Abstract
Background
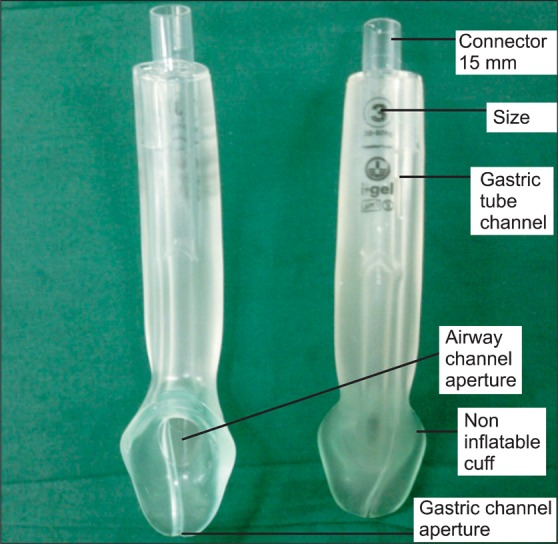
The relatively recently developed I-gel (Intersurgical Ltd., Workingham, England) is a supraglottic airway device designed for single-use that, unlike conventional LMAs, does not require an inflatable cuff. In addition, the I-gel, much like the Proseal LMA (PLMA), has a gastric drainage tube associated with an upper tube for decompression of the stomach, thereby avoiding acid reflux and decreasing the risk of pulmonary absorption. The purpose of this study was to compare PLMA and I-gel devices in patients undergoing gynecological laparoscopy based on sealing pressure before and during pneumoperitoneum, insertion time, and gas exchange.
Methods
Following Institutional Review Board approval and written informed consent, 30 adult patients were randomly allocated to one of two groups (the PLMA or I-gel group). In each case, insertion time and number of attempts were recorded. After successful insertion, airway leak pressure was measured.
Results
Successful insertion and mechanical ventilation with both supraglottic airway devices was achieved on the first attempt in all 30 patients, and there were no significant differences with respect to insertion time. Likewise, leak pressure did not vary significantly either between or within groups after CO2 insufflation. In addition, differences between leak volume and leak fraction between groups were not significant.
The relatively recently developed I-gel (Intersurgical Ltd., Workingham, England) (Fig. 1) is a device intended for single-use in which cuff is not used [1], instead of it I-gel utilizes a thermoplastic elastomer (styrene butadiene styrene ethylene) to create a more intimate interface for interaction with the supraglottic tissue. Like the Proseal LMA (PLMA), I-gel has a gastric drainage tube integrated to the upper tube for stomach decompression, which significantly reduces risk of acid reflux and pulmonary aspiration [2]. I-gel has a semi-rigid stem to aid with insertion and prevents kinking and also has an intrinsic bite block to prevent compression of the airway tube and prevent misplacement in the mouth and axial rotation [2,3]. Several studies have shown that I-gel exhibits higher sealing pressure [4], ease of insertion and reduced trauma [5,6] compared with the LMA-Classic. For laparoscopic surgery, several studies have reported the safety and successful insertion of LMA [7,8].
Recent studies show that the I-gel provides a good seal during anesthesia for spontaneously breathing and for controlled ventilation [1,4,9]. However, there are no studies performed which have compared its performance with PLA for laparoscopic surgery.
Our study was primarily aimed at evaluating the use of I-gel as alternative to the PLMA for sealing adequacy before and during pneumoperitoneum for laparoscopic gynecologic surgery. Second, the insertion time, number of attempts, and respiratory mechanics were compared before and during pneumoperitoneum.
Patient enrollment and subsequent experimental procedures were performed with approval from the Institutional Review Board on Human Subjects Research and Ethics Committee and after obtaining written informed consent from patients. We enrolled a total of 30 women judged to be at American Society of Anesthesiologists physical status 1 or 2, aged 18-65 years, and undergoing laparoscopic gynecologic operation. Patients with the following were excluded from the study: obese (body mass index more than 35 kg/m2), pregnancy, gastric reflux, and/or suspected airway difficulty (Mallampati score 3 or 4, mouth opening less than 2.5 cm). The attending anesthesiologist recorded patient demographics and measured Mallampati score preoperatively.
Enrolled patients were randomly allocated into PLMA or I-gel groups using computer-generated numbers. In the operating room before surgery, the usual monitoring occurred, which included a Bispectral Index (BIS; Aspect Medical Systems, Newton, MA, USA) sensor. The following baseline data were recorded: heart rate, noninvasive blood pressure, oxyhemoglobin saturation, and BIS.
Prior to induction, all patients assumed a neutral position, and IV access was secured. After preoxygenation of the lungs with 6 L/min, using Orchestra® Base Primea (Fresenius Kabi, Brezins, France) as the infusion equipment, total intravenous anesthesia was performed.
Once patients' full muscle relaxation was achieved using rocuronium 0.6 mg/kg intravenously, the selected airway device (PLMA or I-gel) was inserted by a single user (S.C) per the manufacturer's instructions based on patient size. Size selection of the I-gel depended on patient weight (weight < 50 kg: I-gel size 3; 50-90 kg: size 4; and > 70 kg: size 5). Size selection of the PLMA is identical to classic LMA (weight 30-50 kg: size 3; 50-70 kg: size 4; 70-100 kg: size 5). Insertion of PLMA was performed without an introducer; the index finger of operator was placed in the retaining strap.
The PLMA was pressed against the hard palate and advanced into the hypopharynx until resistance was felt. After PLMA placement, the cuff was inflated. A defined volume of air was used; the cuff pressure was set to 60 cmH2O. (Maximum cuff inflation volume; size 3: 20 ml; size 4: 30 ml; size 5: 40 ml) After insertion of the breathing apparatus and subsequent connection to the ventilation system, correct positioning of it was confirmed by visualizing verification of insertion with visualization of three expiratory carbon dioxide square waveforms and movements of chest wall during mechanical ventilation and a leak pressure greater than 20 cmH2O. During surgery rocuronium was used to achieve neuromuscular block, which was verified with a peripheral nerve stimulator. At the end of the surgery, pyridostigmine 0.2 mg/kg and glycopyrrolate 0.008 mg/kg was used to reverse the effects of rocuronium. In all experimental cases, the time required for insertion and the number of attempts was obtained. The insertion time of the device was defined as the time between grabbing the device until visualization of 3 expiratory CO2 waveforms. If the first attempt at insertion was deemed a failure according to the anesthesiologist's judgment, the next try was made via either a jaw thrust maneuver or a change in head position. When and if a third attempt was necessary, a different device size was utilized. Upon failure of third line approaches, additional devices were utilized based on the attending anesthesiologist's preference.
Oropharyngeal leak pressure was determined by closing the expiratory valve of the circle system at a fixed gas flow of 3 L/min and noting the airway pressure (maximum allowed was 40 cm H2O) at which equilibrium was reached [10].
In both groups, 10 min after insertion (T1) and 15 min after carbon dioxide pneumoperitoneum (T2), measurement of vital signs and changes to airway pressure were observed and recorded. In both groups, a carbon dioxide pneumoperitoneum was induced with a maximal intraabdominal pressure of 15 mmHg. The Ppeak, leak pressure, mean airway pressure, compliance and airway resistance were measured by spirometry via an Avance station (Datex-Ohmeda, WI, USA) during measurement time.
We labeled the gap between the inspired versus the expired tidal volume as 'leak volume' and measured it at T1 and T2. The leak fraction was calculated as the leak volume divided by inspired tidal volume at T1 and T2.
We performed a pilot study with 10 patients from the PLMA group to assess the size of our study. The mean value of leak pressure was 26.7 cmH2O, standard deviations were 4.9 cmH20. For our power calculation, we assumed equal standard deviation for both groups. To sense a difference of 5.4 cmH20 between the 2 groups with a two-tailed α = 0.05 and a power of 80%, a minimum of 13 per group were needed. A Z-test was performed to prove the lack of difference between the 2 groups. Therefore, we decided to recruit 30 patients to allow for a drop rate of 10%.
Data were expressed as the median and interquartile range or as categorical distributions. Statistical analyses were performed using the Statistical Package for Social Sciences software (SPSS 12.0 for Windows; SPSS Inc., IL, USA) and SigmaStat (SIGMASTAT 3.1; Systat Software, Inc., CA, USA). The Mann-Whitney rank sum test was used to compare and analyze the numerical data between the 2 groups. The Kruskal-Wallis one way analysis of variance was used for hemodynamic data, with a Dunn multiple comparison tests for inter-group comparison. Significance was assumed at P < 0.05.
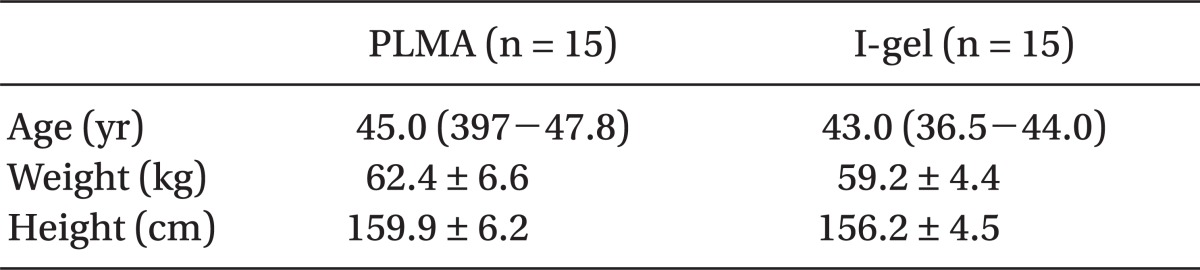
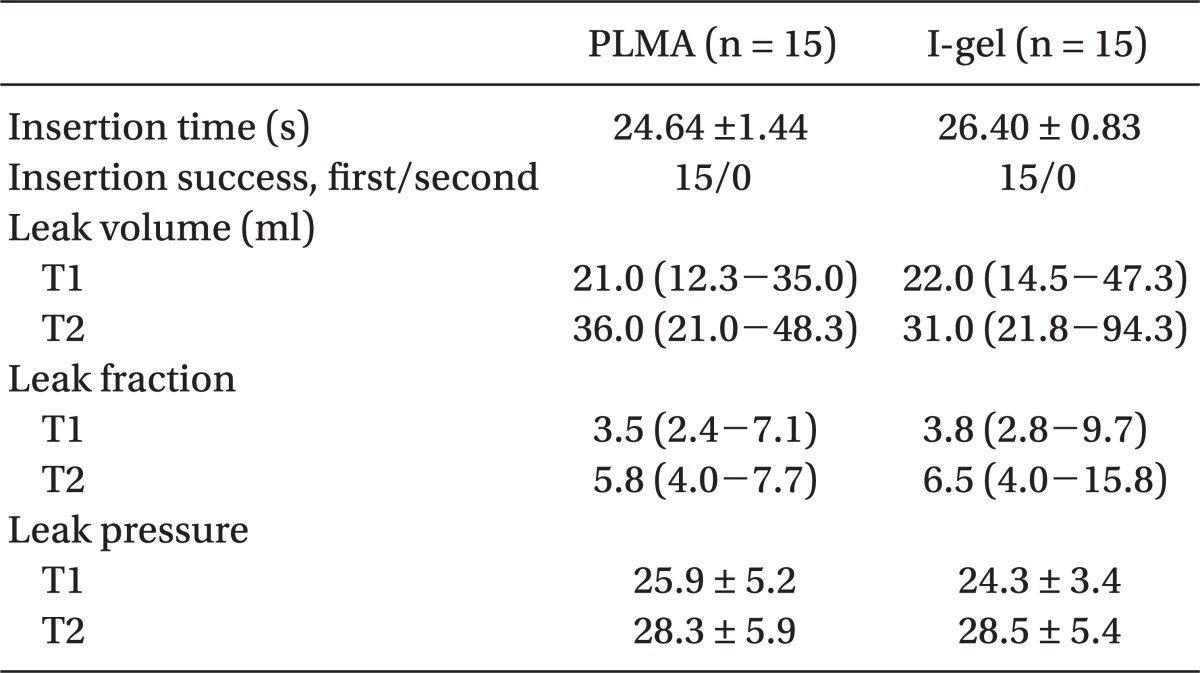
Demographic data between groups were statistically insignificant (Table 1). Likewise, leak pressure after CO2 insufflation did not differ significantly between or within groups (Table 2). The differences in leak volume and leak fraction were insignificant between the groups.
Successful insertion and mechanical ventilation of both devices was achieved on the first attempt in all 30 patients, and the time to insertion was similar (26.4 ± 1.4 and 26.4 ± 0.8 for PLMA and I-gel, respectively).
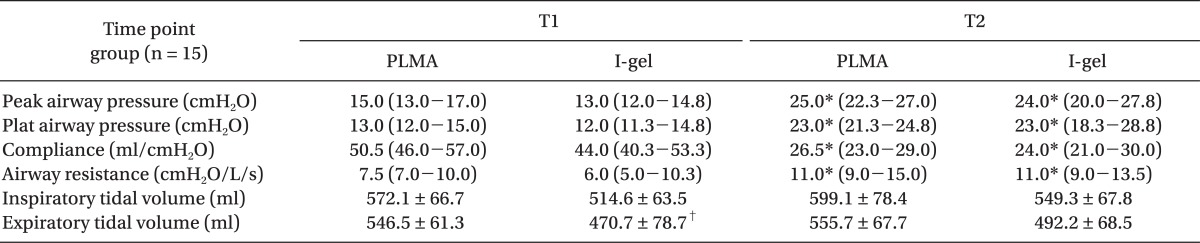
Differences between groups of the peak airway pressures and plateau airway pressures were insignificant (Table 3). In both groups the Ppeak 15 min after CO2 insufflation increased substantially compared to baseline values (P < 0.01). Compliance at T1 did not differ between groups, and compliance in both groups 15 min after the formation of pneumoperitoneum (T2) was significantly decreased compared to that at T1 (P < 0.01). Inspiratory tidal volume of both groups did not differ over time; however, the expiratory tidal volume of the I-gel group at T1 was smaller than that of the PLMA group (P < 0.05).
Based on the results of our study, the leak airway pressures of the I-gel group and the PLMA group were almost identical with respect to pneumoperitoneum during laparoscopic gynecologic surgery. Furthermore, the total insertion times and number of attempts for both devices were not significantly different.
The cuff of the I-gel was made to produce a sealing device that does not need inflation to fit the perilaryngeal anatomy [1]. In a study comparing an LMA and the I-gel, airway leak pressures were similar between the devices [2]. Another study comparing the I-gel with the LMA-Unique showed that leak pressure was significantly higher in the I-gel group and this higher airway leak pressure indicated better seal and I-gel was alternative to the LMA-Unique for mechanical ventilation [4]. Using a cadaver model, Schmidbauer et al. [11] demonstrated that both the PLMA and cLMA made a tighter seal than the I-gel. The PLMA is designed to improve controlled ventilation, airway protection and diagnosis of displacement. Cook et al. [12] concluded that PLMA offered significant benefits over classic LMA and tracheal tube in some circumstances including laparoscopic gynecologic surgery. In the present study, we showed that leak airway pressures 10 min after insertion were similar between PLMA and the I-gel (25.9 ± 5.2 and 24.3 ± 3.4 cmH2O, respectively). Further, leak pressure did not vary significantly between or within groups 15 min after CO2 insufflation (28.3 ± 5.9 vs 28.5 ± 5.4, respectively). In addition, leak volumes and leak fractions of these devices before and after CO2 insufflation were not statistically significantly different. The similarities in airway leak pressures, leak volumes and leak fractions demonstrated that both devices sealed equivalently and protected airway effectively.
Successful insertion and ventilation of both devices were achieved on the first attempt in all patients. Median time to insertion using the PLMA and I-gel was 26.0 sec and 27.0 sec, respectively, this data is similar to other data [2,11]. In addition, the insertion times for the 2 devices were not statistically significantly different. Initially, we thought that that insertion of I-gel would be easier than PLMA due to the absence of a cuff and no requirement of air insufflation. However, insertion time in both devices did not differ.
Several manuscripts have reported safe and successful use of LMA-Classic devices in patients undergoing laparoscopic surgery [7,8]. Likewise, other devices, such as the PLMA, have been investigated and provided effective mechanical ventilation and have been used safely during laparoscopic surgery [13,14]. In the present study, we did not find gastric insufflation, regurgitation, or gastric aspiration during surgery in either group.
The first limitation of our study was instrument selection bias by the anesthesiologist, which was not possible to eliminate, because the anesthesiologist was aware of the device he was using due to the difference in shape between the devices. Second, all insertions were performed by an experienced anesthesiologist; therefore, our results may not be applicable to novice users. Finally, patients enrolled in our study had normal airways; thus, no conclusions can be made regarding patients for whom difficult intubation is expected.
In conclusion, we demonstrated that sealing effect, insertion time, or first-time insertion success rate of PLMA versus I-gel was insignificant. We conclude that the I-gel provides a reliable alternative to the PLMA for positive pressure ventilation during laparoscopic gynecologic surgery without severe complications.
References
1. Uppal V, Gangaiah S, Fletcher G, Kinsella J. Randomized crossover comparison between the i-gel and the LMA-Unique in anaesthetized, paralysed adults. Br J Anaesth. 2009; 103:882–885. PMID: 19846406.

2. Cattano D, Ferrario L, Maddukuri V, Sridhar S, Khalil Y, Hagberg CA. A randomized clinical comparison of the Intersurgical i-gel and LMA Unique in non-obese adults during general surgery. Minerva Anestesiol. 2011; 77:292–297. PMID: 21364502.
3. Wharton NM, Gibbison B, Gabbott DA, Haslam GM, Muchatuta N, Cook TM. I-gel insertion by novices in manikins and patients. Anaesthesia. 2008; 63:991–995. PMID: 18557971.

4. Francksen H, Renner J, Hanss R, Scholz J, Doerges V, Bein B. A comparison of the i-gel with The LMA-Unique™ in non-paralyzed anaesthetized patients. Anaesthesia. 2009; 64:1118–1124. PMID: 19735404.
5. Richez B, Saltel L, Banchereau F, Torrielli R, Cros AM. A new single use supraglottic airway device with a noninflatable cuff and an esophageal vent: an observational study of the i-gel. Anesth Analg. 2008; 106:1137–1139. PMID: 18349185.

6. Gatward JJ, Cook TM, Seller C, Handel J, Simpson T, Vanek V, et al. Evaluation of the size 4 i-gel airway in 100 non-paralyzed patients. Anaesthesia. 2008; 63:1124–1130. PMID: 18616521.
7. Bapat PP, Verghese C. Laryngeal mask airway and the incidence of regurgitation during gynecological laparoscopies. Anesth Analg. 1997; 85:139–143. PMID: 9212137.

8. Jeon WJ, Cho SY, Bang MR, Ko SY. Comparison of volume-controlled and pressure-controlled ventilation using a laryngeal mask airway during gynecological laparoscopy. Korean J Anesthesiol. 2011; 60:167–172. PMID: 21490817.

9. Uppal V, Fletcher G, Kinsella J. Comparison of the i-gel with the cuffed tracheal tube during pressure-controlled ventilation. Br J Anaesth. 2009; 102:264–268. PMID: 19151051.

10. Keller C, Brimacombe JR, Keller K, Morris R. Comparison of four methods for assessing airway sealing pressure with the laryngeal mask airway in adult patients. Br J Anaesth. 1999; 82:286–287. PMID: 10365012.

11. Schmidbauer W, Bercker S, Volk T, Bogusch G, Mager G, Kerner T. Oesophageal seal of the novel supralaryngeal airway device I-Gel™ in comparison with the laryngeal mask airways Classic™ and ProSeal™ using a cadaver model. Br J Anaesth. 2009; 102:135–139. PMID: 19011262.

12. Cook TM, Lee G, Nolan JP. The proseal laryngeal mask airway: a review of the literature. Can J Anaesth. 2005; 52:739–760. PMID: 16103390.
13. Brimacombe J, von Goedecke A, Keller C, Brimacombe L, Brimacombe M. The laryngeal mask airway Unique versus the Soft Seal laryngeal mask: a randomized, crossover study in paralyzed, anesthesized patients. Anesth Analg. 2004; 99:1560–1563. PMID: 15502065.
14. Natalini G, Lanza G, Rosano A, Dell'Agnolo P, Bernardini A. Standard Laryngeal Mask Airway and LMA-Proseal during laparoscopic surgery. J Clin Anesth. 2003; 15:428–432. PMID: 14652119.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download