Abstract
Paroxysmal supraventricular tachycardia (SVT) is a common arrhythmia in the parturient and can occur with or without an underlying organic heart disease. A woman of 35 weeks' gestation, who had a paroxysmal SVT that was resistant to antiarrhythmic drugs and electric cardioversion, required emergency Cesarean delivery. The Cesarean delivery was performed under spinal anesthesia and a healthy baby was delivered uneventfully. SVT spontaneously converted to normal sinus rhythm right after delivery of the baby.
Cardiac arrhythmias, especially supraventricular tachycardia (SVT), frequently occur during pregnancy, even in patients without detectable organic heart disease. Although most of them are benign, more serious arrhythmias are usually associated with mitral stenosis in parturients with rheumatic heart disease [1]. Therefore, patients with arrhythmia during pregnancy should be evaluated to rule out organic heart disease.
Here, we present a case of maternal SVT that was resistant to antiarrhythmic agents and electric cardioversion, and required emergency Caesarean delivery. The anesthetic implication and treatment of paroxysmal SVT in the parturients will be discussed.
At 35 weeks of gestation, a 37-year-old (height 162 cm and weight 85.1 kg) primigravida visited the emergency department with complaints of unceasing palpitations, without associated symptoms such as dizziness, syncope or dyspnea. She had no history of any significant disease and her pregnancy had been uneventful. Upon questioning, she described a history of occasional palpitations over the past few years, which went away spontaneously in minutes.
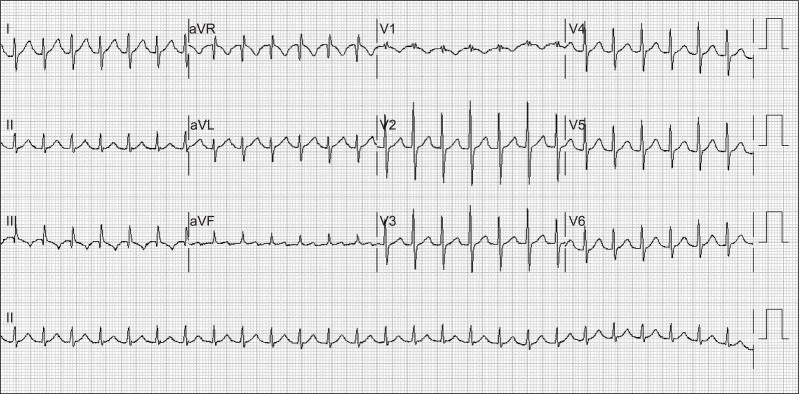
EKG showed the presence of a SVT at a rate over 160 beats/min with stable blood pressure (Fig. 1). Three boluses of IV adenosine (6 mg → 12 mg → 12 mg) were injected after unsuccessful carotid sinus massage. The SVT reverted to a normal sinus rhythm for only several minutes with adenosine, and SVT recurred. IV verapamil (5 mg) and two trials of synchronized electric cardioversion (150 J → 200 J) were also unsuccessful. Emergency Cesarean delivery was then performed because of uncertainty about the maternal health and concern for the fetus.
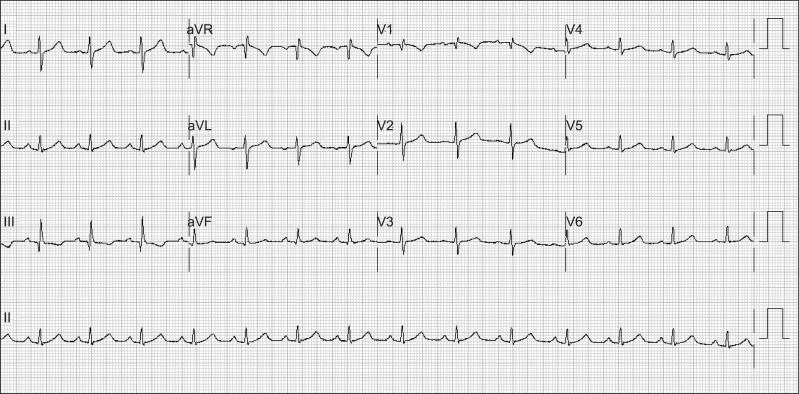
A spinal anesthesia was performed using 10 mg of bupivacaine and 20 µg of fentanyl after 500 ml of 6% HES 130/0.4 infusion. Phenylephrine (0.2 µg/min/kg) was given to prevent spinal anesthesia related hypotension and 50 µg of phenylephrine was occasionally administered when systolic blood pressure was lower than 100 mmHg. The systolic blood pressure maintained between 90-120 mmHg. Total infused dose of phenylephrine before delivery of a baby was 350 µg with bolus and 60 µg with continuous infusion. A healthy baby was delivered uneventfully, and 100 µg of carbetocin was infused slowly without any complications. Her heart rate was around 150 beats/min throughout the operation, which suddenly dropped to 80-90 beats/min at the end of surgery. A normal sinus rhythm was maintained during the postoperative period (Fig. 2). A 24-hour Holter monitor and a cardiac echography were performed the next day, but no abnormalities were found. She was discharged after one week of postnatal care in the hospital without any episodes of palpitations.
It has been reported that newly onset of paroxysmal SVT was rare but symptoms of paroxysmal SVT were shown to be exacerbated in some patients during pregnancy [2]. Hemodynamic, hormonal, autonomic, and emotional changes during pregnancy can be the precipitating factors for arrhythmia [3-5]. Depending on the gestational age, maternal and fetal condition, emergency delivery should always be an option. In our case, the patient was unresponsive to carotid massage, antiarrythmics, and electric cardioversion. Paroxysmal SVT lasting longer than 6 hours has been associated with left ventricular failure [6]. Thus, considering her gestational age and the possibility of heart failure, emergency delivery was the best course of action for the mother and the baby.
Anesthetic management of parturients with paroxysmal SVT for Cesarean delivery is not a straightforward decision. Anesthetic management should focus on avoiding factors known to produce cardiac ectopy, such as increased sympathetic tone, electrolyte imbalances and acid-base disturbance. Volatile agents may reduce the incidence of perioperative tachyarrhythmias because they increased refractoriness within the accessory and atrioventricular pathways [7]. But, it is almost impossible to avoid sympathetic stimulation during intubation in general anesthesia for Cesarean delivery. Hypotension related to regional anesthesia might be another problem. In this regard, epidural anesthesia can be preferred over spinal anesthesia. However, we decided to do spinal anesthesia because we had more experience in spinal anesthesia than epidural anesthesia and hypotension during spinal anesthesia can be managed safely with appropriate treatment.
There are a few points that should be considered for spinal anesthesia during Cesarean delivery in this case. The reduced atrial filling associated with spinal anesthesia has been identified as a risk factor for arrhythmia [8]. Fluid pre-loading could prevent a reduction in atrial filling and also reduce sympathomimetic requirements, which may trigger SVT [9]. Sympathomimetics, which are frequently used to treat hypotension during spinal anesthesia, may also initiate tachycardia. There was a previous case of SVT, which was induced by ephedrine during Cesarean delivery [10]. The combined use of ephedrine and phenylephrine in treating hypotension after spinal anesthesia for Cesarean delivery abolishes the increase in heart rate and effectively maintains the blood pressure [11]. We used phenylephrine alone throughout the surgery and weaned the patient off this drug after SVT terminated. Phenylephrine increases the vagal tone by indirectly stimulating baroreceptor reflexes, which ultimately reduces SVT occurrence [9], and may have advantages over ephedrine.
In general, drug therapy strategy used in parturients is similar to that in non-pregnant patients. However, the effects of antiarrhythmics on the fetus and uterine blood flow and contractility must be considered. For this reason, non-pharmacological treatment such as vagal maneuvers, Valsalva maneuver and facial ice immersion should be tried first to terminate tachycardia [12]. When the vagal maneuver fails, intravenous adenosine is the first-choice drug because of its rapid onset, high efficacy and short half-life [13].
Calcium channel blockers can also be used if adenosine is not effective. The adverse side effect of these drugs is hypotension, which is more common with the use of diltiazem than verapamil [14]. These changes may not be physiologically important to the fetus, but may be consequential in patients with cardiovascular dysfunction.
Synchronized electrical cardioversion may become necessary for SVT that are resistant to pharmacological therapy, like our case. Direct current electrical shock has been used in all stages in pregnancy without significant complications [15]. The amount of current that reaches the fetus is thought to be negligible. However, fetal heart rate monitoring during cardioversion is advisable.
Non-pharmacological treatments, antiarrythmics, and even electrical cardioversion were unsuccessful in our case and emergency cesarean delivery was performed. Every treatment provided to the mother should be considered carefully, weighing the risk of their use against the risk of continuing SVT. If Cesarean delivery is performed, conditions that could exacerbate the symptoms must be avoided.
References
1. Rotmensch HH, Rotmensch S, Elkayam U. Management of cardiac arrhythmias during pregnancy. Current concepts. Drugs. 1987; 33:623–633. PMID: 3301303.
2. Lee SH, Chen SA, Wu TJ, Chiang CE, Cheng CC, Tai CT, et al. Effects of pregnancy on first onset and symptoms of paroxysmal supraventricular tachycardia. Am J Cardiol. 1995; 76:675–678. PMID: 7572623.
3. Hunter S, Robson SC. Adaptation of the maternal heart in pregnancy. Br Heart J. 1992; 68:540–543. PMID: 1467047.

4. Hong JH, Sohn DJ, Kim AR, Jang YH, Kim JM, Bae JI. Supraventricular tachycardia developed by the concealed bypass tract in a parturient: a case report. Korean J Anesthesiol. 2005; 48:108–111.

5. Speranza G, Verlato G, Albiero A. Autonomic changes during pregnancy: assessment by spectral heart rate variability analysis. J Electrocardiol. 1998; 31:101–109. PMID: 9588655.

6. Mangano DC. Hughes SC, Levinson G, Rosen MA, editors. Anesthesia for the pregnant cardiac patient, Shnider and Levinson's Anesthesia for Obstetrics. 2001. 4th ed. Philadelphia: Lipppincott Williams & Wilkins;p. 477–478.
7. Sharpe MD, Dobkowski WB, Murkin JM, Klein G, Guiraudon G, Yee R. The electrophysiologic effects of volatile anesthetics and sufentanil on the normal atrioventricular conduction system and accessory pathways in Wolff-Parkinson-White syndrome. Anesthesiology. 1994; 80:63–70. PMID: 8291732.

8. Van Zijl DH, Dyer RA, Millar RN, James MF. Supraventricular tachycardia during spinal anaesthesia for caesarean section. Int J Obstet Anesth. 2001; 10:202–205. PMID: 15321611.
9. Ngan Kee WD, Khaw KS, Lee BB, Ng FF, Wong MM. Randomized controlled study of colloid preload before spinal anaesthesia for caesarean section. Br J Anaesth. 2001; 87:772–774. PMID: 11878530.
10. Robins K, Lyons G. Supraventricular tachycardia in pregnancy. Br J Anaesth. 2004; 92:140–143. PMID: 14665567.

11. Hall PA, Bennett A, Wilkes MP, Lewis M. Spinal anaesthesia for caesarean section: comparison of infusions of phenylephrine and ephedrine. Br J Anaesth. 1994; 73:471–474. PMID: 7999486.

12. Sermer M, Colman J, Siu S. Pregnancy complicated by heart disease: a review of Canadian experience. J Obstet Gynaecol. 2003; 23:540–544. PMID: 12963517.

13. Wolbrette D. Treatment of arrhythmias during pregnancy. Curr Womens Health Rep. 2003; 3:135–139. PMID: 12628083.
14. Ghosh N, Luk A, Derzko C, Dorian P, Chow CM. The acute treatment of maternal supraventricular tachycardias during pregnancy: a review of the literature. J Obstet Gynaecol Can. 2011; 33:17–23. PMID: 21272431.

15. Klepper I. Cardioversion in late pregnancy. The anaesthetic management of a case of Wolff-Parkinson-White syndrome. Anaesthesia. 1981; 36:611–616. PMID: 7270830.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download