Introduction
Measurement of end-tidal carbon dioxide pressure (P
ETCO
2) by capnometry is a useful non-invasive method to estimate arterial carbon dioxide partial pressure (P
aCO
2) during general anesthesia. Several factors have been reported to affect P
ETCO
2 and to increase the arterial to end-tidal carbon dioxide pressure gradient (P
a-ETCO
2) [
1]. For example, Trendelenburg positioning and CO
2 pneumoperitoneum have been found to decrease functional residual capacity (FRC) and to increase dead space ventilation. These maneuvers, performed either alone or together, may affect P
a-ETCO
2 [
2-
4]. In addition, age has been found to contribute to an increase in P
a-ETCO
2 [
2].
Robot-assisted laparoscopic surgery has become an alternative approach to open techniques in many surgical fields. Robot-assisted laparoscopic prostatectomy (RALP) was found to improve surgical outcomes and to reduce complications compared with open radical prostatectomy [
5,
6]. However, RALP requires pneumoperitoneum in the steep Trendelenburg position, which can cause significant changes in respiratory physiology. P
a-ETCO
2 was shown to increase gradually with time during pneumoperitoneum in the Trendelenburg position [
7] and a rise in P
a-ETCO
2 has been observed in elderly patients during gynecologic laparoscopy surgery [
8]. To the best of our knowledge, the relationship between age and P
a-ETCO
2 in the steep Trendelenburg position with pneumoperitoneum has not been determined. Therefore, we evaluated the correlation between age and P
a-ETCO
2 in patients undergoing RALP.
Materials and Methods
We enrolled 92 consecutive male patients (ASA physical status I and II) undergoing elective RALP between May to December 2009. Patients with cardiopulmonary disease and/or abnormal pulmonary function test results were excluded. Patients were divided into 2 groups by age; a middle-aged group (45-65 years) and an elderly group (> 65 years). The study protocol was approved by our Institutional Review Board, and all patients provided written informed consent.
All patients were premedicated with oral midazolam (7.5 mg) 1 h before induction of anesthesia. Upon arrival in the operating room, patients were monitored by ECG, pulse oximetry, and non-invasive automated arterial blood pressure tracking. Anesthesia was induced with thiopental (4-5 mg/kg) and vecuronium (0.1 mg/kg), and the trachea was intubated with an 8.0-mm endotracheal tube. Anesthesia was continued using sevoflurane (1-1.5 MAC) and additional boluses of vecuronium (1-2 mg) and fentanyl (1-1.5 µg/kg) to maintain stable hemodynamic parameters (i.e., heart rate and blood pressure variations < 20% of preinduction values). The lungs were ventilated with a ventilator (Primus; Dräger Medical, Lübeck, Germany) operating in the volume control mode. Ventilator settings were a tidal volume of 10 ml/kg, an inspiratory: expiratory ratio of 1 : 2, a fraction of inspired O2 (FIO2) of 0.5, and an air and inspiratory fresh gas flow of 2 L/min. The respiratory rate was adjusted to hold the PETCO2 between 30 and 38 mmHg. The end-tidal concentration of anesthesia gases and PETCO2 were monitored using the side stream method (M1026B Anesthetic Gas Module; Philips, Boeblingen, Germany).
After induction of anesthesia, a 20-G radial arterial catheter was inserted to obtain hemodynamic measurements and to permit blood sampling. Normothermia (about 36℃) was maintained using a forced-air warming system. The abdominal cavity was insufflated with CO
2 gas at a pressure of 15 mmHg, and the trocar and cannulae were located at the classical points [
9] in the supine position. Each patient was slowly moved into a steep Trendelenburg position (30° from horizontal; the maximal angle allowed by the operating table). RALPs were performed using the da Vinci Robot Surgical System (Intuitive Surgical, Sunnyvale, CA). Intra-abdominal pressure was automatically maintained at 10-13 mmHg. At the end of the procedure, each patient was returned to the supine position and the CO
2 pneumoperitoneum was released. When the operation had completed, the patient was awakened and extubated in the operating room.
Heart rate, mean arterial pressure, peak inspiratory pressure, lung compliance, minute ventilation, and PETCO2 were measured 10 min after intubation in the supine position without pneumoperitoneum (T0; baseline); and 10 (T1), 60 (T2), and 120 (T3) min after pneumoperitoneum in the 30° Trendelenburg position. Arterial oxygen partial pressure (PaO2) and PaCO2 were measured by arterial blood gas analysis (GEM Premier 3000; Instrumentation Laboratory, Lexington, MA) at each time point. Pa-ETCO2 was calculated as the difference between the measured PaCO2 and PETCO2.
Based on a preliminary study, we estimated that data from 84 patients were required to detect a correlation coefficient above 0.3 between age and Pa-ETCO2, with a statistical power of 80% and a type I error of 0.05 (the null hypothesis correlation is 0.0 and the alternative hypothesis correlation 0.3). To compensate for possible exclusions (10%), 92 patients were enrolled in the present study. All statistical analyses were performed using SPSS for Windows Version 18.0 (SPSS Inc., Chicago, IL). Data are expressed as mean ± SD. Changes in parameters (heart rate, mean arterial pressure, peak inspiratory pressure, lung compliance, minute ventilation, PaO2, PETCO2, PaCO2, and Pa-ETCO2) over time were assessed using a linear mixed model to evaluate within- and between-group differences. The relationship between age and Pa-ETCO2 at each time point was determined using the Pearson correlation test and by performing a simple linear regression analysis. In addition, the relationships and interactions between Pa-ETCO2 and patient or anesthetic parameters (age, body mass index, heart rate, mean arterial pressure, minute ventilation, peak inspiratory pressure, and PaO2) with time (duration of pneumoperitoneum in the Trendelenburg position) were tested using a linear mixed model with adjustment for heart rate, mean arterial pressure, peak inspiratory pressure, minute ventilation, and PaO2. A P value less than 0.05 was considered statistically significant.
Results
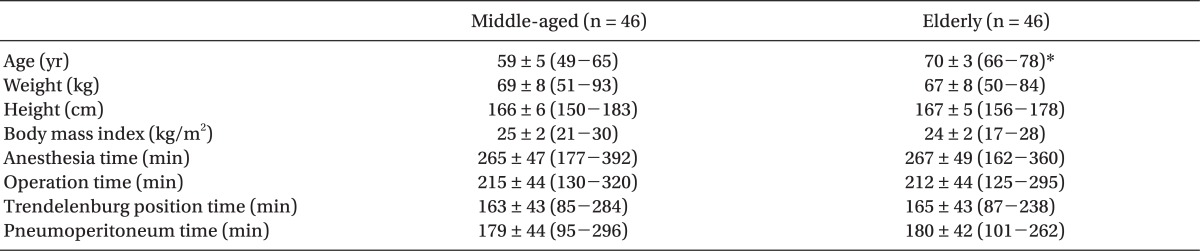
Ninety-two male patients were enrolled (46 in the middle-aged group and 46 in the elderly group). No patient was excluded from the study. The numbers of data sets were 92 from T0, T1, and T2; and 84 from T3. Data sets were not collected from 8 patients at T3 (4 in either group) because the procedures were completed within 120 min. Except for age, there was no significant between-group difference in any physical characteristic or surgical duration (
Table 1).
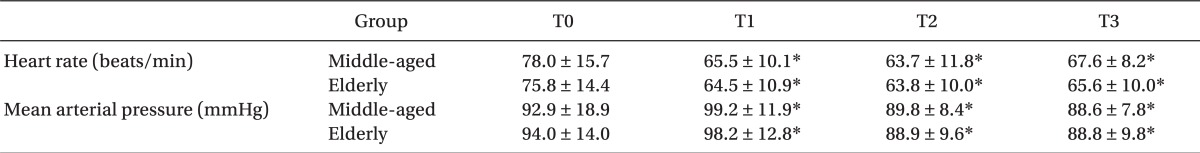
Hemodynamic data are shown in
Table 2. Heart rate and mean arterial pressure changed significantly after pneumoperitoneum in the steep Trendelenburg position (from T1 to T3) compared with the baseline values at T0 in both groups, with no significant between-group difference being evident.
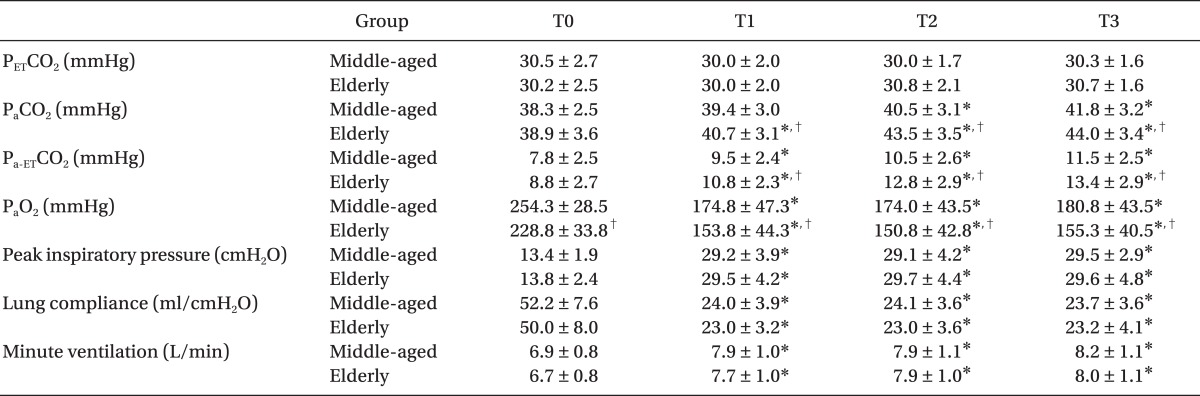
Table 3 shows changes in peak inspiratory pressure, lung compliance, minute ventilation, P
aO
2, P
ETCO
2, P
aCO
2, and P
a-ETCO
2 at each time point. There was no significant between-group difference in any of peak inspiratory pressure, lung compliance, minute ventilation, or P
ETCO
2. After CO
2 insufflation in the steep Trendelenburg position, these values, except for P
ETCO
2, changed significantly compared with the baseline values at T0. In addition, P
aO
2, P
aCO
2, and P
a-ETCO
2 changed significantly from T0 after CO
2 insufflation in the steep Trendelenburg position, with all 3 parameters showing significant between-group differences.
Although P
ETCO
2 was maintained constant throughout surgery, P
aCO
2 and P
a-ETCO
2 increased gradually with time during pneumoperitoneum in the steep Trendelenburg position. The magnitudes of these increases were significantly greater in the elderly than in the middle-aged group (
Table 3).
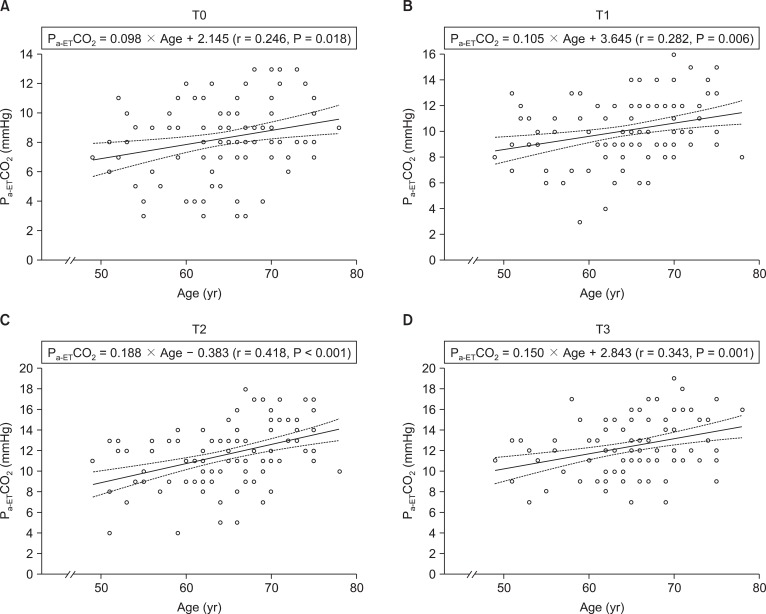
We observed a significant correlation between age and P
a-ETCO
2 at each time point (
Fig. 1). The regression coefficients were 0.098 (P = 0.018) at T0, 0.105 (P = 0.006) at T1, 0.188 (P < 0.001) at T2, and 0.150 (P = 0.001) at T3.
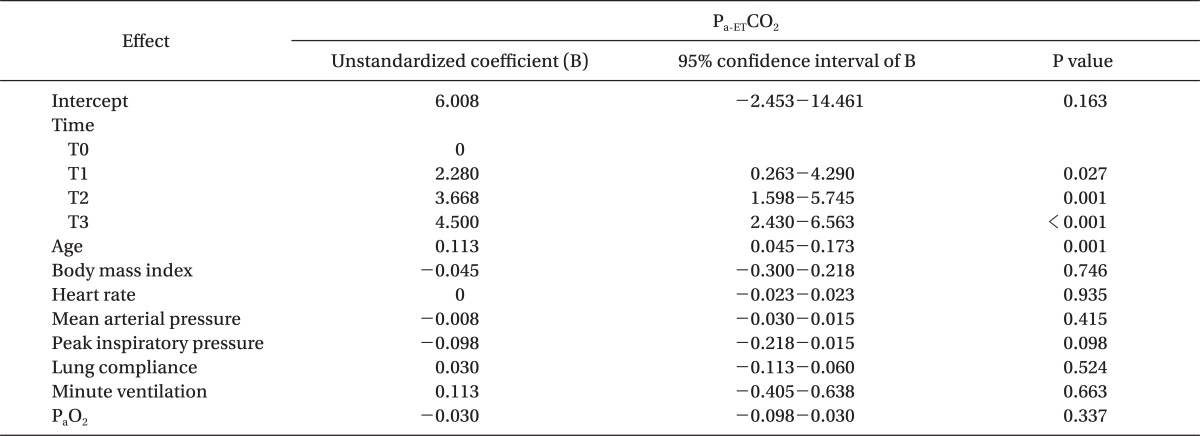
A linear mixed model was used to evaluate the relationships and interactions between P
a-ETCO
2 and patient or anesthetic factors (age, body mass index, heart rate, mean arterial pressure, minute ventilation, peak inspiratory pressure, and P
aO
2) with respect to duration of pneumoperitoneum in the Trendelenburg position, because of the absence of some T3 data sets. We found that P
a-ETCO
2 was significantly associated with patient age (regression coefficient 0.113, P = 0.001) and with duration of pneumoperitoneum in the Trendelenburg position (regression coefficient 2.280, P = 0.027 at T1; regression coefficient 3.668, P = 0.001 at T2; and regression coefficient 4.500, P < 0.001 at T3) (
Table 4). However, there was no significant interaction between age and duration of pneumoperitoneum in the Trendelenburg position (P = 0.090).
Discussion
We have shown here that Pa-ETCO2 increased more in elderly than in middle-aged males during placement in the steep Trendelenburg position with CO2 pneumoperitoneum, and that a significant relationship between age and Pa-ETCO2 in male patients undergoing RALP was evident.
RALP has several advantages compared with open retropubic radical prostatectomy, including easier accessibility, decreased blood loss, reduced postoperative pain, and a lower complication rate [
6]. However, RALP requires pneumoperitoneum and Trendelenburg positioning, both of which, either alone or in combination, affect P
a-ETCO
2 [
2-
4]. A cephalad displacement of diaphragm resulting from CO
2 pneumoperitoneum and placement in the steep Trendelenburg position enhances atelectasis formation, decreases lung volume and lung compliance [
10-
12]. The resultant enhancement of atelectasis formation may lead to increase in P
a-ETCO
2. This is supported by previous reports that P
a-ETCO
2 was a good predictor of atelectasis formation, and the absorption of CO
2 during pneumoperitoneum had no effect on P
a-ETCO
2 [
13].
Increases in P
a-ETCO
2 have been reported during pneumoperitoneum in the Trendelenburg position. For example, men undergoing RALP showed a mean 3.0 mmHg increase in P
a-ETCO
2 after 120 min in the steep Trendelenburg position with CO
2 pneumoperitoneum [
4], and women undergoing laparoscopic hysterectomy in the Trendelenburg position showed a mean 1.5 mmHg increase in P
a-ETCO
2 [
3]. In addition, P
ETCO
2 differed significantly from P
aCO
2 during prolonged laparoscopic colon surgery in the Trendelenburg position [
7]. We observed a mean 4.1 mmHg increase in P
a-ETCO
2 after 120 min of pneumoperitoneum and steep Trendelenburg positioning. Moreover, linear mixed model analysis showed a significant relationship between P
a-ETCO
2 and duration of pneumoperitoneum in the Trendelenburg position. Our results are consistent with previous findings showing that P
a-ETCO
2 increased during pneumoperitoneum in the Trendelenburg position [
3,
4], although both studies in the nature of surgery and patient characteristics. Our results indicate that measurements of P
ETCO
2 may underestimate P
aCO
2 under certain circumstances, and that ventilator settings based on capnometry in anesthetized patients should be carefully determined.
P
a-ETCO
2 during general anesthesia has been reported to be affected by age. For example, significant correlations were observed between age and P
a-ETCO
2 in patients in the supine, lateral, prone, and Trendelenburg positions [
2]. In the cited study, the relationship between age and P
a-ETCO
2 was assessed separately in supine patients and those in the Trendelenburg groups, whereas we assessed the relationship at different time points in patients placed in the Trendelenburg position. Moreover, P
a-ETCO
2 was found to increase gradually after CO
2 pneumoperitoneum in the Trendelenburg position only in elderly patients [
8]. Although the cited study compared P
a-ETCO
2 between elderly patients and those of other age groups at the same time point, the work did not evaluate the relationship between age and P
a-ETCO
2. In contrast, we found that the magnitude of the increase in P
a-ETCO
2 was significantly greater in elderly than in middle-aged men, and linear mixed model analysis showed a significant relationship between age and P
a-ETCO
2. Although differences in study design are evident, our results are in agreement with previous findings showing that P
a-ETCO
2 increases with age in patients under general anesthesia [
2,
8].
In addition, we used linear mixed model analysis to assess the relationships and interactions between Pa-ETCO2 and patient or anesthetic factors, on the one hand, and duration of pneumoperitoneum in the Trendelenburg position, on the other. This analysis showed that the magnitude of Pa-ETCO2 was significantly related to both age and duration of pneumoperitoneum in the Trendelenburg position. However, the interaction between age and duration of pneumoperitoneum in the Trendelenburg position was not significant. These results suggest that aging may increase Pa-ETCO2 during general anesthesia, with or without pneumoperitoneum in the Trendelenburg position.
The possible mechanism of higher gradient in the elderly group is unclear, but it may be explained by the age-related respiratory changes. It is well known that aging is intimately associated with various changes in the respiratory system, including structural and functional changes in the lungs. In terms of lung volume, aging increases residual volume, closing volume, and FRC [
14]. Although atelectasis does not increase with age during general anesthesia, the amount of perfusion to low ventilation/perfusion regions increases with age due to increased airway closure [
15,
16]. Therefore, these age-related changes in respiratory function are likely to increase P
a-ETCO
2 during general anesthesia.
The magnitude of P
a-ETCO
2 is influenced by many factors, including pulmonary disorders, anesthesia, and cardiac output [
1,
17,
18]. To minimize the effects of such factors, we included only healthy patients without cardiopulmonary disease and/or abnormal pulmonary function test results. In addition, anesthetic management was standardized in terms of anesthetic drugs, ventilator settings, and patient position. Thus, the effect of anesthetic conditions on P
a-ETCO
2 may be expected to be the same in all patients. Finally, cardiac output could change P
aCO
2 and P
ETCO
2 in the same direction, but the change in P
a-ETCO
2 is variable in direction and magnitude [
19]. In addition, P
a-ETCO
2 remains stable when cardiac output is constant [
20]. The steep Trendelenburg position with pneumoperitoneum was recently reported to cause no change in cardiac output during RALP [
21,
22]. Although cardiac output was not measured in the present study, the observed increase in P
a-ETCO
2 was not likely affected by this factor.
This study had several limitations. First, the data from our homogeneous group of patients may be specific to an older male population undergoing RALP. Because prostate cancer usually occurs in older men (mean age at diagnosis is 67 years) [
23], all patients enrolled in this study were men with a narrower age range (49-78 years) and with a smaller mean age difference between the groups (11 years), when compared with previous studies [
2,
7,
8]. Therefore, the gender and age range may limit the generalization of our data. Second, arterial blood gas analyses were not performed on patients in the Trendelenburg position or with pneumoperitoneum alone. In our institute, urologic surgeons perform CO
2 insufflation before patients are placed in the Trendelenburg position. Therefore, additional time would have been required to analyze arterial blood gases in such patients, which would have unethically prolonged the duration of anesthetic management. Third, we did not conduct measurements in the non-anesthetized state because the impact of anesthesia on such parameters has been previously reported [
3].
In conclusion, we found that the magnitude of Pa-ETCO2 increased gradually with time during pneumoperitoneum in the steep Trendelenburg position, and rose with advancing patient age. Under such specific circumstances, ventilator settings based on capnometry in elderly patients should be carefully determined and PaCO2 should be measured periodically by arterial blood sampling during surgery.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download