient with Suspected Hepatoadrenal Syndrome
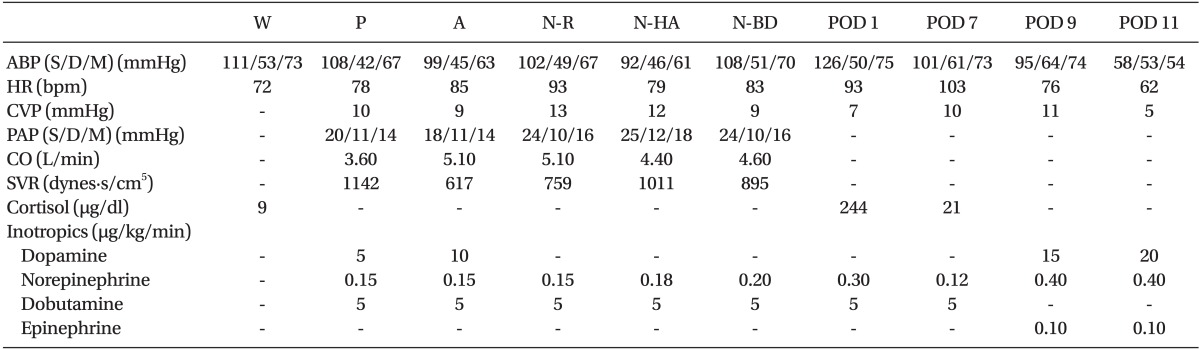

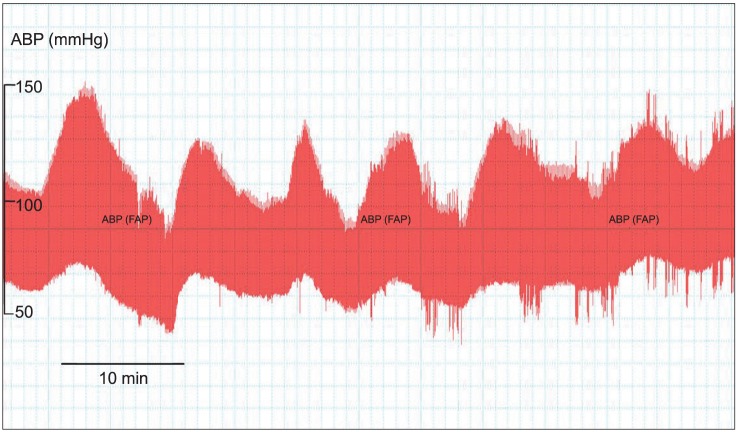
Anesthesia was induced with thiopental sodium, fentanyl, vecuronium, and sevoflurane. Hemodynamic data were recorded in real time during surgery using an online personal computer interfaced with a signal processing software (Windaq, DATAQ instrument, Akron, OH). Thirty minutes after surgical incision, the patient's mean arterial blood pressure (ABP) started to fluctuate and decreased to less than 60 mmHg without significant blood loss. Because intermittent bolus administration of ephedrine was not effective, she was infused continuously with dopamine (5-10 µg/kg/min), dobutamine (5 µg/kg/min) and norepinephrine (0.15-0.2 µg/kg/min), starting from the pre-anhepatic phase of liver transplantation (
Table 1). However, her ABP fluctuated markedly (
Fig. 1). Before graft reperfusion, she was administered 172.5 mg of methylprednisolone (3 mg/kg) for immunosuppression. Immediately after reperfusion, she was administered 40 µg of an epinephrine bolus due to severe hypotension. However, although she was supported by increasing dose of inotropics and vasopressors after graft reperfusion, her ABP continued to fluctuate until the end of the operation. Blood components transfused during operation were shown in
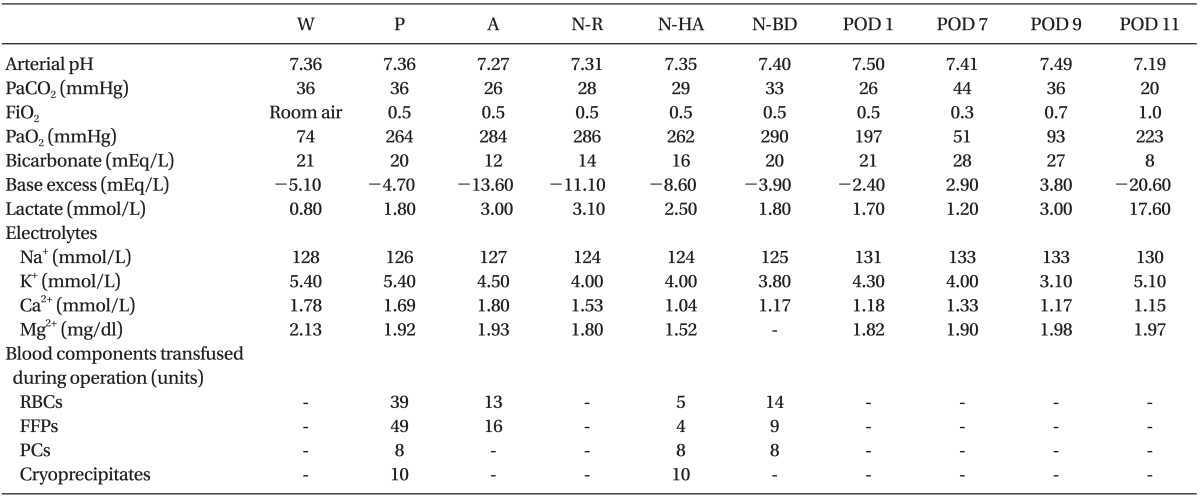
Table 2.
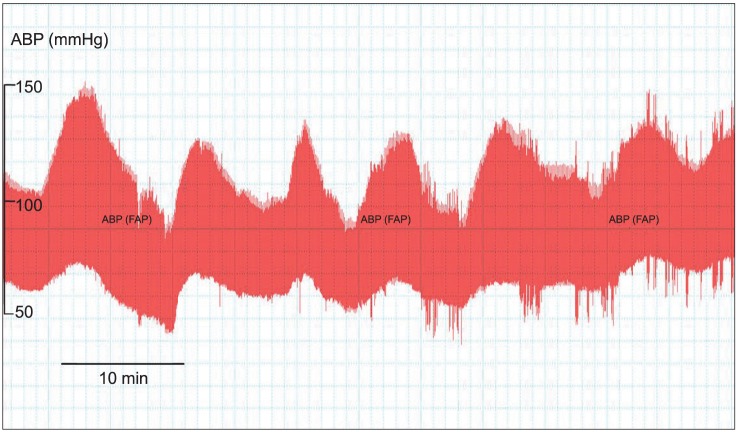 | Fig. 1Changes in arterial blood pressure (ABP) during the pre-anhepatic period of liver transplantation in a patient with suspected hepatoadrenal syndrome. Note that ABP fluctuated markedly 30 min after surgical incision, although blood loss was minimal. FAP: femoral arterial pressure. 
|
Table 2
Arterial Blood Gas Analysis and Electrolytes Concentrations during the Perioperative Period, and Infused Blood Components during Operation in a Liver Transplant Recipient with Suspected Hepatoadrenal Syndrome

Although she was maintained on hydrocortisone postoperatively, inotropics could not be tapered and hemodynamic instability continued (
Table 1). On postoperative day 9, the patient developed atrial fibrillation, and a chest radiograph showed pneumonic infiltration. On postoperative day 11, the patient died due to pneumonia and septic shock.
Go to :

Discussion
Adrenal insufficiency is relatively common in critically ill patients [
9,
10]. Interestingly, there is a high incidence of adrenal insufficiency in critically ill patients with liver disease [
3]. Harry et al. [
5] reported that hemodynamically unstable patients with acute hepatic dysfunction showed significantly lower serum cortisol levels of ACTH stimulation test. They also revealed that the steroid replacement was associated with dose reduction of vasopressor, but not survival, in patients with adrenal insufficiency in liver failure [
4]. Furthermore, Marik et al. [
3,
7] have observed a pathophysiologic association between adrenal insufficiency and low concentrations of high-density lipoprotein, the preferred source of seteroidogenic substrates in the adrenal gland, in patients with liver failure and in post-liver transplant recipients. These findings have led to recognition of the disease entity "hepatoadrenal syndrome". Our patient was not septic and she showed relatively stable vital signs preoperatively. Although hydrocortisone replacement started immediately after diagnosis of adrenal insufficiency, her hemodynamic status was unstable and she required continuous infusion of inotropics during and after liver transplantation. Therefore, she likely had hepatoadrenal syndrome, with adrenal insufficiency playing a role in her cardiovascular instability during and after liver transplantation.
Because most of liver transplant recipients receive supplementary corticosteroids as postoperative immunosuppressants, adrenal insufficiency has been rarely documented in those patients. After the development of steroid-free immunosuppression, several reports have shown adrenal insufficiency in post-liver transplant recipients [
3,
7,
8,
11]. For example, adrenal insufficiency, as manifested by severe multiple organ dysfunction, was observed in a post-liver transplant recipient who had not been administered with steroid immunosuppressants [
11]. That patient had been diagnosed with adrenal insufficiency 40 days after liver transplantation and was successfully treated with corticosteroid [
11]. However, there is little report focused on adrenal insufficiency that occurred before liver transplantation. Our report is a case of a liver transplant recipient to be diagnosed preoperatively with adrenal insufficiency, showing marked ABP fluctuation during liver transplantation surgery. It is well known that the basic concept of adrenal insufficiency is the inadequate activation of hypothalamic-pituitary-adrenal axis with cortisol release to illness and stress [
3,
7,
9]. Even though the present patient showed relatively stable hemodynamic parameters before glucocorticoid replacement, she was treated with hydrocortisone throughout the hospital course after confirming adrenal insufficiency. However, surgical stress may not be tolerated and cause severe hemodynamic instability during liver transplantation despite hydrocortisone replacement therapy, implying importance of adrenal function in liver transplantation.
Several previous studies on patients with liver failure and adrenal insufficiency have focused on sepsis or septic conditions and survival by corticosteroid administration [
4,
5,
12,
13]. Previous studies have reported that corticosteroid therapy has beneficial effects on survival and hemodynamic stability in patients with liver failure and septic shock [
5,
13,
14] and in post-liver transplant recipients [
3,
11-
13]. However, consistent with findings showing that corticosteroid therapy may not improve survival in vasopressor-dependent patients with adrenal insufficiency and liver disease [
4], our patient with suspected hepatoadrenal syndrome did not effectively respond to corticosteroid therapy, eventually expired due to pneumonia and septic shock after liver transplantation. The specific mechanisms underlying these controversial effects of steroid therapy are unknown, but warrant further investigation.
It has been well known that hemodynamic complications in patients with liver failure may be affected by several factors. For examples, low systemic vascular resistance, high cardiac output, combined cirrhotic cardiomyopathy, massive bleeding and coagulopathy, and metabolic status during liver transplantation may be involved in hemodynamic instability in liver failure patients [
15]. Hemodynamic instability in the present patient during and after liver transplantation was not explained completely by the general pathophysiology of liver failure. Because arterial pH, electrolytes, lactate level, and intravascular volume status during liver transplantation surgery were maintained adequately, adrenal insufficiency diagnosed preoperatively was thought to be an important reason for the marked ABP fluctuation during and after liver transplantation surgery in our patient. However, we could not exclude the above mentioned pathophysiological effects.
In conclusion, we found that a patient with adrenal insufficiency suffered severe hemodynamic instability during and after liver transplantation, reinforcing the importance of hepatoadrenal syndrome. These findings indicate that perioperative adrenal function should be monitored carefully in liver transplantation recipients with severe hemodynamic fluctuation.
Go to :





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download