Abstract
Background
The oculocardiac reflex (OCR) can be elicited during manipulation of the orbital structures in the strabismus correction surgery. A sinus bradycardia is the most common manifestation of OCR; and cardiac dysrhythmia and asystole may also occur. Various efforts to reduce OCR have been attempted, but without coherent outcome results.
Methods
Sixty one children, undergoing elective strabismus surgery, were randomly allocated into 2 groups: Group K received ketamine 1.0 mg/kg; and Group M received midazolam 0.15 mg/kg for induction of anesthesia. Anesthesia was maintained with 1-1.3 MAC of sevoflurane with 50% N2O in O2. Heart rate and blood pressure were measured 30 seconds before extraocular muscle (EOM) traction and immediately after traction. The OCR was defined as a decrease in heart rate more than 20% of the baseline heart rate, following manipulating EOM. Postoperative nausea and vomiting (PONV) and emergence agitation (EA) were assessed in postanesthetic care unit (PACU).
Results
Blood pressure before tightening EOM in Group K was higher than that in Group M (P < 0.05). However Δ HR (2.7 ± 15% vs. - 0.9 ± 16%) and incidence of OCR (10.0% vs. 19.4%) after traction an EOM were not different between the two groups. The occurrence of PONV (6.7 vs. 9.7%) and EA (30.0% vs. 22.6%) were similar.
Strabismus is a malalignment of the visual axes. It is the most common cause of pediatric ophthalmic surgery [1,2]. The orbital structure including six extraocular muscles (EOMs) which move the globe within the orbit is manipulated during surgery.
Manipulation of the globe can elicit oculocardiac reflex (OCR). In general OCR is defined as a decrease in heart rate more than 20% from baseline heart rate after pressing globe [3,4]. Other definitions, such as a decrease in heart rate more than 10%, an increase in heart rate more than specific value, and occurrence of any type of dysrhythmia after manipulating of orbital structure are also used [5]. Incidence of OCR varies from 16 to 82% according to its definition [2]. The afferent limb of reflex is from ciliary nerve to ciliary ganglion, to ophthalmic division of the trigeminal nerve, to the trigeminal sensory nucleus near the fourth ventricle. The efferent limb is by the vagus nerve to the heart [1].
The most common manifestation of OCR is a sinus bradycardia but atrioventricular block, ventricular ectopy, ventricular fibrillation, or even asystole may occur. The OCR may be fatal in pediatric patients [6]. It was reported that OCR was exacerbated by orbital injection, hypercapnia, hypoxemia, and inappropriate anesthetic depth [1,2]. To reduce OCR, retrobulbar block and premedication with anticholinergics have been used besides controlling factors stated above [7-11]. Likewise, many articles have proved that the anesthetic agents may influence the incidence of OCR [5,12-17]. In spite of various attempts, the methods of preventing OCR have not been found to be consistently effective.
We use intravenous drugs for induction in the waiting room to reduce separation anxiety of the pediatric patients with their parents. Ketamine and midazolam are used widely, and have different mechanisms. As such, we have designed this study to compare the effects of these drugs on OCR.
Because strabismus surgery is regarded as a stimulant factor for the postoperative nausea and vomiting (PONV) [18], we assessed the incidence of PONV in postanesthetic care unit (PACU). We also planned to investigate the effects of these drugs on the occurrence of emergence agitation (EA).
The informed consent was obtained individually from parents of the children. The criteria for inclusion were children aged from 2 to 9 years, the American Society of Anesthesiologists physical status 1-2, and elective strabismus surgery. Children who exhibited problems of central nervous system, cardiopulmonary system, or other organic dysfunction were excluded. Sixty one children were randomly assigned to 2 groups by choosing a shielded envelope in the waiting room: ketamine (Group K) and midazolam (Group M).
Solid food and milk products were allowed until 6 hours before the surgery, and clear liquids were allowed until 3 hours before the surgery. Children were not premedicated. One hour before arriving in the operating room, a peripheral intravenous route was cannulated with topical anesthesia by EMLA cream (lidocaine-prilocaine; Astra Zeneca, Karlskoga, Sweden). Before the start of surgery, children were monitored with electrocardiography, pulse oximetry, noninvasive blood pressure, and capnography. Anesthesia was induced with ketamine 1.0 mg/kg in Group K and midazolam 0.15 mg/kg in Group M in the waiting room; and maintained with 1.0-1.3 MAC of sevoflurane, corrected for age with 50% N2O in O2. Concentration of sevoflurane was controlled according to mean arterial pressure and heart rate. Tracheal tubes were placed with rocuronium 0.5 mg/kg. Ventilation was adjusted to maintain normocapnia (30-35 mmHg of end-tidal carbon dioxide pressure) with volume controlled ventilation. Peripheral oxygen saturation (SpO2) was maintained more than 98% with 10 ml/kg of tidal volume.
Heart rate and blood pressure were recorded 30 seconds before EOM manipulation (HR 1, BP 1) and immediately after manipulation (HR 2, BP 2). Considering duration of action of ketamine and midazolam, the muscle involved first was included in this study. OCR was defined as a decrease in heart rate more than 20% from the baseline heart rate. When OCR occurred an anesthesiologist asked a surgeon to stop the procedure. If the OCR persisted or severe bradycardia (HR < 60 BPM) developed, 0.01 mg/kg of atropine was given intravenously.
After the surgery was completed, sevoflurane was ceased and residual neuromuscular blockade was reversed with pyridostigmine 0.5 mg/kg glycopyrrolate 0.01 mg/kg. When the children breathed spontaneously and airway reflex was recovered, tracheal tube was removed.
The children stayed in the PACU for 1 hour and transferred to the ward. PONV and EA were assessed in the PACU. Using modified Aono's scale [19], not easily calmed or combative children were enrolled in the agitated group. Only one anesthesiologist and one ophthalmologist participated in this study.
Statistical analysis was performed using SPSS for Windows version 12.0 (SPSS, Chicago, Illinois, USA). Data are expressed as mean ± SD or as number (%). Statistical difference was considered significant at P < 0.05.
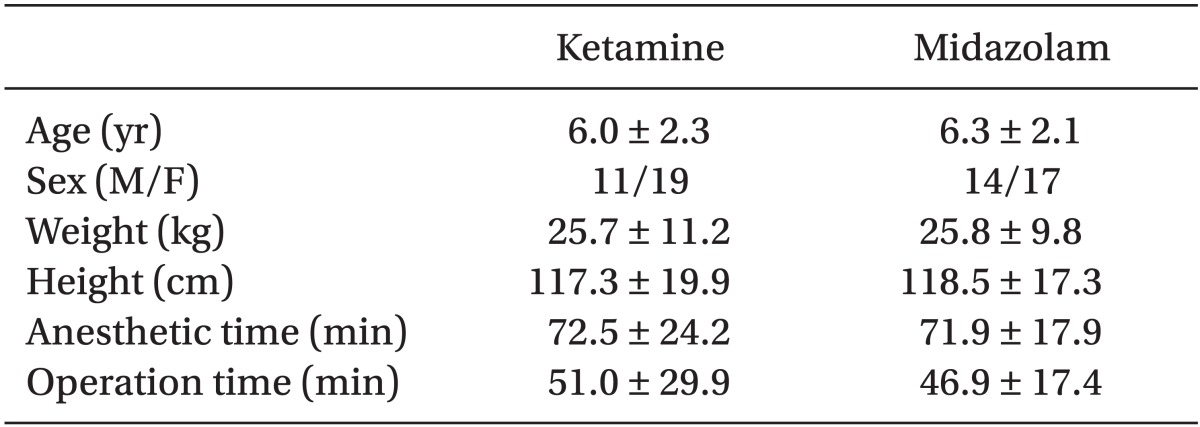
A total of 61 cases were analyzed. Problems with ventilation did not occur during surgery. There were no differences in demographic and clinical data between the two groups (Table 1).
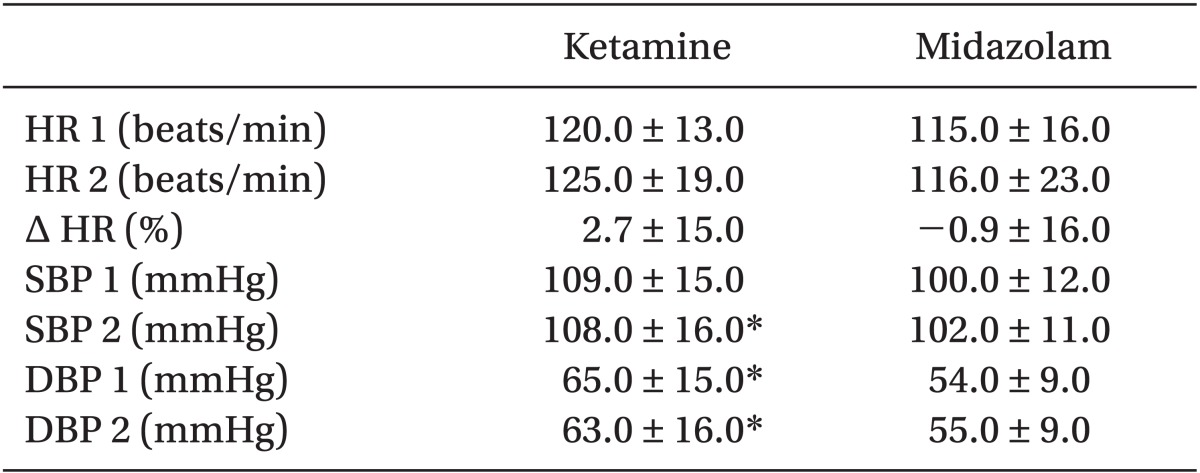
Before and after EOM traction, systolic and diastolic blood pressures were higher in Group K than in Group M (P < 0.05). Heart rate appeared in increasing tendency after EOM manipulation in Group K (2.7 ± 15.0%), but decreasing tendency in Group M (-0.9 ± 16.0%) (Table 2).
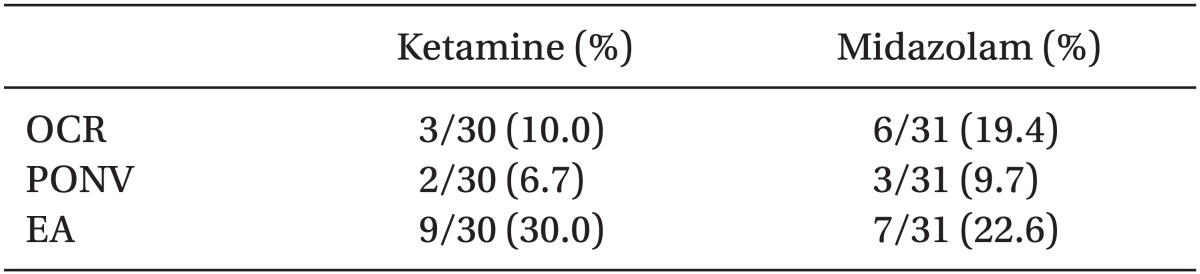
Forty nine cases were assessed on lateral rectus muscle and the incidence of OCR was similar in both groups. On the other muscles, the incidence of OCR was not different between the two groups (Table 3).
Overall incidence of OCR was not different between the two groups (10.0% in Group K vs. 19.4% in Group M) (P = 0.47). The OCR disappeared spontaneously without atropine in all children presenting OCR. In the PACU, incidence of PONV (6.7% in Group K vs. 9.7% in Group M) and EA (30.0% in Group K vs. 26.6% in Group M) was similar (Table 4).
The OCR was first reported by Aschner in 1908 and observed frequently in pediatric strabismus surgery. In this study OCR was defined as a decrease in heart rate more than 20% after pressing globe. Incidence varies from 16 to 82% depending on the definition of OCR [2]. We planned to ask the surgeon to stop stimulation immediately when OCR happened, but if it persisted, atropine should be administered. Most OCR disappears without treatment, but it may seldom bring catastrophic results such as cardiac arrest and sudden death [6]. It is important to understand and manage OCR for the anesthesiologist, but its exact mechanism remains.
Various methods to reduce OCR have been attempted. Premedication with anticholinergics is considered effective to reduce OCR [7], but results are diverse in practice. Misurya et al. [8] demonstrated that patients with premedication by atropine and retrobulbar block with 2% xylocaine did not exhibit positive OCR. Gupta et al. [9] reported that incidence and severity of OCR was significantly lower in children who received peribulbar block by 0.25% of bupivacaine. However to use atropine is controversial because vagolytics can generate undesirable dysrhythmia and diminish cardiac output, particularly in infants. If it penetrates into the central nervous system, central anticholinergic syndrome may be triggered [10,11].
Currently, there are on-going research efforts to reduce OCR, using anesthetic regimen. Chung et al. [12] reported that remifentanil activated parasympathetic tone and had a direct negative chronotropic effect. The continuous infusion of remifentanil induced more change in heart rate following EOM traction than sevoflurane. Allison et al. [13] concluded that sevoflurane depressed vagal activity more than halothane. Bradycardia was less pronounced in patients receiving sevoflurane, when OCR happened. Desflurane is the only volatile agent that increases sympathetic activity, and does not increase the incidence of OCR compared with sevoflurane [14]. It is because vagolytic effect acts more strongly than activation of sympathetic tone in increasing heart rate during steady-state anesthesia with desflurane. However sevoflurane is preferable for very low blood-gas partition coefficient and non-pungency in pediatric surgery. As such, we concluded that sevoflurane was safe and had less influence on OCR. This study was designed to study the maintenance of anesthesia by using sevoflurane.
Braun et al. [10] suggested that OCR consisted of 3 phases. Heart rate decreased passively after traction of EOM in phase 1; heart rate returned after maximal traction (phase 2); and boosted after abrupt release (phase 3) of EOM occurred spontaneously. Ketamine has a cardiostimulatory effect by increasing sympathetic nervous system activity with enhanced norepinephrine release [15], and it may block the phase 1 of OCR. In fact, many anesthesiologists have reported that ketamine compared with other anesthetic drugs is effective for reducing OCR. Hahnenkamp et al. [5] designed the study by using 4 anesthetic regimens, a group of propofol and alfentanil, a group of sevoflurane, a group of ketamine and midazolam, and a group of halothane. It suggested that a combination of ketamine as an analgesic and a volatile anesthetic might be useful for preventing OCR. Choi et al. [16] demonstrated a single bolus of intravenous ketamine resulted in lower incidence of OCR, and it was proportional to the dose of drug. In a recent study, Choi et al. [17] reported that ketamine had little effect on OC,R but propofol or remifentanil was associated with a higher incidence of OCR than sevoflurane and desflurane.
We predicted higher incidence of OCR in midazolam group than in ketamine group. Although the OCR happened frequently in midazolam group, it was insignificant statistically. In addition, Choi et al. [17] demonstrated that the incidence of OCR was similar in ketamine and midazolam group in multi-drug study. The dose of ketamine could be a reason for these results because the former research found that an increase dose of ketamine was associated with lower incidence of OCR [16]. Higher dose of ketamine could produce more OCR with a significant outcome.
PONV after strabismus surgery is an important problem, and the incidence is 50% to 80% without treatment [18]. PONV may be a result of an oculogastric reflex following surgical manipulation of EOM [18]. Sometimes it may result in delayed eating and drinking leading to electrolyte imbalance, dehydration, and prolonged recovery time [20]. Major risk factors of PONV are the type of surgery including strabismus surgery, age more than 3 years old, duration of anesthesia more than 30 minutes, and a personal or family history of PONV or motion sickness [21]. Since strabismus surgery is an independent risk factor for PONV, use of anti-emetics such as ondansetron in high risk group of children is highly efficient and cost-effective [1-3]. Other strategies to minimize PONV include gentle surgical stimulation, an anesthetic plan with propofol rather than inhalation agents [18], a peribulbar block with bupivacaine, and an eye dropping of 2% lidocaine [9]. We predicted that ketamine has a lower incidence of PONV by inhibiting the efferent pathway of the oculogastric reflex; however the incidence of PONV is similar in both groups.
Ketamine is called a dissociative agent, which has been demonstrated as a functional dissociation of the thalamus (relays sensory impulses from the reticular activating system to the cerebral cortex) from limbic cortex (involved in the awareness). The emergence reactions of ketamine include alterations in image, vivid dream, floating sensation, dizziness, and blurred vision [15]. There was a report on the large doses of ketamine (more than 2 mg/kg, intravenous) intensifying this reaction at emergence with prolonged recovery, as more than thiopentone 4 mg/kg and althesin 0.055 ml/kg [22]. However, administration of 1 mg/kg of ketamine intravenously did not affect any emergence agitation in this study.
Although heart rate increased in Group K and decreased in Group M after traction of EOM, the overall incidence of the OCR was not different statistically. We analyzed the limitation of this study as follows. First, the small number of sample could disturb the exact outcome. Because 80.3% cases were on the lateral rectus muscle, to investigate the relation between type of EOM and the incidence of OCR was limited. Second, the definition of OCR was too strict so that effective results could not be produced. In fact the incidence of OCR varied by definition in many articles. Lastly, maintaining the same depth of anesthesia is difficult, since mean alveolar concentration of sevoflurane is altered by age, body weight, and other characteristics of patients. As such, the influence of sevoflurane on OCR cannot be ruled out.
Ketamine did not reduce OCR despite its vagolytic effect; but it did not increase the incidence of PONV and EA. In conclusion, it is reliable to use ketamine for pediatric strabismus surgery.
References
1. Donlon JV, Doyle DJ, Feldman MA. Anesthesia for eye, ear, nose, and throat surgery. In : Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Young WL, editors. Miller's anesthesia. 7th ed. Philadelphia: Churchill Livingstone;2009. p. 2378–2384.
2. McGoldrick KE, Gayer SI. Anesthesia for ophthalmologic surgery. In : Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Stock MC, editors. Clinical anesthesia. 6th ed. Philadelphia: Lippincott Williams & Wilkins;2009. p. 1327–1338.
3. Rodgers A, Cox RG. Anesthetic management for pediatric strabismus surgery: Continuing professional development. Can J Anaesth. 2010; 57:602–617. PMID: 20393822.

4. Dell R, Williams B. Anaesthesia for strabismus surgery: a regional survey. Br J Anaesth. 1999; 82:761–763. PMID: 10536558.

5. Hahnenkamp K, Hönemann CW, Fischer LG, Durieux ME, Muehlendyck H, Braun U. Effect of different anaesthetic regimes on the oculocardiac reflex during paediatric strabismus surgery. Paediatr Anaesth. 2000; 10:601–608. PMID: 11119192.

6. Fayon M, Gauthier M, Blanc VF, Ahronheim GA, Michaud J. Intraoperative cardiac arrest due to the oculocardiac reflex and subsequent death in a child with occult Epstein-Barr virus myocarditis. Anesthesiology. 1995; 83:622–624. PMID: 7661365.

7. Blanc VF. Atropine and succinylcholine: beliefs and controversies in paediatric anaesthesia. Can J Anaesth. 1995; 42:1–7. PMID: 7889577.
8. Misurya VK, Singh SP, Kulshrestha VK. Prevention of oculocardiac reflex (O.C.R) during extraocular muscle surgery. Indian J Ophthalmol. 1990; 38:85–87. PMID: 2387608.
9. Gupta N, Kumar R, Kumar S, Sehgal R, Sharma KR. A prospective randomised double blind study to evaluate the effect of peribulbar block or topical application of local anaesthesia combined with general anaesthesia on intra-operative and postoperative complications during paediatric strabismus surgery. Anaesthesia. 2007; 62:1110–1113. PMID: 17924890.

10. Braun U, Feise J, Mühlendyck H. Is there a cholinergic and an adrenergic phase of the oculocardiac reflex during strabismus surgery? Acta Anaesthesiol Scand. 1993; 37:390–395. PMID: 8322568.

11. Zimmerman G, Steward DJ. Bradycardia delays the onset of action of intravenous atropine in infants. Anesthesiology. 1986; 65:320–322. PMID: 3752579.

12. Chung CJ, Lee JM, Choi SR, Lee SC, Lee JH. Effect of remifentanil on oculocardiac reflex in paediatric strabismus surgery. Acta Anaesthesiol Scand. 2008; 52:1273–1277. PMID: 18823468.

13. Allison CE, De Lange JJ, Koole FD, Zuurmond WW, Ros HH, van Schagen NT. A Comparison of the incidence of the oculocardiac and oculorespiratory reflexes during sevoflurane or halothane anesthesia for strabismus surgery in children. Anesth Analg. 2000; 90:306–310. PMID: 10648311.

14. Oh AY, Yun MJ, Kim HJ, Kim HS. Comparison of desflurane with sevoflurane for the incidence of oculocardiac reflex in children undergoing strabismus surgery. Br J Anaesth. 2007; 99:262–265. PMID: 17556352.

15. White PF, Way WL, Trevor AJ. Ketamine - its pharmacology and therapeutic uses. Anesthesiology. 1982; 56:119–136. PMID: 6892475.
16. Choi SH, Lee SJ, Kim SH, Kim JH, Kwon HH, Shin YS, et al. Single bolus of intravenous ketamine for anesthetic induction decreases oculocardiac reflex in children undergoing strabismus surgery. Acta Anaesthesiol Scand. 2007; 51:759–762. PMID: 17488312.

17. Choi SR, Park SW, Lee JH, Lee SC, Chung CJ. Effect of different anesthetic agents on oculocardiac reflex in pediatric strabismus surgery. J Anesth. 2009; 23:489–493. PMID: 19921355.

18. Watcha MF, Simeon RM, White PF, Stevens JL. Effect of propofol on the incidence of postoperative vomiting after strabismus surgery in pediatric outpatient. Anesthesiology. 1991; 75:204–209. PMID: 1859008.
19. Aono J, Ueda W, Mamiya K, Takimoto E, Manabe M. Greater incidence of delirium during recovery from sevoflurane anesthesia in preschool boys. Anesthesiology. 1997; 87:1298–1300. PMID: 9416712.

20. Gayer S, Tutiven J. Anesthesia for pediatric ocular surgery. Ophthalmol Clin North Am. 2006; 19:269–278. PMID: 16701164.
21. Kovac AL. Management of postoperative nausea and vomiting in children. Paediatr Drugs. 2007; 9:47–69. PMID: 17291136.

22. Saarnivaara L. Comparison of thiopentone, Althesin, and ketamine in anaesthesia for otolaryngological surgery in children. Br J Anaesth. 1977; 49:363–370. PMID: 889650.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download