Abstract
A 37-year-old woman diagnosed with sickle cell anemia (SCA), beta (+) thalassemia, Crohn's disease, and liver dysfunction was scheduled for laparoscopic cholecystectomy (LC) due to acute cholecystitis with gall bladder. Regional anesthesia was performed. An epidural catheter was inserted into the 9-10 thoracal epidural space and then 15 ml of 0.5% bupivacaine was injected through the catheter. The level of sensorial analgesia tested with pinprick test reached up to T4. Here we describe the first case of the combination of sickle cell anemia (SCA), beta (+) thalassemia, and Crohn's disease successful anesthetic management with attention to hemodynamics, particularly with regards to liver dysfunction.
The primary pathology in thalassemia stems from the quantity of globin production, whereas the primary pathology in sickle cell anemia (SCA) is related to the quality of globin produced [1]. Careful perioperative and postoperative monitoring should allow hypoxemia, hypovolaemia, hypothermia, acidosis and over-transfusion to all be avoided because the erythrocytes undergo sickling. High erythrocyte turnover and hyperbilirubinemia is associated with an incidence of cholelithiasis estimated as high as 70% in the adult population. Cholecystectomy is the most common surgical procedure performed in sickle cell disease patients [2]. We report the case of a 37-year-old woman diagnosed with S/β+ thalassemia, Crohn's disease who presented with a liver enzyme disorder. She was effectively anesthetized for laparoscopic cholecystectomy using thoracic epidural anesthesia.
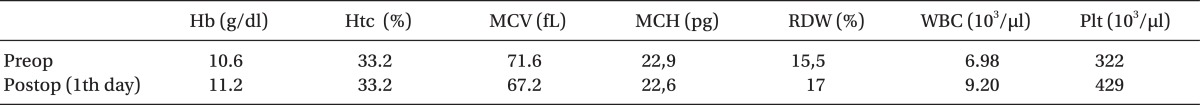
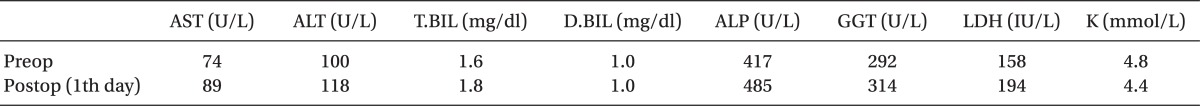
A 37-year-old female patient (161 cm, 49 kg) was admitted with sickle cell syndrome (SCA), S/Beta (β) positive thalassemia. Hemoglobin electrophoresis showed an HbS count of 58.5%, HbA count of 23.5%, HbA2 count of 7%, and an HbF count of 11%. Due to Crohn's disease and liver dysfunction, the patient was scheduled for elective laparoscopic cholecystectomy (LC) to treat acute cholecystitis. It was decided to perform the operation with thoracic epidural anesthesia (TEA) due to severely impaired liver function and hematologic problems. The patient had been diagnosed as having Crohn's colitis ten years prior to our clinic admission, following several episodes of abdominal pain and bloody diarrhoea. The diagnosis had been confirmed by radiology, endoscopic examination and biopsy of the gastrointestinal tract. Azathioprine was also used for treatment of Crohn's disease. Seven years ago the patient underwent successful elective cesarean surgery. During the diagnosis of SCA disease, plasma exchange occurred 7 times. Examination of each system revealed no abnormality. The reports of hemoglobin (Hb) level and liver function tests are shown in Table 1 and 2. Our patient was not given preoperative medication. Noninvasive monitoring (EKG, arterial blood pressure and pulse oximetry) was initiated on patient arrival. All data were recorded at 5 minutes intervals. During the monitoring, 500 ml of isolyte S was infused.
TEA was performed with a 20-G Tuohy needle and epidural catheter that was inserted 5 cm in the cephalic direction from T9/T10 for perioperative anesthetic management and postoperative
pain control. This was followed by a 15 ml injection of 0.5% bupivacaine through the catheter. Twenty-fifth minutes later, sensory blockage was established at T4. The patient received oxygen at a rate of 4 L/min through a facemask attached to an end tidal CO2 monitor. During the operation the patient was given a 10-25 microgram/kg/min propofol infusion for sedation, 2 mg midazolam for hypnotic, and 100 microgram fentanyl for shoulder pain. Shoulder pain was the main intraoperative problem observed in our patient. Surgery time was approximately 105 minutes with CO2 insufflations pressure ≤ 12 mmHg and was eventful. There was no need for intraoperative blood transfusion and our patient was taken to the intensive care unit without experiencing any problem during the surgical procedure. Throughout surgery, the patient remained hemodynamically stable with a pulse rate 64-78/min and a systolic blood pressure of 104-126 mmHg. After the operation during the 2nd and 4th hours, 0.5% bupivacaine was administered for postoperative pain control. The epidural catheter was removed after 24 hours. The patient was discharged from the hospital 3 days after surgery.
We describe the first case of sickle cell anemia (SCA), beta (+) thalassemia, and Crohn's disease, in which the patient was effectively anesthetized for laparoscopic cholecystectomy using thoracic epidural anesthesia, with particular attention to hemodynamics, especially in liver dysfunction.
The primary pathology in thalassemia stems from the quantity of globin production, whereas the primary pathology in sickle cell disease is related to the quality of globin produced. The sickle cell syndromes are caused by a genetic mutation in the β-globin chain of the hemoglobin molecule, where glutamic acid is substituted by valine at the sixth position and includes the prototype sickle cell anemia (homozygous), sickle cell carrier (heterozygous), hemoglobin SC disease, and sickle β thalassemia (S/β° thalassemia and S/β+ thalassemia). Sickle cell-β thalassemia disease most commonly occurs in people of Mediterranean descent [1,3].
The thalassemias share with the sickle haemoglobinopathies characteristics such as accelerated hemoglobin denaturation and degradation, excess free iron release, heightened oxidative stress, a hypercoagulable state, and widespread vascular damage. Common clinical features include chronic hemolytic anemia, pulmonary damage and hypoxemia, progressive neurological damage, intracranial hemorrhage, thrombotic stroke, deep vein thrombosis, arterial occlusion, leg ulcers, and shortened life expectancy [1-3]. Thus anesthetic management in the case we observed is critical and needs to be monitored carefully.
General anesthesia and surgical trauma add an additional risk of complication because of changes in temperature, pH, oxygen tension, and fluid volume. Careful perioperative and postoperative monitoring should allow the avoidance of hypoxemia, hypovolaemia, hypothermia, acidosis and over-transfusion since the erythrocytes undergo sickling. Epidural anesthesia, no special postoperative complications, may be applicable for LC. However, the incidence of intraoperative referred shoulder pain is high, and so careful patient recruitment and management of shoulder pain should be considered [2,4,5]. Thus we decided that our patient with sickle cell anemia, beta (+) thalassemia, and Crohn's disease, who demonstrated liver dysfunction would undergo anesthetic management using the thoracic epidural anesthesia (TEA) technique. During the operation, hemodynamics and postoperative liver function test parameters were stable. Nevertheless intraoperative shoulder pain was a major event and was controlled effectively with small doses of opioid analgesia administered intravenously.
The effect of general anesthesia using isoflurane and epidural anesthesia using ropivacaine was shown on hemostasis in hepatic patients. General anesthesia showed a marked significant increase in specific parameters compared to epidural anesthesia. Thus epidural ropivacaine anesthesia provided better hemostatic stability, especially in hepatic patients [6]. In our case, the epidural anesthesia did not affect liver enzyme parameters.
We presented the first case of sickle cell anemia (SCA), beta (+) thalassemia, and Crohn's disease, which was effectively anesthetized for laparoscopic cholecystectomy using thoracic epidural anesthesia. According to our experience, the results were excellent without severe complications. Ultimately, we considered laparoscopic cholecystectomy using thoracic epidural anesthesia that resulted in a shorter hospital stay with rare postoperative complications rather than an open operation using general anesthesia in patients with sickle cell disease. We suggest that this may be the procedure of choice in the treatment of cholelithiasis in such patients.
References
2. Haberkern CM, Neumayr LD, Orringer EP, Earles AN, Robertson SM, Black D, et al. Preoperative Transfusion in Sickle Cell Disease Study Group. Cholecystectomy in sickle cell anemia patients: perioperative outcome of 364 cases from the National Preoperative Transfusion Study. Blood. 1997; 89:1533–1542. PMID: 9057634.
3. Origa R, Galanello R. Pathophysiology of beta thalassaemia. Pediatr Endocrinol Rev. 2011; 8(Suppl 2):263–270. PMID: 21705976.
4. Al-Mulhim AS, Al-Mulhim AA. Laparoscopic cholecystectomy in 427 adults with sickle cell disease: a single-center experience. Surg Endosc. 2009; 23:1599–1602. PMID: 19444510.

5. Lee JH, Huh J, Kim DK, Gil JR, Min SW, Han SS. Laparoscopic cholecystectomy under epidural anesthesia: a clinical feasibility study. Korean J Anesthesiol. 2010; 59:383–388. PMID: 21253374.

6. Khafagy HF, Hussein NA, Radwan KG, Refaat AI, Hafez HS, Essawy FM, et al. Effect of general and epidural anesthesia on hemostasis and fibrinolysis in hepatic patients. Hematology. 2010; 15:360–367. PMID: 20863432.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download