1. Fujii Y. Management of postoperative nausea and vomiting in patients undergoing laparoscopic cholecystectomy. Surg Endosc. 2011; 25:691–695. PMID:
20927550.
2. Fujii Y. Prevention of nausea and vomiting during termination of pregnancy. Int J Gynaecol Obstet. 2010; 111:3–7. PMID:
20598689.

3. Rose JB, Watcha MF. Postoperative nausea and vomiting in paediatric patients. Br J Anaesth. 1999; 83:104–117. PMID:
10616338.

4. Bolton CM, Myles PS, Nolan T, Sterne JA. Prophylaxis of postoperative vomiting in children undergoing tonsillectomy: a systematic review and meta-analysis. Br J Anaesth. 2006; 97:593–604. PMID:
17005507.

5. Fujii Y, Tanaka H, Ito M. A randomized clinical trial of a single dose of ramosetron for the prevention of vomiting after strabismus surgery in children: a dose-ranging study. Arch Ophthalmol. 2005; 123:25–28. PMID:
15642807.
6. Ku CM, Ong BC. Postoperative nausea and vomiting: a review of current literature. Singapore Med J. 2003; 44:366–374. PMID:
14620731.
7. Henzi I, Walder B, Tramer MR. Dexamethasone for the prevention of postoperative nausea and vomiting: a quantitative systematic review. Anesth Analg. 2000; 90:186–194. PMID:
10625002.

8. Hahm TS, Ko JS, Choi SJ, Gwak MS. Comparison of the prophylactic anti-emetic efficacy of ramosetron and ondansetron in patients at high-risk for postoperative nausea and vomiting after total knee replacement. Anaesthesia. 2010; 65:500–504. PMID:
20337618.

9. Lee HK, Lee JH, Chon SS, Ahn EK, Kim JH, Jang YH. The effect of transdermal scopolamine plus intravenous dexamethasone for the prevention of postoperative nausea and vomiting in patients with epidural PCA after major orthopedic surgery. Korean J Anesthesiol. 2010; 58:50–55. PMID:
20498812.

10. Fujii Y. Current management of vomiting after tonsillectomy in children. Curr Drug Saf. 2009; 4:62–73. PMID:
19149526.

11. Rabasseda X. Ramosetron, a 5-HT3 receptor antagonist for the control of nausea and vomiting. Drugs Today (Barc). 2002; 38:75–89. PMID:
12532186.

12. Hesketh PJ, Gandara DR. Serotonin antagonists: a new class of antiemetic agents. J Natl Cancer Inst. 1991; 83:613–620. PMID:
1850806.

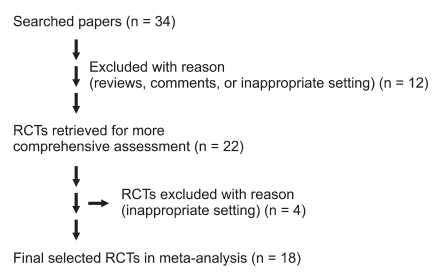
13. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009; 62:e1–e34. PMID:
19631507.

14. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Reprint--preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement. Phys Ther. 2009; 89:873–880. PMID:
19723669.

15. Watcha MF, White PF. Postoperative nausea and vomiting. Its etiology, treatment, and prevention. Anesthesiology. 1992; 77:162–184. PMID:
1609990.
16. Gan TJ, Meyer TA, Apfel CC, Chung F, Davis PJ, Habib AS, et al. Society for Ambulatory Anesthesia guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2007; 105:1615–1628. PMID:
18042859.

17. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996; 17:1–12. PMID:
8721797.

18. Bax L, Yu LM, Ikeda N, Tsuruta H, Moons KG. Development and validation of MIX: comprehensive free software for meta-analysis of causal research data. BMC Med Res Methodol. 2006; 6:50. PMID:
17038197.

19. Bax L, Yu LM, Ikeda N, Moons KG. A systematic comparison of software dedicated to meta-analysis of causal studies. BMC Med Res Methodol. 2007; 7:40. PMID:
17845719.

20. Fujii Y, Tanaka H. Results of a prospective, randomized, double-blind, placebo-controlled, dose-ranging trial to determine the effective dose of ramosetron for the prevention of vomiting after tonsillectomy in children. Clin Ther. 2003; 25:3135–3142. PMID:
14749151.
21. Fujii Y, Tanaka H, Ito M. Ramosetron compared with granisetron for the prevention of vomiting following strabismus surgery in children. Br J Ophthalmol. 2001; 85:670–672. PMID:
11371485.

22. Fujii Y, Saitoh Y, Tanaka H, Toyooka H. Ramosetron for preventing postoperative nausea and vomiting in women undergoing gynecological surgery. Anesth Analg. 2000; 90:472–475. PMID:
10648342.

23. Fujii Y, Tanaka H. Randomized, double-blind, placebo-controlled, dosed-finding study of the antiemetic effects and tolerability of ramosetron in adults undergoing middle ear surgery. Clin Ther. 2003; 25:3100–3108. PMID:
14749148.
24. Fujii Y, Tanaka H, Somekawa Y. A randomized, double-blind, placebo-controlled trial of ramosetron for preventing nausea and vomiting during termination of pregnancy. Int J Obstet Anesth. 2004; 13:15–18. PMID:
15321434.
25. Fujii Y, Uemura A, Tanaka H. Prophylaxis of nausea and vomiting after laparoscopic cholecystectomy with ramosetron: randomised controlled trial. Eur J Surg. 2002; 168:583–586. PMID:
12699092.

26. Fujii Y, Tanaka H. Double-blind, placebo-controlled, dose-ranging study of ramosetron for the prevention of nausea and vomiting after thyroidectomy. Clin Ther. 2002; 24:1148–1153. PMID:
12182258.
27. Roila F, Del Favero A. Ondansetron clinical pharmacokinetics. Clin Pharmacokinet. 1995; 29:95–109. PMID:
7586904.

28. Fujii Y, Saitoh Y, Tanaka H, Toyooka H. Ramosetron vs granisetron for the prevention of postoperative nausea and vomiting after laparoscopic cholecystectomy. Can J Anaesth. 1999; 46:991–993. PMID:
10522590.
29. Choi DK, Chin JH, Lee EH, Lim OB, Chung CH, Ro YJ, et al. Prophylactic control of post-operative nausea and vomiting using ondansetron and ramosetron after cardiac surgery. Acta Anaesthesiol Scand. 2010; 54:962–969. PMID:
20626355.

30. Ryu J, So YM, Hwang J, Do SH. Ramosetron versus ondansetron for the prevention of postoperative nausea and vomiting after laparoscopic cholecystectomy. Surg Endosc. 2010; 24:812–817. PMID:
19707823.
31. Fujii Y, Tanaka H, Kawasaki T. Benefits and risks of granisetron versus ramosetron for nausea and vomiting after breast surgery: a randomized, double-blinded, placebo-controlled trial. Am J Ther. 2004; 11:278–282. PMID:
15266219.

32. Lee SY, Lee JY, Park SY, Kim JH, Cho OG, Kim JS, et al. Prophylactic antiemetic efficacy of granisetron or ramosetron in patients undergoing thyroidectomy. Asian J Surg. 2002; 25:309–314. PMID:
12471004.

33. Fujii Y, Saitoh Y, Tanaka H, Toyooka H. Comparison of ramosetron and granisetron for preventing postoperative nausea and vomiting after gynecologic surgery. Anesth Analg. 1999; 89:476–479. PMID:
10439770.

34. Jeon Y, Kim H, Kwak K. Comparison of ramosetron, dexamethasone, and a combination of ramosetron and dexamethasone for the prevention of postoperative nausea and vomiting in Korean women undergoing thyroidectomy: A double-blind, randomized, controlled study. Current Therapeutic Research. 2010; 71:78–88.

35. Kim SI, Kim SC, Baek YH, Ok SY, Kim SH. Comparison of ramosetron with ondansetron for prevention of postoperative nausea and vomiting in patients undergoing gynaecological surgery. Br J Anaesth. 2009; 103:549–553. PMID:
19700442.

36. Lee D, Kim JY, Shin JW, Ku CH, Park YS, Kwak HJ. The effect of oral and IV ramosetron on postoperative nausea and vomiting in patients undergoing gynecological laparoscopy with total intravenous anesthesia. J Anesth. 2009; 23:46–50. PMID:
19234822.

37. Choi YS, Shim JK, Yoon do H, Jeon DH, Lee JY, Kwak YL. Effect of ramosetron on patient-controlled analgesia related nausea and vomiting after spine surgery in highly susceptible patients: comparison with ondansetron. Spine (Phila Pa 1976). 2008; 33:E602–E606. PMID:
18670328.
38. Lee HJ, Kwon JY, Shin SW, Kim CH, Baek SH, Baik SW, et al. Preoperatively administered ramosetron oral disintegrating tablets for preventing nausea and vomiting associated with patient-controlled analgesia in breast cancer patients. Eur J Anaesthesiol. 2008; 25:756–762. PMID:
18426627.

39. Fujii Y, Tanaka H. Prevention of nausea and vomiting with ramosetron after total hip replacement. Clin Drug Investig. 2003; 23:405–409.

40. Fujii Y, Tanaka H. Comparison of granisetron and ramosetron for the prevention of nausea and vomiting after thyroidectomy. Clin Ther. 2002; 24:766–772. PMID:
12075944.
41. Fujii Y, Tanaka H, Kobayashi N. Prevention of nausea and vomiting after middle ear surgery: granisetron versus ramosetron. Laryngoscope. 1999; 109:1988–1990. PMID:
10591360.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download