Abstract
We report that intraoperative NIM-2 monitoring devices can interfere with bispectral index monitoring. A 45-year-old male with chronic otits media underwent tympanolasty under general anesthesia with NIM-2 monitoring and bispectral index monitoring at our institution. And then, bispectral index monitoring was severely interrupted by facial nerve monitoring.
Bispectral Index Monitoring (BIS) has been used in clinical anesthesia as a monitoring device with the purpose of measuring the depth of anesthesia and as a means to reduce patient awakening. This device provides reliable information in most cases, but it is known that electrical surgical devices, certain clinical situations, abnormal electroencephalogram (EEG) patterns and neuromuscular blocking agents (NMBA) are known to lower the accuracy of BIS figures [1]. Most recently, the NIM-2 nerve integrity monitoring device (NIM-Response 2.0, Medtronic Xomed, USA) has been used in surgeries that require monitoring of specific nerves, which detects damage to nerves during surgery, while also preventing permanent nerve damage. However, due to its operating principle, it can generate electrical signals that can affect BIS. The authors observed a phenomenon where the BIS values were not affected while monitoring the recurrent laryngeal nerve, but the BIS values were interrupted severely while monitoring the facial nerve, thus we are reporting this case.
A 45 year-old male patient came to the hospital to receive tympanoplasty for chronic otitis media. There were no past history or family history before the surgery. The patient was 66.6 kg and 164 cm tall, and all physical and general examination results were normal other than the ventricular bradycardia of 58 beats per minute in the ECG. Glycopyrrate (0.2 mg) was IM injected as a pre-anesthetic medication, while vital signs before anesthesia were normal other than the ventricular bradycardia of 45 beats per minute.
Intravenous anesthesia was planned, rather than anesthesia using a volatile agent, in order to perform nerve integrity monitoring during surgery. Before inducing anesthesia, the BIS sensor was attached while the patient was conscious, and the BIS values registered 95. Medication was started with Fresofol® MCT 2% (Fresenius Kabi, Bad Homburg, German), with a target site concentration of 6 µg/ml and Remifentanil target site concentration of 4 ng/ml using Orchestra base primea (Fresenius Kabi, Bad Homburg, German). After confirming loss of consciousness, rocuronium (50 mg) was IV injected and manual ventilation was maintained with oxygen at 6 L/min. After confirming that there was sufficient muscle relaxation and with BIS values decreased to 44, oral intubation was performed with an endotracheal tube, with a diameter of 7.5 mm (Safety-Flex™, Mallinckrodt), using a curved laryngoscope. Ventilation was maintained with O2 of 1.5 L/min and air of 2 L/min, and with a target site concentration of 3.5 µg/ml and Remifentanil target site concentration of 3.0 ng/ml being continuously IV injected, the BIS values were maintained between 41 to 60.
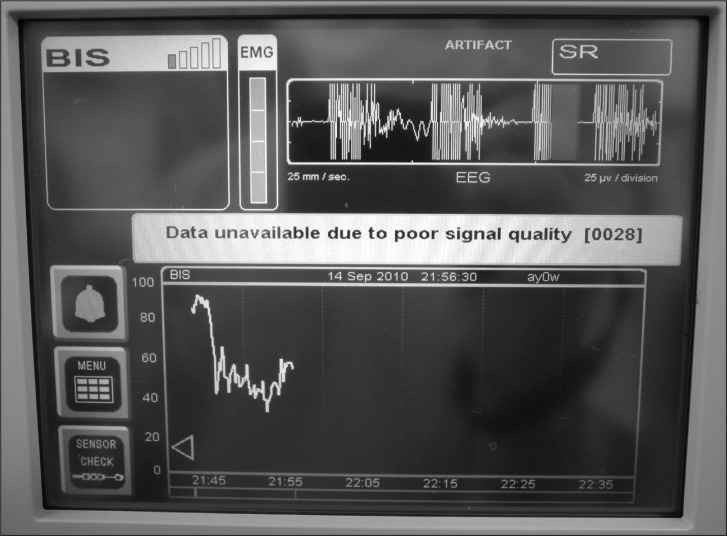
Subsequently, the NIM-2 was attached, and when electricity was applied to measure the resistance in the facial nerve monitoring mode, a severe artifact in the EEG was observed intermittently for 15 seconds on the BIS monitor. A message then appeared on the BIS monitor indicating that the data unavailable due to poor signal quality, so further BIS monitoring was impossible (Fig. 1). Hence, when NIM-2 monitoring was discontinued, the EEG was monitored normally again and it was observed that the BIS monitor was able to read the values.
It was impossible to monitor NIM-2 and BIS simultaneously, but the BIS values had been stable during continuous IV injection of the medication before starting NIM-2 monitoring, while the surgery itself was a stable surgery, so it was decided not to observe BIS values during NIM-2 monitoring, and instead, a continuous IV injection speed with target site concentration of Fresofol at 3.5 µg/ml and Remifentanil at 3.0 ng/ml was maintained. The surgery continued without BIS monitoring, but when NIM-2 monitoring was suspended, before the suturing of the operated area at the completion of tympanoplasty, EEG waves were detected on the BIS monitor again. After completing the suture and dressing of the operated area, all administered anesthetics were suspended. When spontaneous respiration was observed, following the increase in BIS values, pyridostigmine (10 mg) and glycopyrrolate (0.4 mg) were administered in order to reverse muscle relaxation. When spontaneous respiration was sufficiently recovered, BIS monitor showed a value of 91 and the patient was able to open his eyes and obey oral commands. At this point, extubation was performed and the patient was moved to the recovery room. The total surgery time was 3 hours, with the anesthesia time at 3 hours and 45 minutes.
The patient was moved to the ward from the recovery room with no special problems, and was discharged after undergoing a recovery period of 5 days in the hospital ward.
The BIS is a multifactorial parameter obtained from the EEG, which monitors the hynagogue of anesthesia, and is calculated through the general anesthesia experiences of numerous volunteers and patients using several different anesthetic agents [2]. It is expressed as values between 0-100, where patients not under anesthesia show 90-100, while 0 is shown when cortical electrical activity is completely oppressed. Values of 40-60 imply that the possibility of awakening and cognition during surgery is low [3]. BIS monitoring during surgery allows the maintenance of a suitable level of sedation or depth of anesthesia, and can prevent unnecessary deep anesthesia, excessive administration of medications, hypotension, awakening during anesthesia, and memory formation [1].
However, there are research results which report that electrical equipment, the specific clinical state, abnormal EEG patterns, and NMBA, as well as a number of other factors, can interfere with BIS monitoring [1]. For example, there was a case where the BIS increased to 90 when an atrial pacemaker was used during heart surgery, however, this value decreased when the pacemaker was turned off [4]. Also, when a forced-airwarming blanket was directly operated on the patient's face, a false elevation of BIS was observed, with BIS again returning to normal when the operation of the blanket was stopped [5]. There has also been a report that BIS rapidly increased during shoulder arthroscopy when the shaver was started and began generating oscillations [6]. Sloane reported a total thyroidectomy case that combined BIS and recurrent laryngeal nerve monitoring of the electromyography endotracheal tube. During this surgery, the BIS figures rapidly increased, and despite additional administration of midazolam and etomidate, there were no changes in the BIS figures. However, when the EMG stimulator was turned off, the BIS values decreased from 75 to 24 [7].
For this case, NIM-2 equipment was used to prevent facial nerve injury during tympanoplasty. Sub-dermal electrode 1 was attached to the orbicularis oculi muscle area, and electrode 2 was attached to the orbicularis oris muscle area. When current stimulation was given from the standard monopolar probe, a resulting EMG response was detected. When a facial nerve is stimulated, an attached alarm is sounded to notify the operating surgeon. This device, in principle, passes electric currents of 0.8-1.0 mA through electrodes in regular intervals to grasp the accurate location of the electrodes. These electric currents seem to flow into the BIS electrodes, which receive EEGs to cause interference. In effect, as the equipment was activated, an EEG artifact occurred on the BIS monitor, which was stably monitoring at the time, while the BIS values were substantially interfered and were unable to continue monitoring. Not only for this patient, but similar phenomena were observed in other patients using the same monitoring equipment, while receiving the same surgery.
In comparison, this phenomenon did not occur in thyroidectomy procedures experienced by the authors using this same monitoring equipment. When performing thyroidectomy, an endotracheal intubation is performed with a NIM EMG reinforced endotracheal tube (NIM® EMG endotracheal tube, Medtronic Xomed, USA), electrodes are mounted so that they make contact with the vocal cords, and standard monopolar probes are also used in order to monitor the stimulation of the recurrent laryngeal nerve. In these cases, the EEG waves were continuously monitored without artifacts on the BIS monitor, which is in stark contrast to the monitoring of the facial nerve.
No large differences were observed, as the same NIM-2 equipment was used and the electric current used for stimulation was approximately 1.0 mA, but the different results are considered to be related to the distance of the stimulus electrodes from the BIS probe. The electric signal for stimulation enters through each electrode and generally comes out through the grounds attached to the chest, but in facial nerve monitoring, the electric current enters through the electrodes attached next to the eyes, which are close to the front forehead where the BIS probes are attached, so it is highly possible that these electric signals can enter into the BIS probe. In contrast, when monitoring the recurrent laryngeal nerve, electric currents enter through the vocal cord and the current flows towards the chest where the grounds are located, so there is a low possibility of the electric currents traveling upwards. Even when there is an electric current leak, they are greatly decreased when reaching the forehead area, so the effect should be insignificant.
Therefore, when NIM-2 monitoring is used, operating surgeons should be fully aware that the reliability of the BIS can decline when monitoring the facial nerves. A method to reduce this unreliability is to accurately install the location of the electrodes so that the least mA of the stimulating current is given to the BIS. When the depth of anesthesia is uncertain or in patients who have a high risk of awakening during surgery, methods, such as the stopping of NIM-2 monitoring during regular intervals in order to check BIS, should be adopted. When monitoring the recurrent laryngeal nerve, there are fewer interruptions from the stimulating electric currents on the BIS values so relatively reliable information can be obtained. However, in order to obtain more accurate values, it is necessary to adjust the location of the electrodes so that they have the least possible stimulating electric current.
Recently, with the increase in interest and information of the general public regarding anesthesia, the use of BIS monitoring is vitalized as awakening or cognition during anesthesia emerges as a sensitive issue. BIS provides reliable information in objective figures for the depth of anesthesia, but safer anesthesia can be provided to the patient when it is understood that other monitoring devices and surgical equipment used during surgery, such as NIM-2, can have a distinct influence on BIS monitoring.
References
1. Duarte LT, Saraiva RA. When the bispectral index (BIS) can give false results. Rev Bras Anestesiol. 2009; 59:99–109. PMID: 19374221.

2. Liu J, Singh H, White PF. Electroencephalographic bispectral index correlates with intraoperative recall and depth of propofol-induced sedation. Anesth Analg. 1997; 84:185–189. PMID: 8989022.

3. Punjasawadwong Y, Boonjeungmonkol N, Phongchiewboon A. Bispectral index for improving anesthetic delivery and postoperative recovery. Cochrane Database Syst Rev. 2007; 4:CD003843. PMID: 17943802.

4. Gallagher JD. Pacer-induced artifact in the bispectral index during cardiac surgery. Anesthesiology. 1999; 90:636. PMID: 9952180.

5. Hemmerling TM, Fortier JD. Falsely increased bispectral index values in a series of patients undergoing cardiac surgery using forced-air-warming therapy of the head. Anesth Analg. 2002; 95:322–323. PMID: 12145044.

6. Hemmerling TM, Migneault B. Falsely increased bispectral index during endoscopic shoulder surgery attributed to interferences with the endoscopic shaver device. Anesth Analg. 2002; 95:1678–1679. PMID: 12456438.

7. Sloan PA. Interference of bispectral index monitoring with intraoperative use of the electromyograph endotracheal tube. Can J Anaesth. 2007; 54:1028–1029. PMID: 18056216.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download