This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Etomidate has a stable hemodynamic profile after induction, but hypertension and tachycardia are frequent after intubation as well as myoclonus. We compared the effects of fentanyl and remifentanil on the hemodynamic response to intubation and myoclonus during etomidate induction in elderly patients.
Methods
Ninety ASA I or II patients aged over 65 were randomly assigned to 3 groups. Group C received normal saline 10 ml (n = 30), group F and R were pretreated with fentanyl 1.0 µg/kg (n = 30) or remifentanil 1.0 µg/kg with continuous infusion of 0.1 µg/kg/min (n = 30) 1 min before induction with etomidate 0.2 mg/kg. Endotracheal intubation was performed after administration of rocuronium 0.8 mg/kg. Systolic blood pressure (SBP), mean arterial pressure, diastolic blood pressure (DBP), heart rate (HR), and the incidence and intensity of myoclonus were recorded.
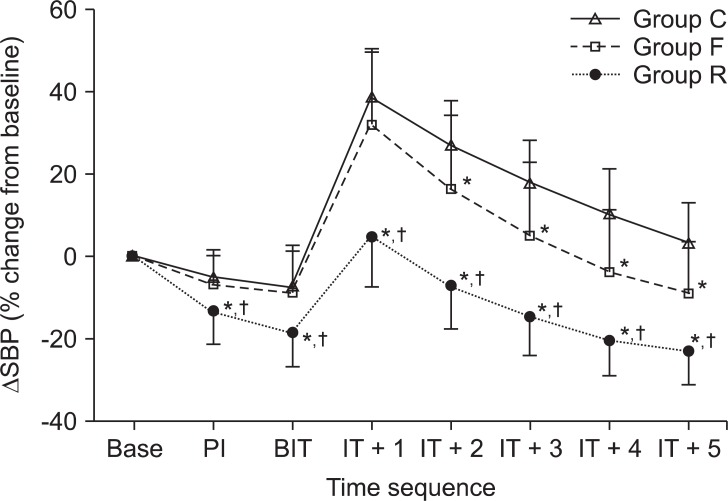
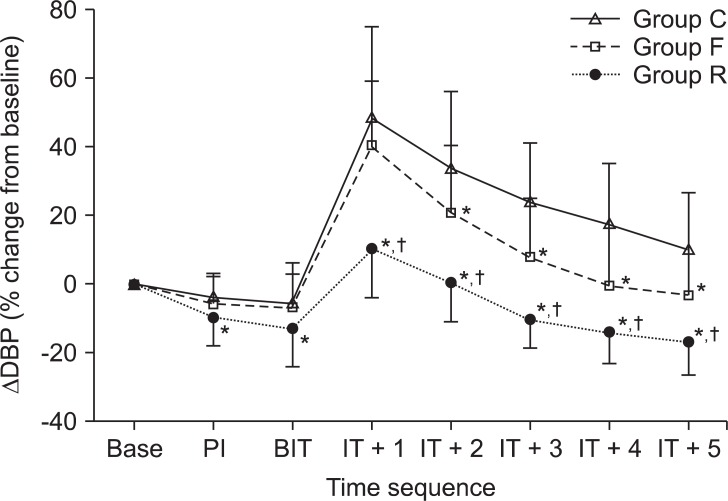
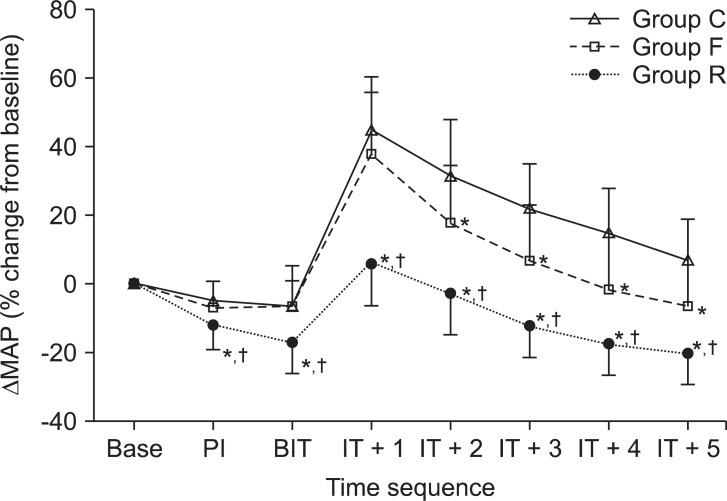
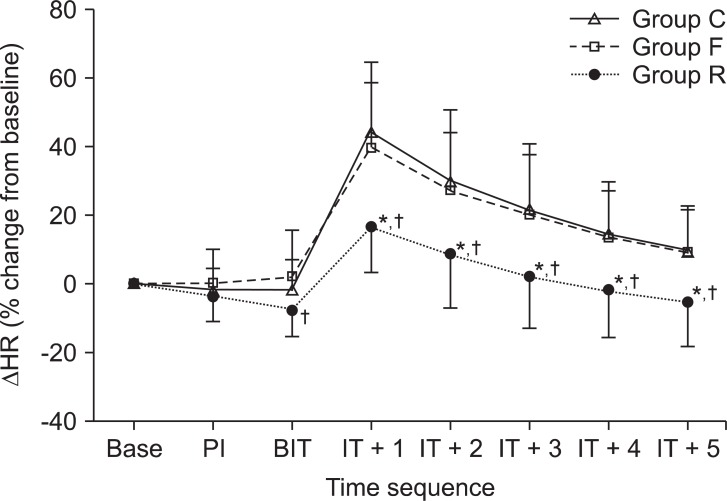
Results
After intubation, group R showed significant decreases compared with groups C and F for all of the hemodynamic variables measured. The incidences of increases in SBP and HR of more than 30% of the baseline levels, SBP of > 200 mmHg, and HR of > 120 beats/min were significantly lower in group R (0%, 10%, 0%, and 0%, respectively) compared with groups C (83%, 83%, 30%, and 13%, respectively) and F (63%, 77%, 13%, and 7%, respectively). The frequency and intensity of myoclonus were significantly decreased in both groups F and R compared with group C.
Conclusions
Pretreatment with remifentanil suppressed cardiovascular reactions to endotracheal intubation more effectively than that of fentanyl during etomidate induction. Both opioids reduced the incidence of myoclonus.
Keywords: Endotracheal intubation, Etomidate, Fentanyl, Remifentanil
Introduction
Elderly patients are at a high risk of experiencing complications caused by hemodynamic changes after endotracheal intubation. Their high risk results from the high prevalence of cardiovascular diseases in the elderly population, the difficulty in recognizing the diseases due to their atypical presentation, as well as the low physiological reserve, pharmacodynamic and pharmacokinetic changes, and autonomic nervous system changes noted in this population [
1]. Therefore, such underlying diseases and physiological differences should be considered when choosing an anesthetic regimen for elderly patients.
Etomidate is frequently used as an anesthesia-inducing drug because of its fast onset of induction and recovery. It also provides cardiovascular stability, leads to minor respiratory suppression, protects the brain, and induces smaller amounts of histamine secretion [
2,
3]. However, its suppression of laryngopharyngeal reflexes during endotracheal intubation is insufficient [
4]. Thus, etomidate has a stable hemodynamic profile after induction, but hypertension and tachycardia are frequent after intubation. It is also associated with myoclonus after injection as well as adrenal suppression, postoperative nausea and vomiting, and pain upon injection. Myoclonus, which increases in proportion with the dose of etomidate administered, may occur in 50-80% of unpremedicated patients [
2]. This condition can be a serious problem in non-fasting emergency conditions, in patients with open eye injuries, or in those with limited cardiovascular reserve [
5].
The occurrences of myoclonus and hemodynamic changes after endotracheal intubation can be reduced by pretreatment with opioids. Previous studies have reported that fentanyl or alfentanil reduced the development of myoclonus and hemodynamic changes after endotracheal intubation in elderly patients with etomidate induction [
6,
7]. However, few studies describe the effects of the concomitant administration of remifentanil with etomidate.
Thus, this study investigated whether the administration of a small dose of etomidate resulted in a stable hemodynamic profile during an anesthetic induction, and compared the effects of pretreated fentanyl to remifentanil on hemodynamic changes after endotracheal intubation and the occurrence of myoclonus in elderly patients with etomidate induction.
Materials and Methods
The participants in this study included 90 patients aged 65 years and over who required tracheal intubation with American Society of Anesthesiologists physical status I or II undergoing elective surgery; informed consent was obtained from the patients prior to enrollment. Patients with histories of hypertension, diabetes mellitus, myocardial infarction, or congestive heart failure were excluded. Those who showed conduction block on an electrocardiogram, or who required excessive manipulations or repeated attempts to achieve tracheal intubation were also excluded. Patients were randomly assigned to a control (n = 30, group C), a fentanyl (n = 30, group F), or a remifentanil group (n = 30, group R) by having patients picking one of 90 cards marked C, F, or R from a closed box. All of the patients fasted from midnight, and were not premedicated in order to avoid pharmacodynamic and pharmacokinetic drug interactions.
The patients were assessed using an electrocardiograph, a non-invasive hemadynamometer, a pulse oximeter, and a bispectral index (BIS) monitor. Anesthesia was induced after ensuring that the blood pressure and heart rate were constant when measured at least 3 times. While supplying 100% oxygen at 5 L/min for 1-2 min through a mask, 0.2 mg/kg of etomidate (Etomidate-Lipuro, B. Braun Melsungen AG, Germany) was injected over 20 s intravenously.
Approximately 1 min before the injection of etomidate, and 3 min before endotracheal intubation, 10 ml of saline was injected into the patients in group C. In group F, 1.0 µg/kg of fentanyl was injected over 30 s, whereas in group R, 1.0 µg/kg of remifentanil was injected over 30 s, followed by continuous infusion at 0.1 µg/kg/min. When the patients became unreactive to oral orders, their eyelash reflex disappeared, and the BIS index was less than 50, 0.8 mg/kg of rocuronium was administered. After 2 min, endotracheal intubation was performed by a skilled anesthesiologist. Sevoflurane was adjusted to achieve BIS value of 45-60 with 50% nitrous oxide in oxygen. Mechanical ventilation was applied to maintain end-expiratory carbon dioxide concentrations at 35-40 mmHg.
When myoclonus occurred, its onset and intensity were recorded by a trained nurse who was blind to the pretreated solution. The intensity measurement grades were as follows: 1, no movement; 2, mild (involuntary movement in a small unit of the muscle group); 3, moderate (movement in a large unit of the muscle group or in 2 muscle groups, or a mild generalized response); and 4, severe (generalized response or intense movement in 2 or more muscle groups).
Systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial blood pressure (MAP), heart rate (HR), and BIS index were measured and recorded before induction (BASE), post-induction (PI), before intubation (BIT), and at each min for 5 min after intubation (IT + 1, IT + 2, IT + 3, IT + 4, and IT + 5). The percent change in hemodynamic data ([measuring value-baseline]/baseline × 100%) for each patient was calculated during the observation period. The number of patients who experienced excessive hemodynamic changes was noted based on the following criteria: an increase or decrease in SBP or HR of more than 30% of the baseline level; an SBP of <90 or >200 mm Hg; or a HR of <50 or >120 beats/min.
All measured values are reported as mean ± standard deviation (SD) and were statistically analyzed using SPSS (version 12.0, SPSS Inc., Chicago, USA). The demographic data of the groups (i.e., age, weight, and height) were analyzed using oneway ANOVA, whereas gender was analyzed using the chi-square test. The differences in the cardiovascular variables among the groups were analyzed by one-way ANOVA and Scheffe's post hoc test. Discrete data were analyzed using either the chi-square test or Fisher's exact test, as appropriate. A P value of less than 0.05 was judged to be statistically significant.
Results
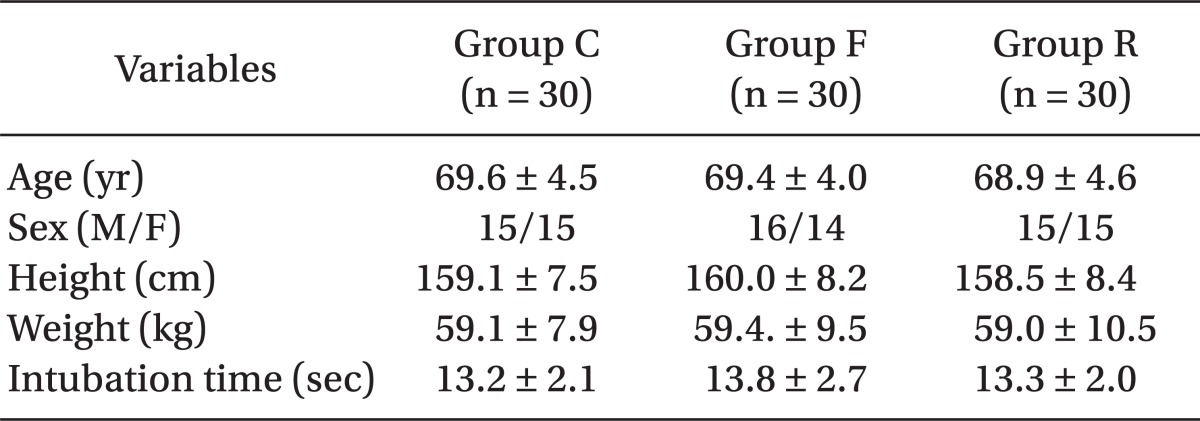
Endotracheal intubation was performed successfully in all patients without any complications. The age, sex, height, and weight of the patients, as well as the time taken for endotracheal intubation were not significantly different among the groups (
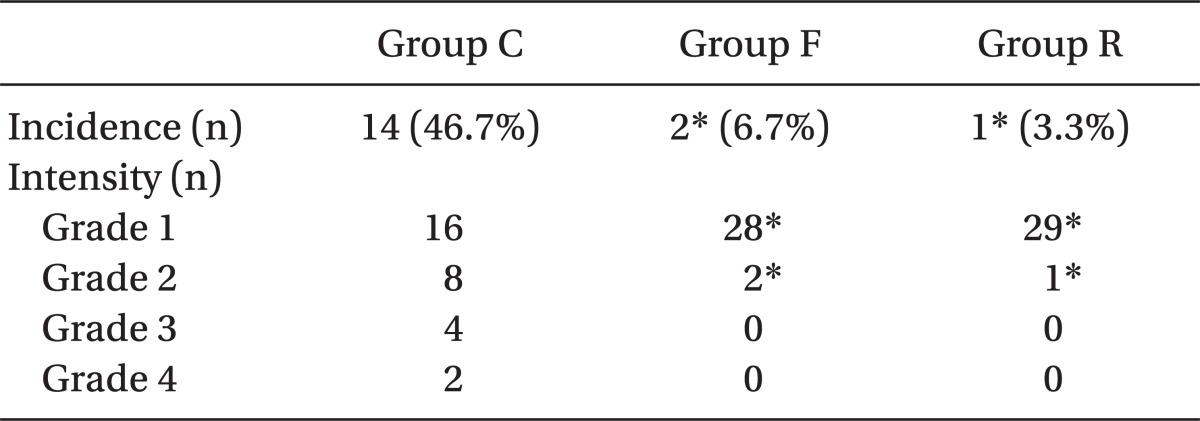
Table 1). The frequency and intensity of myoclonus events were significantly decreased in both groups F and R compared with the saline group (P < 0.05,
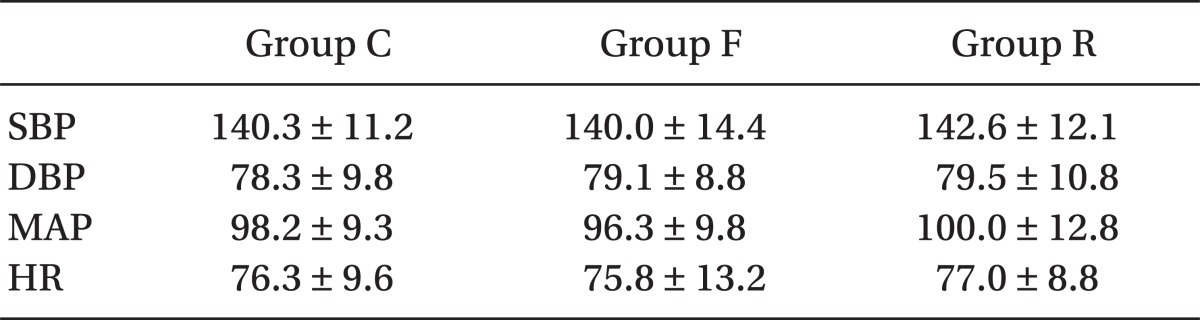
Table 2). However, these values in group C and R were not significantly different. The basal values of the patients for SBP, DBP, MAP, and HR were not significantly different among the groups (
Table 3). The BIS index values were not significantly different among the groups during the observation period, either.
After induction and before intubation, the ΔSBP, ΔDBP, and ΔMAP were significantly decreased in group R compared with groups C and F (P < 0.05). These values in Group F were not significantly different from those in group C until the period before intubation. These measured variables in group F were not significantly different from those in group C at 1 min after intubation. By 2 min after intubation, ΔSBP, ΔDBP, and ΔMAP were significantly decreased in group F compared with group C (P < 0.05). ΔHR was not significantly different in group F compared with group C (P < 0.05). After intubation, group R showed significant decreases compared with groups C and F for all of the hemodynamic variables measured (P < 0.05) (
Fig. 1-
4).
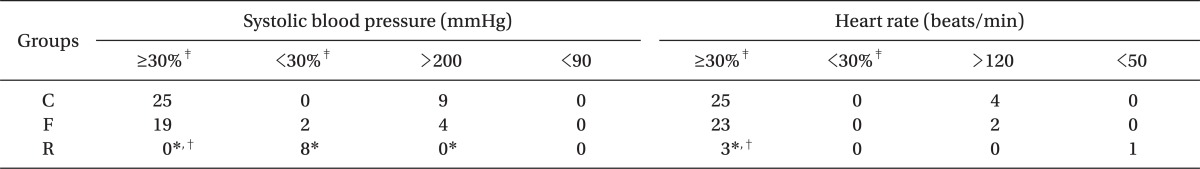
The number of patients who experienced excessive hemodynamic changes is shown in
Table 4. The incidences of increases in SBP and HR of more than 30% of the baseline levels, SBP of >200 mmHg, and HR of >120 beats/min were significantly lower in group R (0%, 10%, 0%, and 0%, respectively) compared with groups C (83%, 83%, 30%, and 13%, respectively) and F (63%, 77%, 13%, and 7%, respectively) (P < 0.01). No significant differences were observed for any comparisons between groups C and F.
With regards to the opioid injection side effects, neither chest wall rigidity nor postoperative respiratory discomfort occurred in any of the patients.
Discussion
This study examines whether a small dose of etomidate can provide a stable anesthetic induction in elderly patients. It also compares the effects of fentanyl 1.0 µg/kg and remifentanil 1.0 µg/kg followed by a continuous infusion of remifentanil 1.0 µg/kg/min on hemodynamic reactions to endotracheal intubation and on reduction of the myoclonus. Based on the results of this study, 0.2 mg/kg of etomidate with remifentanil 1.0 µg/kg followed by a continuous infusion of remifentanil 1.0 µg/kg/min may be suitable for anesthetic induction in elderly patients. Remifentanil reduced the development of myoclonus and suppressed cardiovascular reactions to endotracheal intubation. Fentanyl reduced the development of myoclonus as well, but it did not attenuate hemodynamic response due to endotracheal intubation. However, it shows a tendency to reduce the increased rate of cardiovascular reactions.
Myoclonus is one of the most notable side effects of etomidate induction. The incidence of myoclonus is approximately 50-80% for patients who are not premedicated. It is a serious problem in non-fasting emergency conditions or in patients with open-globe injury because it can lead to a vitreous prolapse as a result of high intraocular pressure [
8]. To prevent the development of myoclonus, pretreatment with benzodiazepine, magnesium sulfate and opioids were used. Guler et al. [
9] reported that 2.248 mmol of magnesium sulfate effectively reduced etomidate-induced myoclonus. Helmers et al. [
10] reported that 5 mg of droperidol and 100 µg of fentanyl significantly decreased the incidence of myoclonus. In our study, incidences of myoclonus were 3.3%, 6.7% and 46.7% in cases of using remifentanil, fentanyl and normal saline, respectively. This is consistent with the results of the study by Kelsaka et al. [
8]. However, in the case of normal saline, incidence of myoclonus was slightly lower than that of other studies [
5,
9,
11]. It takes into consideration that the ages of the patients of our study were greater than 65 years and the dosage of etomidate, 0.2 mg/kg, was the minimum quantity.
Etomidate does not reduce myocardial contractility [
3] and acts as an alpha 2B-receptor agonist [
12]. This ensures very high hemodynamic stability during anesthesia induction. On the other hand, propofol, which is commonly used as an anesthesia induction agent, frequently triggers hypotension during anesthesia induction and reduces myocardial contractility and systemic vascular resistance [
13]. However, etomidate cannot mitigate a sympathetic response to endotracheal intubation because it lacks analgesic efficacy [
14,
15]. In our study, signs of hemodynamic suppression, such as hypotension and bradycardia, did not appear. Heart rate and blood pressure were stably maintained after injecting etomidate in all the patients but a tendency for an increase in heart rate and blood pressure was observed in all the patients after the endotracheal intubation. In particular, the rates of increase were higher in the control group where an opioid was not used in combination with etomidate. This is consistent with the results of many studies, which indicate that if etomidate is used alone, hemodynamic changes caused by endotracheal intubation will be difficult to suppress [
15,
16].
To prevent these reactions of the cardiovascular system, such as hypertension or tachycardia, caused by endotracheal intubation and to maintain hemodynamic stability, the intravenous injection or spraying of lidocaine, the administration of inhalation anesthetics, the intravenous injection of beta blockers and calcium channel blockers, and the administration of nitroglycerin or opioids have been conducted [
17]. In particular, opioids can effectively suppress the reactions of the cardiovascular system to laryngoscopy and endotracheal intubation by increasing the depth of anesthesia and blocking the reactions of the sympathetic nervous system. Dahlgren and Messeter [
18] reported that the bolus of fentanyl 5 µg/kg before an anesthesia induction effectively suppressed hemodynamic reactions to laryngoscopy and endotracheal intubation. In a study by Kautto [
19], 2 and 6 µg/kg of fentanyl were administered. The hemodynamic reactions to endotracheal intubation were remarkably suppressed in the 2 µg/kg and completely abolished in the 6 µg/kg group. In addition, Weiss-Bloom and Reich [
20] suggested that administering fentanyl 5-10 µg/kg during anesthesia induction using etomidate could prevent hemodynamic reactions to endotracheal intubation. However, large amounts of fentanyl may cause thoracic spasticity, postoperative hypoventilation or hypotension after anesthesia induction [
21]. Since elderly patients have relatively high plasma drug concentrations by reduced systemic clearance [
22], reduced doses of fentanyl should be administered. In a study where thiopentone and fentanyl 3 µg/kg had been administered to 16 patients, Chung and Evans [
22] reported that respiratory suppression occurred in three of the 16 patients and thus naloxone had been administered. In a study where thiopentone and fentanyl 1.5 µg/kg had been administered to elderly patients, Splinter and Cervenko [
23] reported that hypotension had occurred in 33% of the patients. In this study, fentanyl 1.0 µg/kg was used in order to avoid these side effects; no thoracic spasticity, postoperative hypoventilation or hypotension after anesthesia induction occurred in any of the patients. However, excessive blood pressure elevation and tachycardia after endotracheal intubation could not be prevented.
Hemodynamic changes were effectively suppressed only in the remifentanil group in our study. This is consistent with the results of a study by Zhang and Sun [
24]. Habib et al. [
25] reported that the administration of remifentanil 0.5 µg/kg followed by its continuous infusion at 0.1 µg/kg/min in elderly patients effectively suppressed hemodynamic reactions to laryngoscopy and endotracheal intubation. Casati et al. [
26] reported that the administration of remifentanil 1 µg/kg followed by a continuous infusion at 0.1 µg/kg/min effectively suppressed cardiovascular changes caused by endotracheal intubation.
However, there have been a few studies conducted on the appropriate dosage of remifentanil that can suppress cardiovascular reactions to endotracheal intubation during anesthesia induction using etomidate. Zhang and Sun [
24] reported that the bolus injection of remifentanil 1 µg/kg followed by a continuous infusion at 0.1 µg/kg/min was effective in blunting the cardiovascular response to endotracheal intubation. Kelsaka et al. [
8] reported that pretreatment with remifentanil 1 µg/kg reduced myoclonus after etomidate induction without side effects. The doses of remifentanil used in our study were determined based on these reports. Besides, since the relative potency of fentanyl and remifentanil are 1 : 1 [
27,
28], it can be concluded that the two doses of opioid used in our study had equal potency. However, since the action duration of fentanyl was as long as 30-60 min but the context sensitive half time of remifentanil was as short as 3 min, a single bolus injection of remifentanil alone could not maintain an effective blood concentration until some time had passed after endotracheal intubation. Therefore, remifentanil was infused continuously to maintain an effective blood concentration.
In this study, a non-invasive method was used to measure blood pressure. Since this method takes around 20-30 seconds to measure the blood pressure, it has a disadvantage of not being able to detect the changes in blood pressure immediately. However, if an invasive arterial catheter is installed to measure the immediate changes in blood pressure, the catheter itself will trigger an increase in plasma catecholamine concentration, which may affect the hemodynamic values. More discussion and studies on the different methods and their effects are necessary to accurately measure blood pressure.
In conclusion, it can be stated that the administration of remifentanil 1 µg/kg followed by its continuous infusion at 0.1 µg/kg/min may enable a stable anesthetic induction and an endotracheal intubation without excessive hemodynamic change during an induction of a small dose of etomidate in elderly patients. Also, it may more effectively suppress the laryngopharyngeal reflex due to endotracheal intubation than the administration of fentanyl 1 µg/kg can. It may be also said that the pretreatment of patients with fentanyl and remifentanil reduced the development of myoclonus, and their effects on myoclonus were the same.
Acknowledgments
This study was supported by research funds from Dong-A University.
References
1. Beliveau MM, Multach M. Perioperative care for the elderly patient. Med Clin North Am. 2003; 87:273–289. PMID:
12575895.

2. Ostwald P, Doenicke AW. Etomidate revisited. Curr Opin Anaesthesiol. 1998; 11:391–398. PMID:
17013247.

3. Bergen JM, Smith DC. A review of etomidate for rapid sequence intubation in the emergency department. J Emerg Med. 1997; 15:221–230. PMID:
9144065.

4. Erhan E, Ugur G, Gunusen I, Alper I, Ozyar B. Propofol - not thiopental or etomidate - with remifentanil provides adequate intubating conditions in the absence of neuromuscular blockade. Can J Anaesth. 2003; 50:108–115. PMID:
12560298.

5. Hueter L, Schwarzkopf K, Simon M, Bredle D, Fritz H. Pretreatment with sufentanil reduces myoclonus after etomidate. Acta Anaesthesiol Scand. 2003; 47:482–484. PMID:
12694150.

6. Stockham RJ, Stanley TH, Pace NL, Gillmor S, Groen F, Hilkens P. Fentanyl pretreatment modifies anaesthetic induction with etomidate. Anaesth Intensive Care. 1988; 16:171–176. PMID:
3394909.
7. Cho SY, Jeon WJ, Nam YM, Yeom JH, Kim KH. The optimal dosage of alfentanil pretreatment for prevention of myoclonus after injection of etomidate. Korean J Anesthesiol. 2008; 55:320–325.

8. Kelsaka E, Karakaya D, Sarihasan B, Baris S. Remifentanil pretreatment reduces myoclonus after etomidate. J Clin Anesth. 2006; 18:83–86. PMID:
16563323.

9. Guler A, Satilmis T, Akinci SB, Celebioglu B, Kanbak M. Magnesium sulfate pretreatment reduces myoclonus after etomidate. Anesth Analg. 2005; 101:705–709. PMID:
16115978.

10. Helmers JH, Adam AA, Giezen J. Pain and myoclonus during induction with etomidate. A double-blind, controlled evaluation of the influence of droperidol and fentanyl. Acta Anaesthesiol Belg. 1981; 32:141–147. PMID:
7027723.
11. Lee SW, Gill HJ, Park SC, Kim JY, Kim JH, Lee JY, et al. The effect of remifentanil for reducing myoclonus during induction of anesthesia with etomidate. Korean J Anesthesiol. 2009; 57:438–443.

12. Paris A, Philipp M, Tonner PH, Steinfath M, Lohse M, Scholz J, et al. Activation of alpha 2B-adrenoceptors mediates the cardiovascular effects of etomidate. Anesthesiology. 2003; 99:889–895. PMID:
14508322.
13. Ebert TJ, Muzi M, Berens R, Goff D, Kampine JP. Sympathetic response to induction of anesthesia in humans with propofol or etomidate. Anesthesiology. 1992; 76:725–733. PMID:
1575340.
14. Nauta J, Stanley TH, de Lange S, Koopman D, Spierdijk J, van Kleef J. Anaesthetic induction with alfentanil: comparison with thiopental, midazolam, and etomidate. Can Anaesth Soc J. 1983; 30:53–60. PMID:
6402282.

15. Giese JL, Stockham RJ, Stanley TH, Pace NL, Nelissen RH. Etomidate versus thiopental for induction of anesthesia. Anesth Analg. 1985; 64:871–876. PMID:
4025853.

16. Harris CE, Murray AM, Anderson JM, Grounds RM, Morgan M. Effects of thiopentone, etomidate and propofol on the haemodynamic response to tracheal intubation. Anaesthesia. 1988; 43:32–36. PMID:
3259093.

17. Kovac AL. Controlling the hemodynamic response to laryngoscopy and endotracheal intubation. J Clin Anesth. 1996; 8:63–79. PMID:
8695083.

18. Dahlgren N, Messeter K. Treatment of stress response to laryngoscopy and intubation with fentanyl. Anaesthesia. 1981; 36:1022–1026. PMID:
7032347.

19. Kautto UM. Attenuation of the circulatory response to laryngoscopy and intubation by fentanyl. Acta Anaesthesiol Scand. 1982; 26:217–221. PMID:
7113629.

20. Weiss-Bloom LJ, Reich DL. Haemodynamic responses to tracheal intubation following etomidate and fentanyl for anaesthetic induction. Can J Anaesth. 1992; 39:780–785. PMID:
1288902.

21. White PF. Textbook of intravenous anesthesia. 1997. Baltimore: Williams & Wilkins;p. 212–218.
22. Chung F, Evans D. Low-dose fentanyl: haemodynamic response during induction and intubation in geriatric patients. Can Anaesth Soc J. 1985; 32:622–628. PMID:
3907792.

23. Splinter WM, Cervenko F. Haemodynamic responses to laryngoscopy and tracheal intubation in geriatric patients: effects of fentanyl, lidocaine and thiopentone. Can J Anaesth. 1989; 36:370–376. PMID:
2758537.

24. Zhang GH, Sun L. Peri-intubation hemodynamic changes during low dose fentanyl, remifentanil and sufentanil combined with etomidate for anesthetic induction. Chin Med J (Engl). 2009; 122:2330–2334. PMID:
20079135.
25. Habib AS, Parker JL, Maguire AM, Rowbotham DJ, Thompson JP. Effects of remifentanil and alfentanil on the cardiovascular responses to induction of anaesthesia and tracheal intubation in the elderly. Br J Anaesth. 2002; 88:430–433. PMID:
11990278.

26. Casati A, Fanelli G, Albertin A, Deni F, Danelli G, Grifoni F, et al. Small doses of remifentanil or sufentanil for blunting cardiovascular changes induced by tracheal intubation: a double-blind comparison. Eur J Anaesthesiol. 2001; 18:108–112. PMID:
11270019.

27. Glass PS. Remifentanil: a new opioid. J Clin Anesth. 1995; 7:558–563. PMID:
8652166.

28. McEwan AI, Smith C, Dyar O, Goodman D, Smith LR, Glass PS. Isoflurane minimum alveolar concentration reduction by fentanyl. Anesthesiology. 1993; 78:864–869. PMID:
8489058.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download