1. Hirshey Dirksen SJ, Larach MG, Rosenberg H, Brandom BW, Parness J, Lang RS, et al. Future directions in malignant hyperthermia research and patient care. Anesth Analg. 2011; 113:1108–1119. PMID:
21709147.

2. Wappler F. Malignant hyperthermia. Eur J Anaesthesiol. 2001; 18:632–652. PMID:
11553240.

3. Monnier N, Krivosic-Horber R, Payen JF, Kozak-Ribbens G, Nivoche Y, Adnet P, et al. Presence of two different genetic traits in malignant hyperthermia families: implication for genetic analysis, diagnosis, and incidence of malignant hyperthermia susceptibility. Anesthesiology. 2002; 97:1067–1074. PMID:
12411788.
4. Bachand M, Vachon N, Boisvert M, Mayer FM, Chartrand D. Clinical reassessment of malignant hyperthermia in Abitibi-Temiscamingue. Can J Anaesth. 1997; 44:696–701. PMID:
9232296.
5. Wappler F. Anesthesia for patients with a history of malignant hyperthermia. Curr Opin Anaesthesiol. 2010; 23:417–422. PMID:
20173632.

6. Britt BA, Kalow W. Malignant hyperthermia: a statistical review. Can Anaesth Soc J. 1970; 17:293–315. PMID:
4246871.

7. Rosenberg H, Davis M, James D, Pollock N, Stowell K. Malignant hyperthermia. Orphanet J Rare Dis. 2007; 2:21. PMID:
17456235.

8. Larach MG, Gronert GA, Allen GC, Brandom BW, Lehman EB. Clinical presentation, treatment, and complications of malignant hyperthermia in North America from 1987 to 2006. Anesth Analg. 2010; 110:498–507. PMID:
20081135.

9. Rosero EB, Adesanya AO, Timaran CH, Joshi GP. Trends and outcomes of malignant hyperthermia in the United States, 2000 to 2005. Anesthesiology. 2009; 110:89–94. PMID:
19104175.

10. Chamley D, Pollock NA, Stowell KM, Brown RL. Malignant hyperthermia in infancy and identification of a novel RYR1 mutation. Br J Anaesth. 2000; 84:500–504. PMID:
10823104.
11. Ording H. Investigation of malignant hyperthermia susceptibility in Denmark. Dan Med Bull. 1996; 43:111–125. PMID:
8741205.
12. Robinson RL, Curran JL, Ellis FR, Halsall PJ, Hall WJ, Hopkins PM, et al. Multiple interacting gene products may influence susceptibility to malignant hyperthermia. Ann Hum Genet. 2000; 64:307–320. PMID:
11415515.

13. Hernandez JF, Secrest JA, Hill L, McClarty SJ. Scientific advances in the genetic understanding and diagnosis of malignant hyperthermia. J Perianesth Nurs. 2009; 24:19–31. PMID:
19185818.

14. Brady JE, Sun LS, Rosenberg H, Li G. Prevalence of malignant hyperthermia due to anesthesia in New York State, 2001-2005. Anesth Analg. 2009; 109:1162–1166. PMID:
19762744.

15. Iaizzo PA, Klein W, Lehmann-Horn F. Fura-2 detected myoplasmic calcium and its correlation with contracture force in skeletal muscle from normal and malignant hyperthermia susceptible pigs. Pflugers Arch. 1988; 411:648–653. PMID:
3412868.

16. Struk A, Lehmann-Horn F, Melzer W. Voltage-dependent calcium release in human malignant hyperthermia muscle fibers. Biophys J. 1998; 75:2402–2410. PMID:
9788935.

17. Carrier L, Villaz M, Dupont Y. Abnormal rapid Ca
2+ release from sarcoplasmic reticulum of malignant hyperthermia susceptible pigs. Biochim Biophys Acta. 1991; 1064:175–183. PMID:
1645197.
18. Yang T, Allen PD, Pessah IN, Lopez JR. Enhanced excitation-coupled calcium entry in myotubes is associated with expression of RyR1 malignant hyperthermia mutations. J Biol Chem. 2007; 282:37471–37478. PMID:
17942409.

19. Nelson TE, Sweo T. Ca
2+ uptake and Ca
2+ release by skeletal muscle sarcoplasmic reticulum: differing sensitivity to inhalational anesthetics. Anesthesiology. 1988; 69:571–577. PMID:
3177917.
20. Lai FA, Meissner G. The muscle ryanodine receptor and its intrinsic Ca
2+ channel activity. J Bioenerg Biomembr. 1989; 21:227–246. PMID:
2546931.
21. Kim DH, Sreter FA, Ikemoto N. Involvement of the 60 kDa phosphoprotein in the regulation of Ca
2+ release from sarcoplasmic reticulum of normal and malignant hyperthermia susceptible pig muscles. Biochim Biophys Acta. 1988; 945:246–252. PMID:
3191123.
22. Fill M, Coronado R, Mickelson JR, Vilven J, Ma JJ, Jacobson BA, et al. Abnormal ryanodine receptor channels in malignant hyperthermia. Biophys J. 1990; 57:471–475. PMID:
2306496.

23. Nelson TE, Lin M, Volpe P. Evidence for intraluminal Ca
++ regulatory site defect in sarcoplasmic reticulum from malignant hyperthermia pig muscle. J Pharmacol Exp Ther. 1991; 256:645–649. PMID:
1847206.
24. McCarthy TV, Quane KA, Lynch PJ. Ryanodine receptor mutations in malignant hyperthermia and central core disease. Hum Mutat. 2000; 15:410–417. PMID:
10790202.

25. Maclennan DH, Zvaritch E. Mechanistic models for muscle diseases and disorders originating in the sarcoplasmic reticulum. Biochim Biophys Acta. 2011; 1813:948–964. PMID:
21118704.

26. Robinson R, Carpenter D, Shaw MA, Halsall J, Hopkins P. Mutations in RYR1 in malignant hyperthermia and central core disease. Hum Mutat. 2006; 27:977–989. PMID:
16917943.
27. Sambuughin N, Holley H, Muldoon S, Brandom BW, de Bantel AM, Tobin JR, et al. Screening of the entire ryanodine receptor type 1 coding region for sequence variants associated with malignant hyperthermia susceptibility in the north american population. Anesthesiology. 2005; 102:515–521. PMID:
15731587.

28. Brandom BW. Genetics of malignant hyperthermia. Sci World J. 2006; 6:1722–1730.

29. Monnier N, Procaccio V, Stieglitz P, Lunardi J. Malignant-hyperthermia susceptibility is associated with a mutation of the alpha 1-subunit of the human dihydropyridine-sensitive l-type voltage-dependent calcium-channel receptor in skeletal muscle. Am J Hum Genet. 1997; 60:1316–1325. PMID:
9199552.
30. Marchant CL, Ellis FR, Halsall PJ, Hopkins PM, Robinson RL. Mutation analysis of two patients with hypokalemic periodic paralysis and suspected malignant hyperthermia. Muscle Nerve. 2004; 30:114–117. PMID:
15221887.

31. Hopkins PM. Malignant hyperthermia: advances in clinical management and diagnosis. Br J Anaesth. 2000; 85:118–128. PMID:
10928000.
32. Litman RS, Rosenberg H. Malignant hyperthermia: update on susceptibility testing. JAMA. 2005; 293:2918–2924. PMID:
15956637.
33. Iaizzo PA, Kehler CH, Carr RJ, Sessler DI, Belani KG. Prior hypothermia attenuates malignant hyperthermia in susceptible swine. Anesth Analg. 1996; 82:803–809. PMID:
8615501.

34. Levitt RC, Nouri N, Jedlicka AE, McKusick VA, Marks AR, Shutack JG, et al. Evidence for genetic heterogeneity in malignant hyperthermia susceptibility. Genomics. 1991; 11:543–547. PMID:
1774061.

35. Bandschapp O, Girard T. Malignant hyperthermia. Swiss Med Wkly. 2012; 142:w13652. PMID:
22851008.

36. Heffron JJ. Malignant hyperthermia: biochemical aspects of the acute episode. Br J Anaesth. 1988; 60:274–278. PMID:
3279987.

37. Kim DC, Lim HR, Han YJ. Early recognition of malignant hyperthermia with capnography: A case report. Korean J Anesthesiol. 2002; 43:667–672.

38. Tautz TJ, Urwyler A, Antognini JF, Riou B. Case scenario: Increased end-tidal carbon dioxide: a diagnostic dilemma. Anesthesiology. 2010; 112:440–446. PMID:
20068452.
39. Karan SM, Crowl F, Muldoon SM. Malignant hyperthermia masked by capnographic monitoring. Anesth Analg. 1994; 78:590–592. PMID:
8109781.

40. Denborough MA. Anaesthetic deaths in a family (letter). Lancet. 1960; 2:45.
41. Ali SZ, Taguchi A, Rosenberg H. Malignant hyperthermia. Best Pract Res Clin Anaesthesiol. 2003; 17:519–533. PMID:
14661655.

42. Nelson TE. Porcine malignant hyperthermia: critical temperatures for in vivo and in vitro responses. Anesthesiology. 1990; 73:449–454. PMID:
2393129.
43. Sessler DI. Temperature monitoring and perioperative thermoregulation. Anesthesiology. 2008; 109:318–338. PMID:
18648241.

44. Stratman RC, Flynn JD, Hatton KW. Malignant hyperthermia: a pharmacogenetic disorder. Orthopedics. 2009; 32:835. PMID:
19902883.

45. Larach MG, Brandom BW, Allen GC, Gronert GA, Lehman EB. Cardiac arrests and deaths associated with malignant hyperthermia in North America from 1987 to 2006: a report from the north american malignant hyperthermia registry of the malignant hyperthermia association of the United States. Anesthesiology. 2008; 108:603–611. PMID:
18362591.
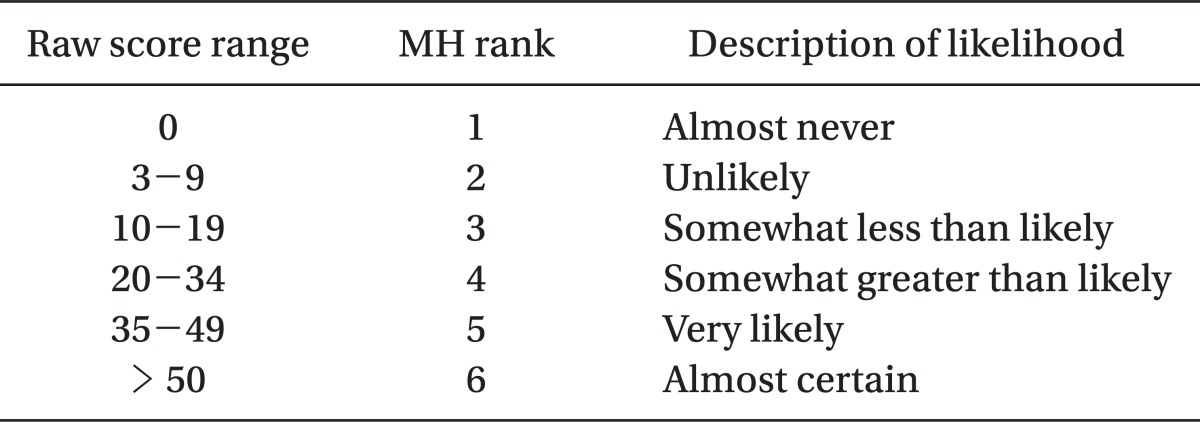
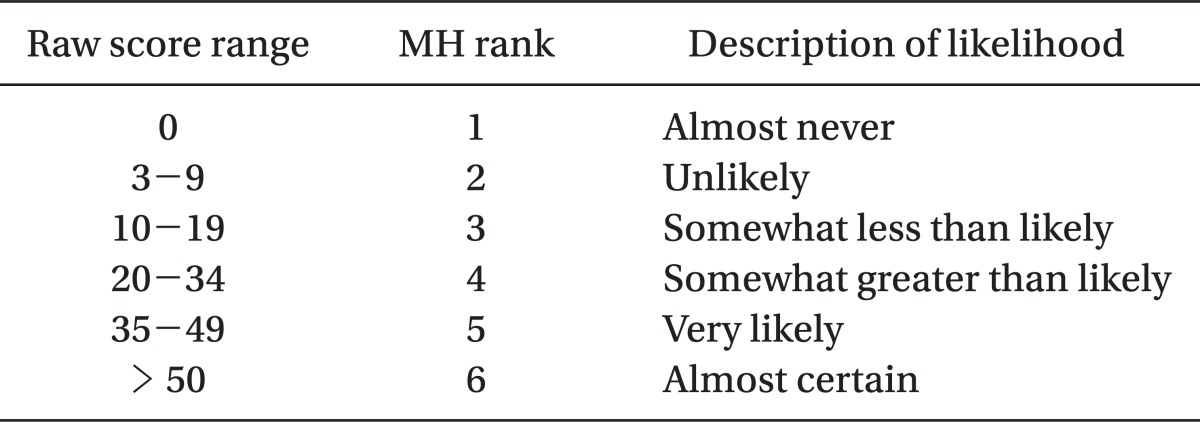
46. Larach MG, Localio AR, Allen GC, Denborough MA, Ellis FR, Gronert GA, et al. A clinical grading scale to predict malignant hyperthermia susceptibility. Anesthesiology. 1994; 80:771–779. PMID:
8024130.

47. Von Richthofen V, Wappler F, Scholz J, Fiege M, Schulte am Esch J. Evaluation of malignant hyperthermia episodes with the Clinical Grading Scale. Anasthesiol Intensivmed Notfallmed Schmerzther. 1998; 33:244–249. PMID:
9617423.
48. Lee JW, Moon SS, Lee JR, Kim DC. Reevaluation by clinical grading scale for malignant hyperthermia reported in Korean Journal of Anesthesiology. Korean J Anesthesiol. 2008; 54:640–645.

49. Larach MG, MacLennan DH. How carefully can we phenotype patients suspected of malignant hyperthermia susceptibility? Anesthesiology. 1999; 90:645–648. PMID:
10078661.

50. Kalow W, Britt BA, Terreau ME, Haist C. Metabolic error of muscle metabolism after recovery from malignant hyperthermia. Lancet. 1970; 2:895–898. PMID:
4097281.

51. Ellis FR, Harriman DG, Keaney NP, Kyei-Mensah K, Tyrrell JH. Halothane-induced muscle contracture as a cause of hyperpyrexia. Br J Anaesth. 1971; 43:721–722. PMID:
5564247.
52. The Malignant Hyperpyrexia Group. A protocol for the investigation of malignant hyperpyrexia (MH) susceptibility. Br J Anaesth. 1984; 56:1267–1269. PMID:
6487446.
53. Larach MG. North American Malignant Hyperthermia Group. Standardization of the caffeine halothane muscle contracture test. Anesth Analg. 1989; 69:511–515. PMID:
2675676.

54. Fletcher JE, Conti PA, Rosenberg H. Comparison of North American and European malignant hyperthermia group halothane contracture testing protocols in swine. Acta Anaesthesiol Scand. 1991; 35:483–487. PMID:
1897341.

55. Allen GC, Larach MG, Kunselman AR. The North American Malignant Hyperthermia Registry of MHAUS. The sensitivity and specificity of the caffeine-halothane contracture test: a report from the North American Malignant Hyperthermia Registry. Anesthesiology. 1998; 88:579–588. PMID:
9523799.
56. Ording H, Brancadoro V, Cozzolino S, Ellis FR, Glauber V, Gonano EF, et al. The European Malignant Hyperthermia Group. In vitro contracture test for diagnosis of malignant hyperthermia following the protocol of the European MH Group: results of testing patients surviving fulminant MH and unrelated low-risk subjects. Acta Anaesthesiol Scand. 1997; 41:955–966. PMID:
9311391.
57. Fletcher JE, Rosenburg H, Aggarwal M. Comparison of European and North American malignant hyperthermia diagnostic protocol outcomes for use in genetic studies. Anesthesiology. 1999; 90:654–661. PMID:
10078664.

58. Ording H, Bendixen D. Sources of variability in halothane and caffeine contracture tests for susceptibility to malignant hyperthermia. Eur J Anaesthesiol. 1992; 9:367–376. PMID:
1396623.
59. Nelson TE, Rosenberg H, Muldoon SM. Genetic testing for malignant hyperthermia in North America. Anesthesiology. 2004; 100:212–214. PMID:
14739790.

60. Urwyler A, Deufel T, McCarthy T, West S. Guidelines for molecular genetic detection of susceptibility to malignant hyperthermia. Br J Anaesth. 2001; 86:283–287. PMID:
11573677.

61. Rosenberg H, Rueffert H. Clinical utility gene card for: malignant hyperthermia. Eur J Hum Genet. 2011; 19.

62. Girard T, Treves S, Voronkov E, Siegemund M, Urwyler A. Molecular genetic testing for malignant hyperthermia susceptibility. Anesthesiology. 2004; 100:1076–1080. PMID:
15114203.

63. McCarthy TV, Healy JM, Heffron JJ, Lehane M, Deufel T, Lehmann-Horn F, et al. Localization of the malignant hyperthermia susceptibility locus to human chromosome 19q12-13.2. Nature. 1990; 343:562–564. PMID:
2300206.
64. Rosenberg H, Sambuughin N, Dirksen R. Malignant hyperthermia susceptibility. GeneReviews at GeneTests: Medical Genetics Information Resource database online. 1997-2011. Accessed August 1, 2012. Seattle: University of Washington;Updated January 19, 2010. Available at
http://www.genetests.org.
65. Deufel T, Sudbrak R, Feist Y, Rübsam B, Du Chesne I, Schäfer KL, et al. Discordance, in a malignant hyperthermia pedigree, between in vitro contracture-test phenotypes and haplotypes for the MHS1 region on chromosome 19q12-13.2, comprising the C1840T transition in the RYR1 gene. Am J Hum Genet. 1995; 56:1334–1342. PMID:
7762556.
66. MacLennan DH. Discordance between phenotype and genotype in malignant hyperthermia. Curr Opin Neurol. 1995; 8:397–401. PMID:
8542047.

67. Robinson R, Hopkins P, Carsana A, Gilly H, Halsall J, Heytens L, et al. Several interacting genes influence the malignant hyperthermia phenotype. Hum Genet. 2003; 112:217–218. PMID:
12522565.

68. Robinson RL, Anetseder MJ, Brancadoro V, van Broekhoven C, Carsana A, Censier K, et al. Recent advances in the diagnosis of malignant hyperthermia susceptibility: how confident can we be of genetic testing? Eur J Hum Genet. 2003; 11:342–348. PMID:
12700608.

69. Robinson RL, Anetseder MJ, Brancadoro V, van Broekhoven C, Carsana A, Censier K, et al. Recent advances in the diagnosis of malignant hyperthermia susceptibility: how confident can we be of genetic testing? Eur J Hum Genet. 2003; 11:342–348. PMID:
12700608.

70. Glahn KP, Ellis FR, Halsall PJ, Müller CR, Snoeck MM, Urwyler A, et al. Recognizing and managing a malignant hyperthermia crisis: guidelines from the European Malignant Hyperthermia Group. Br J Anaesth. 2010; 105:417–420. PMID:
20837722.

71. Inan S, Wei H. The cytoprotective effects of dantrolene: a ryanodine receptor antagonist. Anesth Analg. 2010; 111:1400–1410. PMID:
20861418.
72. Krause T, Gerbershagen MU, Fiege M, Weisshorn R, Wappler F. Dantrolene--a review of its pharmacology, therapeutic use and new developments. Anaesthesia. 2004; 59:364–373. PMID:
15023108.
73. Kurihara T, Brooks JE. Excitation-contraction uncoupling. The effect of hyperosomolar glycerol solution and dantrolene sodium on mammalian muscle in vitro. Arch Neurol. 1975; 32:92–97. PMID:
164844.
74. Bosch X, Poch E, Grau JM. Rhabdomyolysis and acute kidney injury. N Engl J Med. 2009; 361:62–72. PMID:
19571284.

75. Burkman JM, Posner KL, Domino KB. Analysis of the clinical variables associated with recrudescence after malignant hyperthermia reactions. Anesthesiology. 2007; 106:901–906. PMID:
17457120.

76. Afifi AK. Idiopathic hyperCKemia revisited. J Child Neurol. 1998; 13:251–252. PMID:
9660505.

77. Sunohara N, Takagi A, Nonaka I, Sugita H, Satoyoshi E. Idiopathic hyperCKemia. Neurology. 1984; 34:544–547. PMID:
6538316.

78. Prelle A, Tancredi L, Sciacco M, Chiveri L, Comi GP, Battistel A, et al. Retrospective study of a large population of patients with asymptomatic or minimally symptomatic raised serum creatine kinase levels. J Neurol. 2002; 249:305–311. PMID:
11993531.

79. Simmons Z, Peterlin BL, Boyer PJ, Towfighi J. Muscle biopsy in the evaluation of patients with modestly elevated creatine kinase levels. Muscle Nerve. 2003; 27:242–244. PMID:
12548533.

80. Capasso M, De Angelis MV, Di Muzio A, Scarciolla O, Pace M, Stuppia L, et al. Familial idiopathic hyper-CKemia: an under-recognized condition. Muscle Nerve. 2006; 33:760–765. PMID:
16502425.

81. Ellis FR, Clarke IM, Modgill M, Currie S, Harriman DG. Evaluation of creatinine phosphokinase in screening patients for malignant hyperpyrexia. Br Med J. 1975; 3:511–513. PMID:
1164612.

82. Paasuke RT, Brownell AK. Serum creatine kinase level as a screening test for susceptibility to malignant hyperthermia. JAMA. 1986; 255:769–771. PMID:
3944979.

83. Lingaraju N, Rosenberg H. Unexplained increases in serum creatine kinase levels: its relation to malignant hyperthermia susceptibility. Anesth Analg. 1991; 72:702–705. PMID:
2018229.
84. Weglinski MR, Wedel DJ, Engel AG. Malignant hyperthermia testing in patients with persistently increased serum creatine kinase levels. Anesth Analg. 1997; 84:1038–1041. PMID:
9141928.

85. Malandrini A, Orrico A, Gaudiano C, Gambelli S, Galli L, Berti G, et al. Muscle biopsy and in vitro contracture test in subjects with idiopathic hyperCKemia. Anesthesiology. 2008; 109:625–628. PMID:
18813041.

86. Kasi PM. Malignant Hyperthermia and Idiopathic HyperCKemia. Case Report Med. 2011; 2011:194296. PMID:
22162697.

87. Monnier N, Kozak-Ribbens G, Krivosic-Horber R, Nivoche Y, Qi D, Kraev N, et al. Correlations between genotype and pharmacological, histological, functional, and clinical phenotypes in malignant hyperthermia susceptibility. Hum Mutat. 2005; 26:413–425. PMID:
16163667.

88. Davis PJ, Brandom BW. The association of malignant hyperthermia and unusual disease: when you're hot you're hot, or maybe not. Anesth Analg. 2009; 109:1001–1003. PMID:
19762721.

89. Klingler W, Rueffert H, Lehmann-Horn F, Girard T, Hopkins PM. Core myopathies and risk of malignant hyperthermia. Anesth Analg. 2009; 109:1167–1173. PMID:
19762745.

90. Benca J, Hogan K. Malignant hyperthermia, coexisting disorders, and enzymopathies: risks and management options. Anesth Analg. 2009; 109:1049–1053. PMID:
19762731.

91. Quinlivan RM, Muller CR, Davis M, Laing NG, Evans GA, Dwyer J, et al. Central core disease: clinical, pathological, and genetic features. Arch Dis Child. 2003; 88:1051–1055. PMID:
14670767.

92. Frank JP, Harati Y, Butler IJ, Nelson TE, Scott CI. Central core disease and malignant hyperthermia syndrome. Ann Neurol. 1980; 7:11–17. PMID:
7362206.

93. Jungbluth H. Central core disease. Orphanet J Rare Dis. 2007; 2:25. PMID:
17504518.

94. Wu S, Ibarra MC, Malicdan MC, Murayama K, Ichihara Y, Kikuchi H, et al. Central core disease is due to RYR1 mutations in more than 90% of patients. Brain. 2006; 129:1470–1480. PMID:
16621918.

95. Jungbluth H. Multi-minicore disease. Orphanet J Rare Dis. 2007; 2:31. PMID:
17631035.
96. Jungbluth H, Zhou H, Hartley L, Halliger-Keller B, Messina S, Longman C, et al. Minicore myopathy with ophthalmoplegia caused by mutations in the ryanodine receptor type 1 gene. Neurology. 2005; 65:1930–1935. PMID:
16380615.

97. Ferreiro A, Quijano-Roy S, Pichereau C, Moghadaszadeh B, Goemans N, Bonnemann C, et al. Mutations of the selenoprotein N gene, which is implicated in rigid spine muscular dystrophy, cause the classical phenotype of multiminicore disease: reassessing the nosology of early-onset myopathies. Am J Hum Genet. 2002; 71:739–749. PMID:
12192640.

98. Koch BM, Bertorini TE, Eng GD, Boehm R. Severe multicore disease associated with reaction to anaesthesia. Arch Neurol. 1985; 42:1204–1206. PMID:
4062619.
99. Jeong SK, Kim DC, Cho YG, Sunwoo IN, Kim DS. A double mutation of the ryanodine receptor type 1 gene in a malignant hyperthermia family with multiminicore myopathy. J Clin Neurol. 2008; 4:123–130. PMID:
19513315.

100. King JO, Denborough MA. Anaesthetic-induced malignant hyperpyrexia in children. J Pediatr. 1973; 83:37–40. PMID:
4149045.
101. Isaacs H, Badenhorst ME. Dominantly inherited malignant hyperthermia (MH) in the King-Denborough syndrome. Muscle Nerve. 1992; 15:740–742. PMID:
1508238.

102. D'Arcy CE, Bjorksten A, Yiu EM, Bankier A, Gillies R, McLean CA, et al. King-Denborough syndrome caused by a novel mutation in the ryanodine receptor gene. Neurology. 2008; 71:776–777. PMID:
18765655.
103. Kim DC, Kim DS. Identification of G7304A mutation in the ryanodine receptor type 1 gene in a patient with malignant hyperthermia and an extended pedigree study in a korean malignant hyperthermia family. Korean J Anesthesiol. 2003; 44:56–64.

104. Lee H, Kim DC, Lee JH, Cho YG, Lee HS, Choi SI, et al. Molecular genetic analysis of the ryanodine receptor gene (RYR1) in Korean malignant hyperthermia families. Korean J Lab Med. 2010; 30:702–710. PMID:
21157159.

105. Lee JW, Moon SS, Lee JR, Kim DC. Reevaluation by clinical grading scale for malignant hyperthermia reported in Korean journal of anesthesiology. Korean J Anesthesiol. 2008; 54:640–645.