Introduction
As surgeries for aged patients are increasing consistently, total knee replacement surgery caused by internal derangement of the knee has also grown. Total knee replacement surgery is mainly performed in the aged with cardiopulmonary or cerebrovascular disease. A pneumatic tourniquet, used in total knee replacement surgery to minimize blood loss and secure a clean surgical field, may intensify the risk of complications like hypertension or hypotension, deep vein thrombosis, cerebral infarction, rhabdomyolsis, nerve injury, swelling or stiffness, hematoma, and infection; thus, meticulous care is important in anesthesia [
1].
Compared with the average adult patients, the aged are more vulnerable to blood pressure regulation due to changes in autonomic nervous system and decrease in cardiac reserve. Therefore, sudden blood pressure fluctuation can be fatal to the aged even leading to cardiac or brain ischemia. Furthermore, various accompanying diseases may endanger the aged during anesthesia and perioperative period [
2]. Inflation and deflation of a pneumatic tourniquet during surgery induces miscellaneous alterations in patient's hemodynamic and metabolic status. Especially, reperfusion to the exsanguinated area and bleeding from the surgical area, following tourniquet deflation, gives rise to hypotension, arterial oxygen and carbon dioxide partial pressure modification, lactic acidemia, and hyperkalemia [
1,
3]. Cerebral hypoperfusion secondary to hypotension may bring about postoperative cognitive dysfunction in the aged. Considering an increased possibility of several complications in the aged, appropriate monitoring becomes critical in anesthesia. Contrary to cardiovascular monitoring, such as electrocardiography, blood pressure, pulse oximetry, and arterial blood gas analysis performed routinely, monitoring for the central nervous system is rare, making it difficult to find out neurologic adverse events during general anesthesia. Near-infrared spectroscopy (NIRS) is a noninvasive, continuous monitoring device, designed to estimate the regional cerebral oxygen saturation (rSO
2) by expressing the percentage between oxygenated and deoxygenated hemoglobin in the cerebral tissues. Accordingly, NIRS reflects a balance among cerebral oxygen supply and demand, enabling the effective surveillance for brain ischemia [
4-
6].
As the aged lack compensatory mechanism to adjust to hemodynamic changes, following tourniquet deflation, aggressive anesthetic management through active monitoring is essential. We evaluated the effect of tourniquet deflation on hemodynamics and regional cerebral oxygen saturation in the aged undergoing total knee replacement surgery, under general anesthesia, utilizing NIRS.
Go to :

Materials and Methods
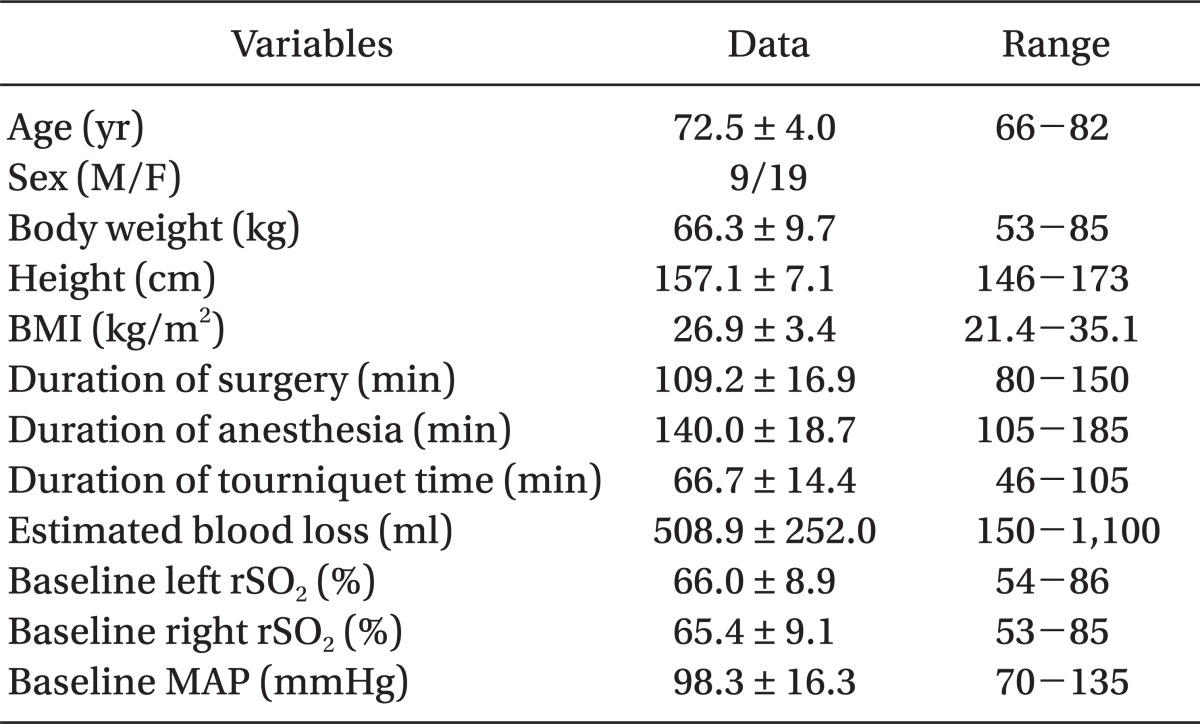
After obtaining approval from the Institutional Review Board and written informed consent, twenty-eight American Society of Anesthesiologists (ASA) physical status I or II patients, over the age of sixty-five years scheduled for total knee replacement surgery under general anesthesia, were enrolled in the study. Patients with a history of hypertension, stroke, heart failure or arrhythmia, chronic obstructive pulmonary disease, chronic kidney disease, and liver cirrhosis were excluded from the study.
No premedication was given. When patients arrived in the operating room, standard monitoring, including 3-lead electrocardiography, automatic noninvasive blood pressure, and peripheral pulse oximetry was attached in supine position. To measure the regional cerebral oxygen saturation (rSO2), cerebral oximetry sensors (Adult SomaSensors®, Somanetics, Troy, MI, USA) were placed bilaterally on the forehead 2 cm above the eyebrows with both diodes meeting at the center and connected to cerebral oximetry monitoring device (INVOS® System-Model 5100, Somanetics, Troy, MI, USA). To monitor the arterial blood pressure continuously during the surgery and perform arterial blood gas analysis, 22 gauge catheter was inserted into the radial artery after modified Allen's test and cardiac output monitoring device (Vigileo/FloTrac™ System, Edwards Lifesciences, Irvine, CA, USA) was applied. Prior to induction of anesthesia, baseline data, including the mean arterial pressure (MAP), heart rate (HR), left and right rSO2, cardiac output (CO), and stroke volume (SV), were collected after 5 min of stabilizing period.
After 3 min of pre-oxygenation with 6 L of oxygen via a face mask, general anesthesia was induced with 0.04 mg/kg of midazolam, 0.2 mg of glycopyrrolate, 4 mg/kg of thiopental sodium, and 1 µg/kg of fentanyl. When the patient's unconsciousness was confirmed, 0.6 mg/kg of rocuronium was given intravenously to facilitate endotracheal intubation, and the patient was manually ventilated with 100% oxygen for 90 s before intubation. Anesthesia was maintained with mixture of oxygen and nitrous oxide, at flow rate of 1.5 L/min each. The end tidal sevoflurane concentration was adjusted to be between 1.0-2.0 vol%. Initial tidal volume and respiratory rate was set as 10 ml/kg and 10/min. The end tidal carbon dioxide partial pressure was adjusted between 30-35 mmHg. All patients maintained normothermia, using a warming device (Bair Hugger® Warming Unit-Model 505, Arizant Healthcare Inc., Eden Prairie, MN, USA).
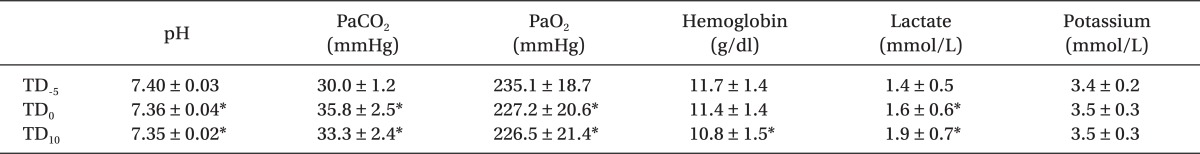
Before skin incision, a pneumatic tourniquet applied to the ipsilateral thigh was inflated to 350 mmHg. All monitoring data were recorded before induction of anesthesia and every 2 min after tourniquet deflation for 20 min. Arterial blood gas analysis was performed 5 min before, and in addition to 0, and 10 min after tourniquet deflation.
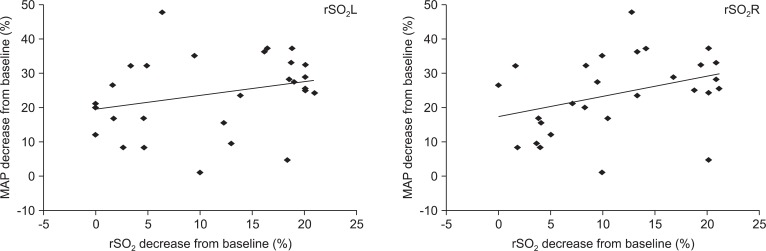
Statistical analysis was performed using SPSS (IBM® SPSS® Statistics 20, SPSS Inc., IBM Corporation, Armonk, NY, USA) and all data were expressed as the mean ± SD or absolute numbers. Repeated-measures ANOVA was used to compare the baseline data with the data at each time point. Linear regression analysis was used to determine the correlation between the maximal decrease of the mean arterial pressure and regional cerebral oxygen saturation, after converting the data according to the following formulas.
A P value less than 0.05 was considered statistically significant.
Go to :

Discussion
The object of this study was to research the effect of tourniquet deflation on hemodynamics and regional cerebral oxygen saturation in the aged patients undergoing total knee replacement surgery, under general anesthesia. In the aged, functional disorders arising from the stiffened heart and blood vessels, decreased response to beta receptor stimulation, autonomic imbalance or dysfunction, and impaired conducting system are common [
2]. Although the central nervous system is considered as the primary endpoint of general anesthesia, perioperative central nervous system monitoring is seldom practiced. Perioperative neurological complications, including stroke, though rare with an incidence of 0.05-7%, can be disastrous for the patient, its family, and the medical team [
7]. Consequently, the necessity of the central nervous system monitoring has emerged. Transcranial Doppler (TCD), jugular bulb venous oxygen saturation, and somatosensory evoked potentials are being used currently [
8]. Nevertheless, owing to its invasiveness and technical difficulty, general application remains controversial. Choi et al. [
9] examined the changes in the brain activity during tourniquet deflation by measuring the bispectral index (BIS) and reported that BIS decreased during tourniquet deflation in patients undergoing knee arthroscopic surgery under general anesthesia, emphasizing proper monitoring for neurologically critical patients.
NIRS is a monitoring device designed to estimate the rSO
2 non-invasively and continuously. By attaching a light-emitting diode (LED) on the scalp, which emits two different near-infrared wavelengths into the skull, NIRS calculates the ratio of oxyhemoglobin to deoxyhemoglobin [
5]. NIRS proved similar accuracy for the detection of cerebral ischemia, compared to the other invasive methods [
8,
10]. Hence, NIRS is appreciated as credible monitoring device that not only perceives variations in cerebral oxygenation caused by systemic hypoxemia, but also assesses the lowest limit for cerebral autoregulation [
11].
Following tourniquet deflation, reperfusion to the exsanguinated lower extremities occurs and central venous pressure (CVP), MAP, and CO decreases as a result [
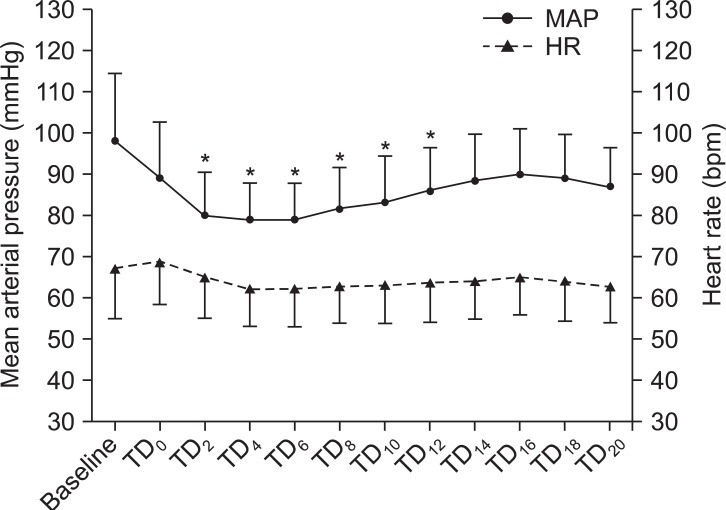
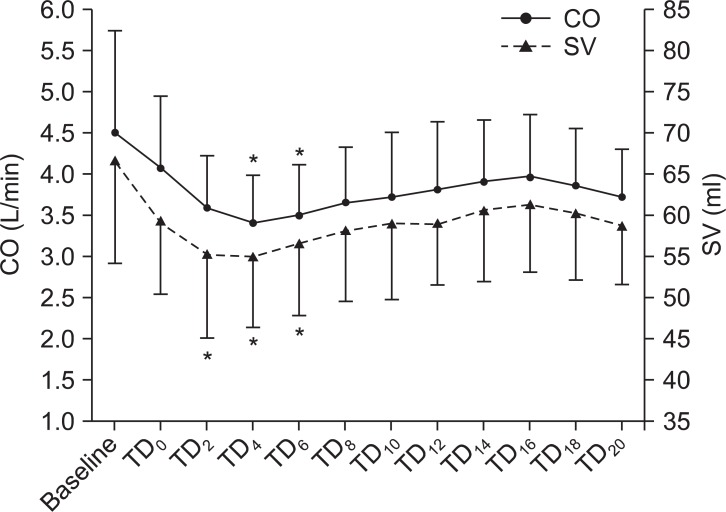
12]. In this study, MAP, CO, and SV showed significant decrease during 2 to 12, 4 to 6, and 2 to 6-min period after tourniquet deflation, respectively. The effect of tourniquet deflation on HR varies in several reports. Cheong et al. [
13] detected no significant changes in HR, whereas, Choi et al. [
12] described that HR significantly increased in all groups (general anesthesia in control, epidural anesthesia in control, epidural anesthesia in elderly) except for general anesthesia in elderly group. In this study, HR showed no significant changes after tourniquet deflation. Townsend et al. [
14] reported maximum changes in arterial pH, PaCO
2, potassium, lactate, and bicarbonate concentration, 3 min after tourniquet deflation. In this study, significant decrease in the pH and PaO
2 accompanied by significant increase in PaCO
2 and lactate were observed, immediately after tourniquet deflation. Hemoglobin showed significant decrease 10 min after tourniquet deflation, and potassium showed no significant changes. Meanwhile, as the changes above were all in normal range, rSO
2 may not have been affected.
The rSO
2 well reflects the cerebral oxygenation during hypoxemia, hypocapnia, hypercapnia, and hypotension, markedly making it valuable for the central nervous system monitoring during anesthesia and surgery, particularly in hypotensive episodes. Hypotension reduces cerebral blood flow, secondarily generates cerebral ischemia and may bring out adverse neurological outcomes [
5]. Cerebral autoregulation refers to the ability of the brain to maintain a constant cerebral blood flow, despite changes in systemic blood pressure or cerebral perfusion pressure. Cerebral autoregulation typically operates between MAP of 60 and 150 mmHg [
15]. However, Schmidt et al. [
16] claimed the lowest MAP for cerebral autoregulation to be 85 ± 5 mmHg in normal patients and 113 ± 7 mmHg in hypertensive patients. If MAP falls below the lowest limit for cerebral autoregulation, cerebral blood flow decreases, and so does the rSO
2. Relationship between the decrease of rSO
2 and MAP has not been clarified yet, causing controversies. Lee et al. [
17] studied changes in rSO
2 during the sitting position for shoulder arthroscopic surgery, and found no significant correlation between MAP and rSO
2. Chu et al. [
18] predicted changes of rSO
2 based on the changes of MAP and HR in patients under spinal anesthesia, discovering that the effects of MAP and HR decrease on rSO
2 lasted continuously for at least 6 min. In this study, there was no relationship between the maximal decrease of MAP and rSO
2 in both the left and right.
Aging acts as a prominent risk factor for perioperative neurologic complications [
7] and the aged are sensitive to cerebral blood flow decline in particular. The rSO
2 is known to be influenced by age, PaCO
2, hemoglobin, cerebral blood flow, and changes in the cerebral metabolic rate. The normal range of rSO
2 has not been established so far; Madsen et al. [
19] insisted 55-78%, and Kim et el. [
20] asserted 71 ± 6% in healthy volunteers, aged 20-36. Papadopoulos et al. [
21] reported that the baseline rSO
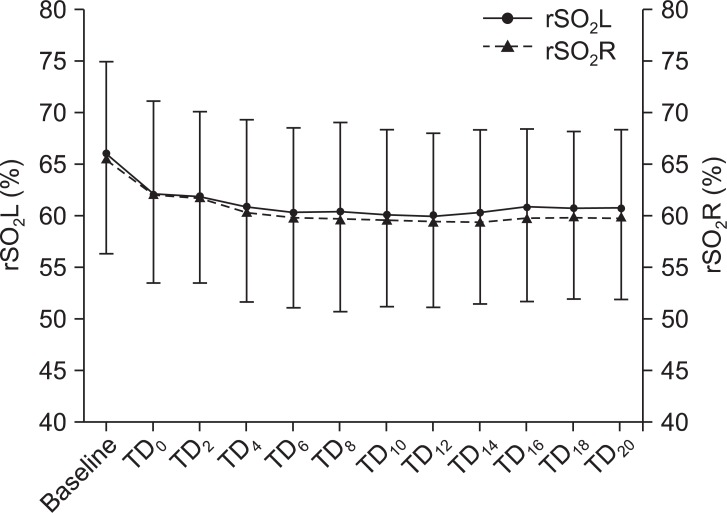
2 values have highly significant positive correlation with preoperative hematocrit and arterial hemoglobin oxygen saturation, but highly significant negative correlations with age and ASA classification. In this study, the decrease of rSO
2 was not significant during 20-min deflation period in both the left and right. The minimum value of rSO
2 was 60.1 ± 7.1% in the left and 59.4 ± 7.8% in the right. Tsuchiya et al. [
22] recommended higher fraction of inspired oxygen to preserve cerebral oxygen delivery in the controlled hypotension during anesthesia. In this study, the arterial oxygen partial pressure maintained above 200 mmHg might have contributed to an insignificant decrease in rSO
2.
Reflecting only the rSO
2 of specific part of the brain and wide variation among individuals affected by changes in the extracranial blood flow or sensor location have been pointed out as weaknesses of NIRS [
23]. For that reason, recognizing the cerebral ischemia based on the changes in rSO
2, rather than diagnosing cerebral ischemia by absolute rSO
2 values, is considered worthwhile [
5]. Casati et al. [
24] stated the association between intraoperative cerebral desaturation and postoperative cognitive decline. Samra et al. [
25] discovered 20% decrease in rSO
2 from the baseline as a predictor of neurologic compromise. Regarding the insignificant decrease in the rSO
2 after tourniquet deflation and the minimum rSO
2 values measured in this study, tourniquet deflation may not escalate the risk of neurologic complications solely. Nonetheless, further studies on multiple factors influencing the rSO
2 are needed.
In conclusion, tourniquet deflation created significant hemodynamic and metabolic changes in the aged undergoing total knee replacement surgery under general anesthesia. The rSO2 decreased, but insignificantly and no relationship between MAP and rSO2 was found. Still, since the aged lack compensatory mechanism to adjust to dynamic changes, aggressive anesthetic management through active monitoring is crucial.
Go to :





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download