Abstract
Stress-induced cardiomyopathy, also referred to Takotsubo cardiomyopathy or apical ballooning syndrome presents in perioperative period. We demonstrated a case of Takotsubo cardiomyopathy recognized after general anesthesia for bladder hydrodistension therapy as ambulatory surgery, which we surmise was due to inadequate blockage of surgical stress and sympathetic discharge against noxious stimulus during ambulatory anesthesia.
Ambulatory surgery has progressed from the practice of performing simple procedures on healthy outpatients to encompassing a broad spectrum of major procedures in outpatients with complex preexisting medical conditions. The choice of anesthetic technique for ambulatory surgery depends on both surgical and patient factors. The elaborate balance between quality, safety, efficiency and the cost of drugs is a key factor in choosing an anesthetic technique for ambulatory surgery. Although one of the most important factors for ambulatory anesthesia is rapid recovery, poor blockade of the stress response to noxious stimuli due to sevoflurane-based anesthesia can result in failure of sympathetic discharge blockade and an increased incidence of myocardial ischemia and cardiac dysfunction [1]. Apical ballooning syndrome (ABS), also called Takotsubo cardiomyopathy is a cardiac syndrome characterized by an acute onset of transient distinguishing left ventricular dysfunction associated with physical or emotional stress [2,3]. We describe a patient with this condition after general anesthesia for hydrodistension of bladder for interstitial cystitis in an university hospital-based ambulatory surgery unit.
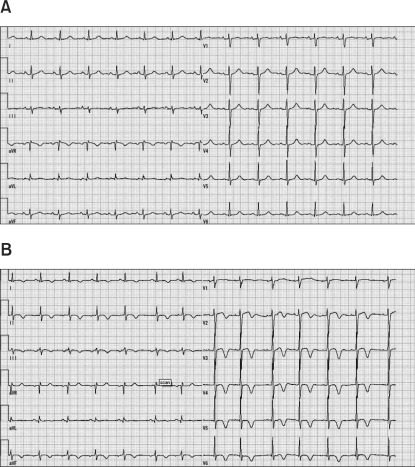
A 70-year-old female (weight, 42 kg; height 149 cm) was scheduled to undergo bladder hydrodistension therapy for interstitial cystitis [4]. She had a previous medical history of gastroesophageal reflux disease and lung cancer for which she had undergone a lobectomy 6 years previously and chemotherapy. Although she also had undergone hydrodistension of bladder under spinal anesthesia 2 years ago, she had a preference for general anesthesia this time. Routine preoperative laboratory investigations, electrocardiogram (ECG) (Fig. 1A) and chest X-ray showed no abnormalities. Preoperative evaluation revealed no remarkable risk factors. Thus, the patient was considered as ASA PS 1 at the preoperative consult and we planned that she would undergo ambulatory surgery under general anesthesia.
Anesthesia was induced with 80 mg of propofol and maintained with sevoflurane at 2-3% in 50% O2 with 50% air via laryngeal mask airway. BIS value was maintained between 50 and 60. 50 mg of flurbiprofen was administered for postoperative analgesia soon after anesthesia induction. Either opioids or muscular relaxants were not administered. The surgery proceeded uneventfully until the bladder was extended when her heart rate increased from 80 beats/min to 140 beats/min and her blood pressure raised from 100/50 mmHg to 190/120 mmHg. Inhalation bolus of sevoflurane (8% sevoflurane with 8 L fresh gas flow) was administered for about 5 minutes and her vital signs were stabilized. No ECG abnormality was observed. After the incident, the surgery proceeded without any particular events and she recovered from general anesthesia 10 minutes after the surgery. She was transferred to a post anesthesia care unit (PACU). On arrival in the PACU, she did not have any complaints. Two hours after the surgery she began to complain chest discomfort and lower abdominal pain in the PACU. ECG showed T wave change (Fig. 1B) compared to baseline ECG (Fig. 1A) taken 29 days before surgery. HR and BP were 110 beats/min and 95/62 mmHg respectively. Although this was planned as ambulatory surgery, the patient was admitted to the ward for further follow-up. Five hours after the surgery she complained chest discomfort and chest pain again and another ECG clearly showed T wave inversion (data not shown). Echocardiography indicated the akinesis of the apical and mid segment with the basal function preserved, which were consistent with Takotsubo cardiomyopathy [7]. Coronary angiography showed no evidence of acute coronary syndrome (ACS). Laboratory studies including CK, CK-MB, Troponin-I and TnT also indicated no evidence of ACS. The concentration of plasma catecholamines were not examined. Heparin infusion was introduced for prophylaxis of left ventricular thrombosis but hematuria made it impossible to continue. She did not undergo supportive therapy including catecholamine infusion or administration of β-blockers or ACE inhibitors because the hemodynamics were stable. She did not suffer recurrence of the symptoms and she was discharged on the postoperative day 10.
In this report, we presented a patient who developed Takotsubo cardiomyopathy or ABS after hydrodistension of bladder, which was originally scheduled as an ambulatory surgery.
Takotsubo cardiomyopathy was first reported in the early 1990s in Japan [2] and named after its characteristic ventriculographic features. This disorder mainly affects postmenopausal females who experience acute physical or emotional stress [3]. The first symptoms and abnormalities on the electrocardiogram are indistinguishable from ACS [6]. Thus, Takotsubo cardiomyopathy is an important differential diagnosis of ACS. The first symptoms in most patients are chest pain and dyspnea and the most common abnormalities on the ECG are ST-segment elevation and T wave inversion as observed in this case (Fig. 1A and 1B). Echocardiogram typically shows hypokinesis or akinesis of the mid and apical segment of the left ventricle and preserved systolic function of the basal segment [7]. Moreover, the coronary angiography usually shows normal coronary arteries or only mild luminal stenosis [9]. Thus, the wall motion abnormalities that extend beyond the distribution of single coronary artery and almost normal cardioangiography, leads to the diagnosis of Takotsubo cardiomyopathy as well as in our case. Prognosis is generally favorable, with an in-hospital mortality of 1.1%.
There are several case reports of perioperative Takotsubo cardiomyopathy. Takotsubo cardiomyopathy have been reported during eye surgery, cholecystectomy, hysterectomy, hernia repair, electroconvulsive therapy, carotid endarterectomy and induction of anesthesia [8]. Excessive discharge of catecholamines with activation of cardiac receptors and discrepancy in the distribution of sympathetic nerve endings and their receptors could explain the wall motion abnormalities [9], but pathophysiological mechanism is still uncertain [3]. Although the optimal management of Takotsubo cardiomyopathy has not been established, supportive therapy with catecholamine and β-blockers leads to spontaneous recovery in most cases.
Ambulatory anesthesia has grown and continues to grow in the ever-changing medical environment. In ambulatory surgery, postoperative nausea and vomiting (PONV) and poorly controlled postoperative pain are common reasons for delayed discharge, patient's dissatisfaction and unanticipated hospital admissions of outpatients. As opioid is one of the major PONV risk factors, its use in the ambulatory anesthesia is often replaced by multimodal pain management adopting local anesthetics and nonsteroidal anti-inflammatory drugs [10]. The α2-adrenergic agonist dexmedetomidine reduces central sympathetic flow and has been shown to produce anxiolysis and sedation [11]. Dexmedetomidine significantly decreased anxiety levels and reduced the requirements for supplemental analgesic medications when given before intravenous regional anesthesia with minimal respiratory depression. It is reported that the slower recovery from dexmedetomidine-induced sedation, as well as the occurrence of bradycardia, has limited its use in the ambulatory setting [12]. Although this technique can eliminate some of the undesirable effects of opioids, it sometimes provides poor blockade of the stress response unless the local anesthetics provides profound neural blockade of the affected area [1]. In this case, at the time of hydrodistension, sharp increase of HR and BP was observed due to strong sympathetic discharge. In the present case, any opioids were not administrated to the patient to reduce the possibility of occurrence of PONV. It is reported the blunting sympathetic responses after surgical incision (MACBAR) of sevoflurane without opioid or nitrous oxide is 2.8% [13]. The alveolar concentration of sevoflurane was at most 3% at the time of bladder distension. Moreover, the effects of sevoflurane on the surgical noxious stimulation-induced norepinephrine response were inversely proportional to the dose. Sevoflurane does not suppress but augments the adrenergic nervous system responses to surgical noxious stimulation [14]. Thus, the anesthesia in the present case did not might not block the sympathetic discharge induced by bladder distension. In fact, the patient uneventfully underwent the same operation previously under spinal anesthesia. Complete blockage contributed to suppress the nociceptive response and innervation of bladder. Central neuraxial blockade such as sacral block after induction of general anesthesia or use of opioid such as remifentanil might have prevented the incident in this case.
In summary, we reported a case of unexpected Takotsubo cardiomyopathy under general anesthesia originally planned as ambulatory surgery. Improvement of surgical technique is making the procedures less invasive, but Takotsubo cardiomyopathy can occur in various situations. Anesthesiologists who participate in ambulatory anesthesia should be aware of the risk factors inherent in the patient, procedure, and anesthetic management for developing this syndrome, and carefully consider strategy of intra- and post-operative analgesia in order to prevent noxious stimulus [15].
References
1. Fleisher LA, Beckman JA, Brown KA, Calkins H, Chaikof E, Fleischmann KE, et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery): developed in collaboration with the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. Circulation. 2007; 116:e418–e499. PMID: 17901357.

2. Dote K, Sato H, Tateishi H, Uchida T, Ishihara M. Myocardial stunning due to simultaneous multivessel coronary spasm: a review of 5 cases. J Cardiol. 1991; 21:203–214. PMID: 1841907.
3. Wittstein IS, Thiemann DR, Lima JA, Baughman KL, Schulman SP, Gerstenblit G, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005; 352:539–548. PMID: 15703419.

4. Ito T, Ueda T, Honma Y, Takei M. Recent trends in patient characteristics and therapeutic choices for interstitial cystitis: analysis of 282 Japanese patients. Int J Urol. 2007; 14:1068–1070. PMID: 18036041.

5. Afonso L, Bachour K, Awad K, Sandidge G. Takotsubo cardiomyopathy: pathogenetic insights and myocardial perfusion kinetics using myocardial contrast echocardiography. Eur J Echocardiogr. 2008; 9:849–854. PMID: 18579499.

6. Prasad A. Apical ballooning syndrome: an important differential diagnosis of acute myocardial infarction. Circulation. 2007; 115:e56–e59. PMID: 17283269.
7. Gianni M, Dentali F, Grandi AM, Sumner G, Hiralal R, Lonn E. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J. 2006; 27:1523–1529. PMID: 16720686.

8. Jabaudon M, Bonnin M, Bolandard F, Chanseaume S, Dauphin C, Bazin JE. Takotsubo syndrome during induction of general anaesthesia. Anaesthesia. 2007; 62:519–523. PMID: 17448067.

9. Lyon AR, Rees PS, Prasad S, Poole-Wilson PA, Harding SE. Stress (Takotsubo) cardiomyopathy--a novel pathophysiological hypothesis to explain catecholamine-induced acute myocardial stunning. Nat Clin Pract Cardiovasc Med. 2008; 5:22–29. PMID: 18094670.

10. Gan TJ, Meyer TA, Apfel CC, Chung F, Davis PJ, Habib AS, et al. Society for Ambulatory Anesthesia guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2007; 105:1615–1628. PMID: 18042859.

11. Carollo DS, Nossaman BD, Ramadhyani U. Dexmedetomidine: a review of clinical applications. Curr Opin Anaesthesiol. 2008; 21:457–461. PMID: 18660652.

12. Renes J, Glass PS, Lubarsky D, McEnvoy M, Martinez-Ruiz R. Intravenous anesthetics. Miller's anesthesia. 2009. 7 ed. New York: Churchill Livingstone;p. 719–764.
13. Albertin A, Casati A, Bergonzi P, Fano G, Torri G. Effects of two target-controlled concentrations (1 and 3 ng/ml) of remifentanil on MAC (BAR) of sevoflurane. Anesthesiology. 2004; 100:255–259. PMID: 14739797.
14. Segawa H, Mori K, Murakawa M, Kasai K, Shirakami G, Adachi T, et al. Isoflurane and sevoflurane augment norepinephrine responses to surgical noxious stimulation in humans. Anesthesiology. 1998; 89:1407–1413. PMID: 9856715.

15. Cohen MM, Duncan PG, Tate RB. Does anesthesia contribute to operative mortality? JAMA. 1988; 260:2859–2863. PMID: 3184350.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download