Abstract
Background
Pain on injection of rocuronium is a common clinical problem. We compared the efficacy of lidocaine, ketorolac, and the 2 in combination as pretreatment for the prevention of rocuronium-induced withdrawal movement.
Methods
For this prospective, randomized, placebo-controlled, double-blind study a total of 140 patients were randomly allocated to one of 4 treatment groups to receive intravenously placebo (saline), lidocaine (20 mg), ketorolac (10 mg), or both (n = 35 for each group), with venous occlusion. The tourniquet was released after 2 min and anesthesia was performed using 5 mg/kg thiopental sodium followed by 0.6 mg/kg rocuronium. The withdrawal response was graded on a 4-point scale in a double-blind manner.
Results
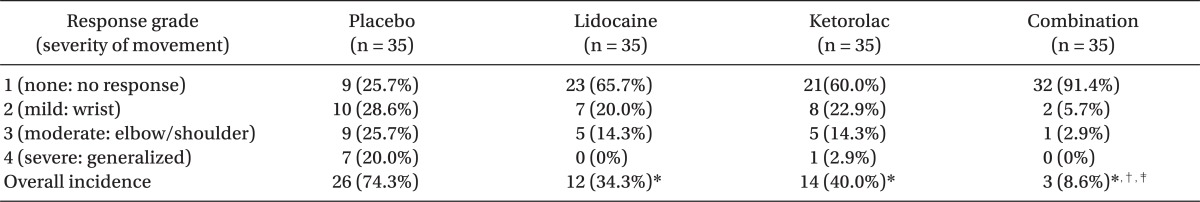
The overall incidence of withdrawal movements after rocuronium was 34.3% with lidocaine (P = 0.001), 40% with ketorolac (P = 0.004), and 8.6% with both (P < 0.001), compared with 74.3% with placebo. There was a significantly lower incidence of withdrawal movements in patients receiving the lidocaine/ketorolac combination than in those receiving lidocaine or ketorolac alone (P = 0.009 and 0.002, respectively). The incidence of moderate to severe withdrawal movements was 14.3% with lidocaine, 17.2% with ketorolac, and 2.9% with lidocaine/ketorolac combination, as compared to 45.7% with the placebo. There was no significant difference in withdrawal movement between the lidocaine group and the ketorolac group.
Conclusions
Ketorolac pretreatment had an effect comparable to that of lidocaine in attenuating rocuronium-induced withdrawal movements and the lidocaine/ketorolac combination pretreatment, compared with lidocaine or ketorolac alone, effectively reduced withdrawal movements during rocuronium injection.
Rocuronium is a widely-used, nondepolarizing muscle relaxant with a rapid onset of action and an intermediate duration. Pain from the injection of rocuronium is a common side effect in anesthetic practice, experienced by 75-100% of patients [1,2]. Even after loss of consciousness during the induction of anesthesia, rocuronium causes localized or generalized movements in 84% of patients [3]. Numerous strategies have been proposed for decreasing the pain associated with rocuronium injection. The most popular strategies involve pretreatment with drugs, such as lidocaine, although no method is completely satisfactory [2-7].
Although the mechanism by which rocuronium causes pain is the subject of speculation, the triggering of a local kinin cascade by kininogen released from the vein walls has been implicated in this pain [7]. Prostaglandins may enhance the action of the products of the kinin cascade on nociceptors present in the vasculature [8]. Non-steroidal anti-inflammatory drugs (NSAIDs) decrease prostaglandin synthesis and inhibit kinin cascades [9]. Ketorolac is an injectable member of the pyrrolo-pyrrole group of NSAIDs and blocks prostaglandin production as an exceptionally potent inhibitor of cyclooxygenase [10,11]. Therefore, ketorolac might be suitable for preventing this distressing side-effect. However, no report has examined as to whether ketorolac pretreatment reduces the withdrawal movement caused by rocuronium injection.
Therefore, this study 1) compared the efficacies of ketorolac and lidocaine at preventing rocuronium-induced withdrawal movements, and 2) evaluated whether the 2 drugs together decrease the withdrawal movements following rocuronium injection more effectively than a single pretreatment.
After Institutional Review Board approval and written, informed consent, we enrolled 140 patients into the study, aged 20 to 75 years, belonging to American Society of Anesthesiologists physical status classification I and II patients scheduled for elective surgery. Patients with difficult venous access on the dorsum of the hand, a known allergy to lidocaine or ketorolac, chronic pain, pregnancy, and those who had received analgesics or sedatives within the previous 24 hours, were excluded from the study.
On patient arrival in the operating room, a 20-gauge cannula was placed in the largest vein on the dorsum of the hand without local anesthesia ensuring free flow by gravity using lactated Ringer's solution as intravenous fluid. All patients were monitored with an electrocardiograph, pulse oximeter, and an automatic noninvasive arterial pressure monitor.
Using a computer-generated randomized table in a sealed envelope, patients were randomly assigned to one of 4 groups to receive placebo (normal saline), lidocaine 20 mg, ketorolac 10 mg, or both lidocaine 20 mg and ketorolac 10 mg intravenously with venous occlusion. If the volume to be administered was below 2 ml, normal saline was added to a total volume of 2 ml. The dosages of lidocaine (20 mg) and ketorolac (10 mg) were chosen based on previous reports investigating their analgesic effects on pain during the injection of rocuronium or propofol [2,12]. All study drugs were prepared in identical syringes and covered by personnel, who did not participate in this study. After the route of intravenous infusion was occluded by applying a rubber tourniquet to the forearm, the study drug at room temperature was administered, and the tourniquet was released after 2 min. Anesthesia was induced using thiopental sodium 5 mg/kg over 10 s. When the eyelash reflex was abolished, 0.6 mg/kg of 1% rocuronium was injected over 10 s. An investigator, who was blinded to patient group assignment, observed patient movement during and after rocuronium administration. The response was graded on the following scale: 1 (none) = no response, 2 (mild) = movement at the wrist only, 3 (moderate) = movement involving upper arm or shoulder, or 4 (severe) = movement in more than one extremity or a generalized response.
Based on an estimated incidence of 75%, a power analysis indicated that a sample size of 35 in each group was sufficient to have 90% power of detecting a 50% reduction in incidence to 37.5% of withdrawal movements at 95% significance level. Data are expressed as means ± SD or numbers (percentages). Patient characteristics were compared by one-way analysis of variance or chi-square test, as appropriate. The incidence of withdrawal movement was analysed using the chi-square test. SPSS software (version 13.0; SPSS Inc, Chicago, IL, USA) was used. A value of P < 0.05 was considered significant.
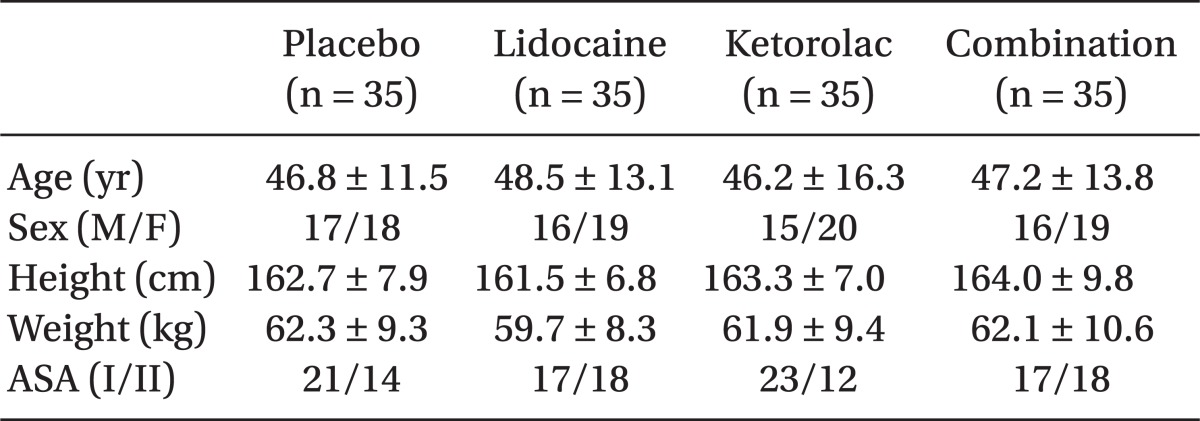
There was no significant difference in the demographic characteristics among the 4 groups (Table 1).
The incidence of withdrawal movements after rocuronium was 34.3% with lidocaine (P = 0.001), 40% with ketorolac (P = 0.004), and 8.6% with both (P < 0.001), compared with 74.3% with placebo. There was a significantly lower incidence of withdrawal movements in patients receiving the lidocaine/ketorolac combination than in those receiving lidocaine or ketorolac alone (P = 0.009 and 0.002, respectively). The incidence of moderate to severe withdrawal movements was 14.3% with lidocaine (P = 0.004), 17.2% with ketorolac (P = 0.01), and 2.9% with lidocaine/ketorolac combination (P < 0.001), as compared to 45.7% with the placebo. There was a significantly lower incidence of moderate to severe withdrawal movements in patients receiving the lidocaine/ketorolac combination than in those receiving ketorolac (P = 0.046), although there was no significant difference compared with lidocaine (P = 0.088). There was no significant difference in withdrawal movements between the lidocaine and ketorolac groups (Table 2).
No adverse effects were seen at the injection site (eg, pain, edema, wheals, inflammation, or hematoma) within 24 hours postoperatively, in any of the groups.
The major finding of this study was that 1) ketorolac with venous occlusion, significantly reduced the incidence of rocuronium-induced withdrawal movements, from 74.3% in the placebo group to 40% in the ketorolac group, which was similar to the 34.3% after lidocaine and 2) the combination of lidocaine and ketorolac was more efficacious in decreasing the incidence of withdrawal movements during the injection of rocuronium than either treatment alone (8.6% versus 40% or 34.3%).
The mechanism of rocuronium-induced pain remains obscure, although various theories have been postulated. These include direct activation of nociceptors by the low pH or nonphysiological osmolality, or activation via the local release of endogenous mediators such as kinin [1,13,14]. However, Borgeat and Kwiatkowski [14] showed that patients, who received normal saline adjusted to pH 4.0, reported no pain. Tuncali et al. [15] showed that undiluted (10 mg/ml) rocuronium caused significant pain on injection compared to diluted preparations (1 or 0.5 mg/ml), although the osmolality of both preparations did not differ significantly. These results render causes associated with pH or osmolality unlikely. Instead, an enzymatic cascade, possibly the local kinin cascade triggered by kininogen, is suspected of being the likely mechanism. According to Borgeat and Kwiatkowski [14], the nature of the pain with rocuronium (eg, immediate, short-duration pain with a marked decrease in severity with repeated administration) probably reflects a direct irritant effect on the kinin cascade. These characteristics of rocuronium injection pain are similar to the characteristics of pain induced by the intravenous injection of propofol. Therefore, mediators that are related to the pain induced by propofol injections may also be involved in the pain associated with rocuronium injection [14,16]. Huang et al. [12] demonstrated that pretreatment with 10 mg ketorolac with venous occlusion for 2 min reduced the propofol injection pain. They compared the retention time under venous occlusion and commented that sufficiently long venous occlusion (120 s, but not 30 or 60 s) played a significant role in reducing this pain. Therefore, we used the same dose of ketorolac and venous occlusion to hold the ketorolac within the vein for 2 min, allowing time to inhibit the kinin cascade peripherally. We drew a similar conclusion: ketorolac pretreatment alleviated withdrawal movements during rocuronium injection. Therefore, the reduction in withdrawal movements that we observed could also be the result of a local peripheral action via inhibition of the kinin cascade through the cyclooxygenase pathway. Indeed, experimental data suggest that ketorolac produces analgesia, mainly peripherally, by reducing sensitizing prostaglandins [17,18], although some NSAIDs also have a central action [19].
Ketorolac improved the tourniquet tolerance and quality of postoperative analgesia when it was combined with lidocaine as intravenous regional anesthesia [20,21]. Studies indicate that 20 mg of ketorolac is effective in intravenous regional anesthesia without adverse effects, implying that a larger dose may increase the risk of local complications [21,22]. We used 10 mg of ketorolac with the venous occlusion technique and no localized complications, such as pain, edema, wheal, inflammation, or hematoma were observed at the injection site within 24 hours, postoperatively.
Based on our literature search, ours appears be the first investigation of the efficacy of ketorolac alone or in combination with lidocaine as pretreatment for reducing pain on injecting rocuronium. Although lidocaine pretreatment has positive results and is widely used for reducing rocuronium injection pain, it is contraindicated in patients with lidocaine allergy [23]. Based on our results, ketorolac could be a useful alternative pretreatment for patients allergic to lidocaine. In other cases, the lidocaine/ketorolac combination could be a more effective pretreatment option.
In conclusion, ketorolac pretreatment had an effect comparable to that of lidocaine in attenuating rocuronium-induced withdrawal movements and the lidocaine/ketorolac combination pretreatment, compared with lidocaine or ketorolac alone, effectively reduced withdrawal movements during rocuronium injection.
References
1. Lockey D, Coleman P. Pain during injection of rocuronium bromide. Anaesthesia. 1995; 50:474. PMID: 7793569.

2. Cheong KF, Wong WH. Pain on injection of rocuronium: influence of two doses of lidocaine pretreatment. Br J Anaesth. 2000; 84:106–107. PMID: 10740559.

3. Shevchenko Y, Jocson JC, McRae VA, Stayer SA, Schwartz RE, Rehman M, et al. The use of lidocaine for preventing the withdrawal associated with the injection of rocuronium in children and adolescents. Anesth Analg. 1999; 88:746–748. PMID: 10195516.

4. Memiş D, Turan A, Karamanlioğlu B, Süt N, Pamukçu Z. The prevention of pain from injection of rocuronium by ondansetron, lidocaine, tramadol, and fentanyl. Anesth Analg. 2002; 94:1517–1520. PMID: 12032018.

5. Liou JT, Hsu JC, Liu FC, Ching-Wah Sum D, Lui PW. Pretreatment with small-dose ketamine reduces withdrawal movements associated with injection of rocuronium in pediatric patients. Anesth Analg. 2003; 97:1294–1297. PMID: 14570640.

6. Kim JY, Kim JY, Kim YB, Kwak HJ. Pretreatment with remifentanil to prevent withdrawal after rocuronium in children. Br J Anaesth. 2007; 98:120–123. PMID: 17065169.

7. Borgeat A, Kwiatkowski D, Ruetsch YA. Spontaneous movements associated with rocuronium injection: the effects of prior administration of fentanyl. J Clin Anesth. 1997; 9:650–652. PMID: 9438893.

8. Ferreira SH. Peripheral analgesia: mechanism of the analgesic action of aspirin-like drugs and opiate-antagonists. Br J Clin Pharmacol. 1980; 10(Suppl 2):237S–245S. PMID: 6254551.

9. Roberts LJ, Morrow JD. Hardman JG, Limbird LE, editors. Analgesic-antipyretic and anti-inflammatory agents and drugs employed in the treatment of gout. Goodman & Gilman's The Pharmacological Basis of Therapeutics. 2001. 10th ed. New York: McGraw-Hill;p. 687–731.
10. Stanski DR, Cherry C, Bradley R, Sarnquist FH, Yee JP. Efficacy and safety of single doses of intramuscular ketorolac tromethamine compared with meperidine for postoperative pain. Pharmacotherapy. 1990; 10:40S–44S. PMID: 2082312.
11. Pallapies D, Salinger A, Meyer zum, Atkins DJ, Rohleder G, Nagyiványi P, et al. Effects of lysine clonixinate and ketorolac tromethamine on prostanoid release from various rat organs incubated ex vivo. Life Sci. 1995; 57:83–89. PMID: 7603299.

12. Huang YW, Buerkle H, Lee TH, Lu CY, Lin CR, Lin SH, et al. Effect of pretreatment with ketorolac on propofol injection pain. Acta Anaesthesiol Scand. 2002; 46:1021–1024. PMID: 12190806.

13. Klement W, Arndt JO. Pain on i.v. injection of some anaesthetic agents is evoked by the unphysiological osmolality or pH of their formulations. Br J Anaesth. 1991; 66:189–195. PMID: 1817619.

14. Borgeat A, Kwiatkowski D. Spontaneous movements associated with rocuronium: is pain on injection the cause? Br J Anaesth. 1997; 79:382–383. PMID: 9389860.

15. Tuncali B, Karci A, Tuncali BE, Mavioglu O, Olguner CG, Ayhan S, et al. Dilution of rocuronium to 0.5 mg/ml with 0.9% NaCl eliminates the pain during intravenous injection in awake patients. Anesth Analg. 2004; 99:740–743. PMID: 15333404.

16. Blunk JA, Seifert F, Schmelz M, Reeh PW, Koppert W. Injection pain of rocuronium and vecuronium is evoked by direct activation of nociceptive nerve endings. Eur J Anaesthesiol. 2003; 20:245–253. PMID: 12650497.

17. Cashman JN. The mechanisms of action of NSAIDs in analgesia. Drugs. 1996; 52(Suppl 5):13–23. PMID: 8922554.

18. Rice AS, Lloyd J, Bullingham RE, OSullivan G. Ketorolac penetration into the cerebrospinal fluid of humans. J Clin Anesth. 1993; 5:459–462. PMID: 8123270.

19. Burian M, Geisslinger G. COX-dependent mechanisms involved in the antinociceptive action of NSAIDs at central and peripheral sites. Pharmacol Ther. 2005; 107:139–154. PMID: 15993252.

20. Reuben SS, Steinberg RB, Kreitzer JM, Duprat KM. Intravenous regional anesthesia using lidocaine and ketorolac. Anesth Analg. 1995; 81:110–113. PMID: 7598236.

21. Steinberg RB, Reuben SS, Gardner G. The dose response relationship of ketorolac as a component of intravenous regional anesthesia with lidocaine. Anesth Analg. 1998; 86:791–793. PMID: 9539603.
22. Souter AJ, Fredman B, White PF. Controversies in the perioperative use of nonsteroidal anti-inflammatory drugs. Anesth Analg. 1994; 79:1178–1190. PMID: 7978444.
23. Chin TM, Fellner MJ. Allergic hypersensitivity to lidocaine hydrochloride. Int J Dermatol. 1980; 19:147–148. PMID: 7390682.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download