Abstract
Lumbar plexopathy is characterized by an abrupt onset of sensory disturbances, weakness, and loss of deep tendon reflexes of lower extremities. The various causes of lumbar plexopathy include trauma, infections, space-occupying lesion, vascular diseases, metabolic diseases, and the use of drugs such as heroin. Postoperative rhabdomyolysis occurs secondary to prolonged muscle compression due to surgical positioning. Herein, we report a case of lumbar plexopathy, complicating an injury to the paraspinal muscle and iliopsoas muscle that occurred in the flexed lateral decubitus position following radical nephrectomy.
Lumbar plexopathy can occur as the result of direct trauma to the lumbar plexus, space-occupying lesions in the peritoneal cavity, complications after aortic surgery, and metabolic diseases [1,2]. Patients who undergo surgery under general anesthesia or regional anesthesia in the lateral decubitus, prone, or lithotomy positions experience complications that damage the soft tissues of the muscles or nerves [3-6]. There have been reports of patients who underwent a nephrectomy in the lateral decubitus position, where severe pressure on the opposite paraspinal muscles or gluteal muscles during surgery induced rhabdomyolysis [3,7]. We report a patient who underwent a nephrectomy in the lateral decubitus position, experienced injury in the opposite paraspinal and iliopsoas muscles, and also evidenced lumbar plexopathy.
A 58 year-old male patient, 171 cm in height and 75 kg in weight was diagnosed with a ureter tumor invading the left kidney. He was admitted into the Urology Department. Since three years ago, the patient had been taking oral medication for diabetes mellitus and hypertension. He had no other previous history. In the preoperative evaluation, the patient's chest X-ray and electrocardiogram was within normal range. His laboratory examination showed Hb 12.8 g/dl, hematocrit 37.3%, SGOT/SGPT 16/17 IU, BUN/Cr 20/1.0 mg/dl, and glucose 127 mg/dl. Thirty minutes before surgery, the patient was premedicated with 3 mg of midazolam and 0.2 mg of glycopyrrolate via intramuscular injection. In the operating room, the electrocardiogram, noninvasive arterial blood pressure cuff, pulse oximeter, capnograph, and bispectral index system (BIS, Aspect Medical, Norwood, MA, USA) were attached in order to monitor the patient.
To induce anesthesia, 250 mg of thiopental sodium and 10 mg of vecuronium bromide were injected intravenously, after which endotracheal intubation was performed. Anesthesia was maintained with 50% O2 (mixed with air), desflurane 4.0-6.0%, and remifentanil 0.05-0.1 µg/kg/min. The patient was laid in the right lateral decubitus position. The kidney rest was raised and the flexion of the operating table was set at 30°. The patient's vital signs during the surgery were maintained in the normal range. Blood loss was approximately 900 ml, and urine output was 760 ml. The total amount of fluids administered to the patient was 6,050 ml of crystalloid solution and 500 ml of colloid solution. 420 ml of packed red blood cells were transfused. The operative time was 8 hours and 35 min. After the surgery ended, we reversed the effects of muscle relaxation and made sure the patient had adequate spontaneous breathing. We then removed the endotracheal tube. Afterward, the patient was transferred to the intensive care unit (ICU). Postoperative pain was controlled by using a 2-day intravenous patient-controlled analgesia regimen (IV-PCA, medical, Auto Fuser, Korea) that included 700 µg of fentanyl and 300 mg of tramadol. On the day of the surgery, the patient complained of pain in the surgical site, the right lumbar region, and the right lower extremity. So his pain was controlled via the intravenous administration of 50 mg of tramadol.
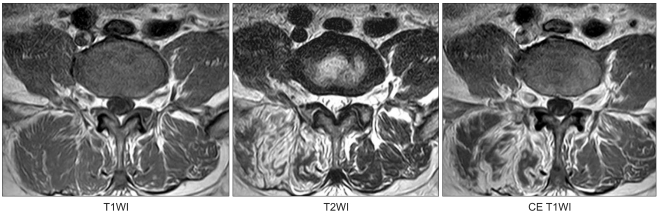
On postoperative day 1, the laboratory tests showed BUN/Cr 21/0.8 mg/dl and a urine output of 2,900 ml, and the urine test showed light yellow urine. Other than hematuria, the findings were normal. On postoperative day 2, the patient complained of pain in the right lumbar and anterior thigh region and weakness in the right lower extremity. No swelling or other abnormalities were noted in the skin of either the lumbar or thigh region. BUN/Cr increased to 44/2.0 mg/dl, and the urine output was 1,400 ml. On postoperative day 3, BUN/Cr was 53/2.9 mg/dl, and urine output was 2,400 ml. On postoperative day 5, the neurologic evaluation showed reduced perception and nociception in the anterior medial side of the right thigh region, as well as a reduced ability to flex the right hip joint and extend the right knee joint. The deep tendon reflex of the knee also decreased. For pain treatment, gabapentin 900 mg, amitriptyline 10 mg, and tramadol 100 mg were administered orally. On postoperative day 9, lumbar radiculopathy was suspected, so a lumbar spine MRI was carried out. We detected diffuse swelling and high signal intensity in the right parapsinal muscles from T12-L1 to L5-S1 and iliopsoas muscles (Fig. 1). There was no finding of a lumbar herniated nucleus pulposus or spinal stenosis. On postoperative day 14, we observed on the electromyography severe denervation potentials in the right iliopsoas muscles and the paraspinal muscles at L2-S1 and mild denervation potentials in the right thigh muscles. Thus, we diagnosed the high likelihood of right lumbar plexopathy.
From postoperative day 5 to day 12, BUN/Cr decreased from 57/3.3 mg/dl to 25/2.1 mg/dl, and the patient's urine output per day was 3,100-4,600 ml. From postoperative day 17, the muscle weakness in the patient's right lower extremity began to improve, and by postoperative day 20 the patient was able to practice ambulation. On postoperative day 27, the patient was discharged. It has been 3 months since the surgery, and the patient has recovered from muscle weakness in his right lower extremity; only symptoms of dysesthesia remained. The patient is currently taking gabapentin 600 mg and tramadol 100 mg.
Lumbar plexopathy can occur idiopathically, but is generally caused by direct trauma to the lumbar plexus, complications with surgery, radiotherapy, infection, metabolic diseases, or ischemia. Characteristics of lumbar plexopathy include paresthesia, muscle weakness, and reduced deep tendon reflexes [2]. Muscle injury from trauma or other causes can induce rhabdomyolysis, which has been reported to be related to brachial plexopathy and lumbosacral plexopathy [8,9].
In a urologic surgery for nephrectomy in the lateral decubitus position, the surgical table is flexed and the kidney rest is used to preserve the operative field. However, such positions put pressure on the opposite paraspinal and gluteal muscles and can induce rhabdomyolysis. In laparoscopic nephrectomies which have long operative times, the occurrence rate of rhabdomyolysis may increase. Reisiger et al. [7] reported that laparoscopic nephrectomies have a 1% rhabdomyolysis occurrence rate. There have also been reported cases of lumbosacral plexopathy due to complications of rhabdomyolysis in the gluteal region [9]. Rhabdomyolysis is characterized by the breakdown of the striated muscle, and the muscle cell contents, such as electrolytes, myoglobin, and creatine kinase leak into the bloodstream [10]. In cases of severe rhabdomyolysis, weakness in the extremities, myalgia, edema, and pigmenturia without hematuria occur. Rhabdomyolysis is diagnosed in cases in which there is no myocardial ischemia, but creatine phosphokinase (CPK) levels are 5 times the normal range, or in cases in which myoglobinuria is present. As a serious complication in rhabdomyolysis, acute renal injury can occur, and renal failure can have a poor prognosis.
In the case presented herein, the nephrectomy in the right lateral decubitus position took 8 hours and 35 min. Immediately after surgery, the patient complained of pain in the right thigh region and in the right lower extremity. Also on postoperative day 2, the patient complained of continuous pain and weakness in the right lower extremity. Because of the patient complaints of his continuous symptoms, radiculopathy was suspected. On postoperative day 9, we took a lumbar MRI, with which we were able to confirm injury to the right paraspinal and ileopsoas muscles. From the electroneurography and electromyography, lumbar plexopathy was diagnosed. The principal shortcoming of the presented case report is that the diagnosis was delayed because the initial patient symptoms were regarded as temporary. When the patient initially complained of his symptoms, we should have suspected injury in the paraspinal or gluteal muscles and we should have measured CPK and myoglobin levels in the blood. Reisiger et al. [7] stated that all 7 patients who had rhabdomyolysis after laparoscopic nephrectomy complained of severe pain in the opposite lumbar and gluteal region immediately after surgery. Factors leading to rhabdomyolysis from surgery include long operating time, positioning in the lateral decubitus position, and the body mass index of the patient. Therefore, when factors that can cause rhabdomyolysis are present and the patient complains of pain in the pressed area, the blood CPK level must first be measured to check for the presence of rhabdomyolysis. From the lumbar MRI and electromyography, we consider the pressure injury on the paraspinal and iliopsoas muscles to have caused lumbar plexopathy. In rhabdomyolysis, increases in blood CPK and myoglobin levels constitute important test findings; additionally, MRI tests have been shown to be valuable in the diagnosis and determination of the range of rhabdomyolysis [9,11-13]. In the case presented herein, the patient's BUN/Cr values, which had increased after the surgery, returned to normal on postoperative day 13. Urine output on postoperative day 2 was 1,400 ml, but from the day after surgery, was maintained at 2,000 ml or above. Therefore, the patient did not require diuretics or dialysis. Fortunately, the patient recovered from his pain and muscle weakness.
Both the surgeon and anesthesiologist are currently making efforts to prevent complications resulting from the positioning of the patient. Positioning-related complications by the flexed lateral decubitus position can be prevented by minimizing operating time, carefully padding the pressed area, and limiting the use or avoiding the use of the kidney rest.
References
1. Kim SM, Kwon KH, Yoo KH, Kim SY, Lee BC, Kang IW. Ischemic lumbar plexopathy: caused by obstruction of iliolumbar artery. J Korean Neurol Assoc. 1995; 13:156–158.
2. Kim HJ, Kim BJ, Hong SJ, Koh SB, Lee DH. A case of lumbar plexopathy diagnosed by magnetic resonance imaging. J Korean Soc Clin Neurophysiol. 2006; 8:174–178.
3. Kim TK, Yoon JR, Lee MH. Rhabdomyolysis after laparoscopic radical nephrectomy. Korean J Anesthesiol. 2010; 59(Suppl):S41–S44. PMID: 21286457.
4. Chung JH, Ahn KR, Park JH, Kim CS, Kang KS, Yoo SH, et al. Lower leg compartment syndrome following prolonged orthopedic surgery in the lithotomy position. Korean J Anesthesiol. 2010; 59(Suppl):S49–S52. PMID: 21286459.
5. Weier CA, Jones LC, Hungerford MW. Meralgia paresthetica of the contralateral leg after total hip arthroplasty. Orthopedics. 2010; 265–268. PMID: 20415307.

6. Judge A, Fecho K. Lateral antebrachial cutaneous neuropathy as a result of positioning while under general anesthesia. Anesth Analg. 2010; 110:122–124. PMID: 19910615.

7. Reisiger KE, Landman J, Kibel A, Clayman RV. Laparoscopic renal surgery and the risk of rhabdomyolysis: diagnosis and treatment. Urology. 2005; 66(5 Suppl):29–35. PMID: 16194704.

8. Riggs JE, Schochet SS Jr, Hogg JP. Focal rhabdomyolysis and brachial plexopathy: an association with heroin and chronic ethanol use. Mil Med. 1999; 164:228–229. PMID: 10091499.

9. Jeon HJ, Cho BM, Oh SM, Park SH. Lumbosacral plexopathy, complicating rhabdomyolysis in a 57-year-old man, presented with sudden weakness in both legs. J Korean Neurosurg Soc. 2007; 42:481–483. PMID: 19096594.

10. Bosch X, Poch E, Grau JM. Rhabdomyolysis and acute kidney injury. N Engl J Med. 2009; 361:62–72. PMID: 19571284.

11. Moratalla MB, Braun P, Fornas GM. Importance of MRI in the diagnosis and treatment of rhabdomyolysis. Eur J Radiol. 2008; 65:311–315. PMID: 17482406.

12. Watanabe N, Inaoka T, Shuke N, Takahashi K, Aburano T, Chisato N, et al. Acute rhabdomyolysis of the soleus muscle induced by a lightning strike: magnetic resonance and scintigraphic findings. Skeletal Radiol. 2007; 36:671–675. PMID: 17522908.

13. Ishii K, Tamaoka A, Shoji S. MRI of idiopathic lumbosacral plexopathy. Neurology. 2004; 63:E6. PMID: 15277659.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download