Abstract
Background
Spinal anesthesia causes hypotension and bradycardia due to sympathetic nerve block and it is difficult to predict the level of sensory block and the duration of blockade. Recent studies have reported that intravenous phenylephrine can reduce the rostral spread of spinal anesthesia in pregnant women. We think a phenylephrine infusion will be useful for maintaining the baseline blood pressure by reducing the rostral spread of spinal anesthesia during the elective surgery of non-obstetric patients.
Methods
Sixty patients who were undergoing urologic surgery were randomized into two groups: Group C (the control group without phenylephrine) and Group P (with the addition of phenylephrine). After a bolus infusion of 50 µg phenylephrine following the spinal injection, phenylephrine was continuously infused at the rate of 200 µg/hr. We compared the dermatomal spreads of spinal anesthesia, the hemodynamic parameters (blood pressure, heart rate) and the incidences of hypotension between the two groups.
Spinal anesthesia is a form of regional anesthesia that involves injecting local anesthetics into the subarachnoid space. Spinal anesthesia is easy to perform and it works fast using even a small amount of drug. In addition, there are less systemic complications compared to that of general anesthesia [1].
However, spinal anesthesia causes cardiovascular complications such as hypotension and bradycardia due to sympathetic nerve block and it has the difficulty to predict the level of sensory block and the duration of blockade.
Absorption of the administered local anesthetics in the subarachnoid space changes the neurologic function. Elimination of the drug from the subarachnoid space and its distribution in the cerebrospinal fluid (CSF) determine the onset time and the level of blockade.
Recent studies have shown that intravenous phenylephrine injection lowers the level of spinal anesthesia during cesarean delivery [2,3]. However, there has been no such study on non-obstetric patients. It is thought that a phenylephrine infusion will be useful to maintain the baseline blood pressure and reduce the rostral spread of spinal anesthesia in the elective surgery of non-obstetric patients. The aim of this study is to evaluate the block level after intravenous phenylephrine administration during spinal anesthesia in urologic surgery.
The present study was approved by the Institutional Bioethics Board for Clinical Research and the study population consisted of sixty patients with an American Society of Anesthesiologists physical status of I-II, they were 18-70 years of age, they were scheduled to undergo elective urologic surgery and they consented to receive spinal anesthesia. We obtained written informed consent from all the patients. The patients who had contraindications to spinal anesthesia or a history of hypertension, cardiovascular disease or spinal disease were excluded. No premedication was given before surgery. The patients were intravenously injected with 10 ml/kg Ringer's lactate solution until the induction of anesthesia, for the prevention of hypotension.
An electrocardiogram (EKG), a non-invasive auto-blood pressure (BP) measurement instrument and pulse oximetry were set up for monitoring the vital signs, while oxygen was provided at 5 L/min via a face mask until the end of the operation.
To perform spinal anesthesia, the patients were placed into a right lateral decubitus position. After the disinfection of the needle insertion site, a dural puncture was made with a 25-G Whitacre spinal needle at the L3-L4 lumbar inter-vertebral space. The location of the subarachnoid space was confirmed by the leakage of cerebrospinal fluid (CSF).
The sixty patients were randomly divided into two groups of 30 persons each: Group C (the control group without phenylephrine) and Group P (with the addition of phenylephrine). Each 10 mg hyperbaric solution of 0.5% bupivacaine was slowly injected to the patients of each group for approximately 15-20 seconds. The patients were then immediately placed in the supine position.
Group P received a 50 µg bolus of phenylephrine at the end of the spinal injection, and then phenylephrine was infused at the rate of 200 µg/hr for 20 min.
The block height, BP and heart rate were measured at 5, 10 and 20 min after spinal anesthesia. An alcohol swab was used to assess cold sensation for checking the blockade level.
A systolic BP under 90 mmHg or a BP decrease more than 20% of the baseline value was defined as hypotension, and ephedrine 8 mg was promptly given intravenously to counteract this. In case of a heart rate lower than 50 beats/min, atropine 0.5 mg was intravenously injected. We recorded the side-effects that the patients complained of such as nausea, vomiting, headache, pruritus and chills.
The SPSS program (version 12.0, SPSS Inc., USA) was used for statistical analysis. For the HR, SAP, DAP and the demographic data, student's t-test was applied to compare the difference in the groups. The Mann-Whitney test was applied to compare the level of sensory blockade. The data of HR, SAP, DAP and the demographic data are expressed as mean ± standard deviation. The data of the level of sensory blockade are expressed as median (interquartile range). P values < 0.05 were deemed statistically significant.
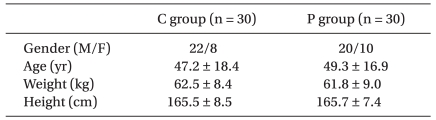
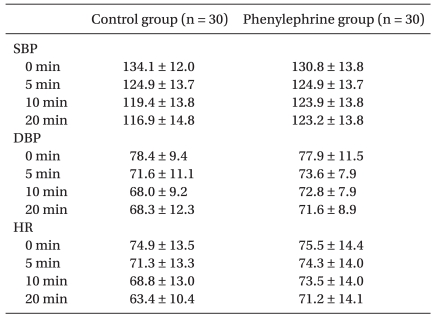
There were no significant differences of age, height, weight and gender between the 2 groups (Table 1). In addition, the systolic BP and diastolic BP were similar in both groups before and after the induction of spinal anesthesia (Table 2). There was no significant difference in heart rate between the 2 groups, as well.
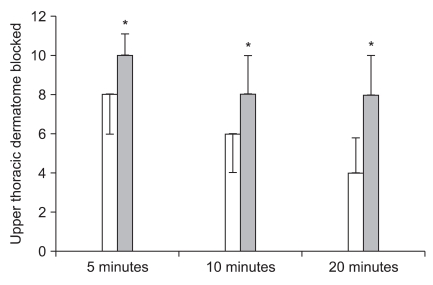
Group P showed a significantly lower level of the highest sensory blockade as compared to that of Group C as T4 (interquartile range: T4-T6) in Group C and T8 (interquartile range: T8-T10) in Group P (P < 0.0001). The level of sensory blockade 5 minutes after the initiation of spinal anesthesia was lower in Group P than that in Group C at T8 (T6-T8) and T10 (T10-T11) at 5 minutes, T6 (T4-T6) and T8 (T8-T10) at 10 minutes and T4 (T4-T6) and T8 (T8-T10) at 20 minutes. The differences were statistically significant. The data are expressed as median (interquartile range) (Fig. 1). There were 2 cases that needed ephedrine injection for hypotension only in C group. The systolic BP was less than 90 mmHg at that time and the level of block was T4, but it was restored to the normal range with an injection of 8 mg of ephedrine. Only one patient in group C complained of nausea. There was no patient who showed arrhythmia or who suffered from vomiting and who needed an injection of atropine to prevent bradycardia.
Spinal anesthesia is advantageous compared to epidural anesthesia as it has a rapid induction time, superior muscle relaxation, a lower rate of failure associated with the procedure and little systemic toxicity because of the small amount of local anesthetic used. Spinal anesthesia has lower systemic adverse effects, a lower incidence of postoperative thromboembolism and cardiovascular complications in high risk patients and a smaller amount of bleeding and transfusion intraoperatively than general anesthesia [1].
However, it has several disadvantages such as cardiovascular complications like hypotension and bradycardia that are induced by sympathetic blockade, and it is difficult to accurately estimate the level of sensory blockade and the duration and degrees of anesthesia. Although exact anesthetics and the appropriate selection of the specific gravity of the local anesthetics have been used, spinal anesthesia has shown various depths and extents of anesthesia. For that reason, we should take into consideration the factors that affect the level of sensory blockade to maintain an adequate level of anesthesia.
The factors are the individual characteristics of patients, the technical skills to inject anesthetics, the properties of the CSF, the features of the anesthetics and so on. Greene reported 25 factors that affect the distribution of local anesthetics, and the patients' age and weight, the region of injection, the direction of the hole of the needle, the volume of CSF, the density and specific gravity of the anesthetics, the patient's position and the volume of anesthetics are important, although they have shown diverse results for their clinical significance [4]. In this study, there was no significant difference of age, weight, height and gender between the 2 groups, and the size of the needles and the direction of the needle hole were equal for both groups.
Phenylephrine is a pure vasoconstrictor that shows a similar vasoconstrictive effect on arteries and veins as a selective α-adrenergic agonist. Its duration of action is relatively short (2-5 minutes) when it is injected intravenously and it is metabolized in the liver by monoamine oxidase. Its cardiovascular effects are constriction of the systemic, pulmonary and coronary vessels, and a decrease of the cardiac output and blood flow of kidney, intestine and subcutaneous tissues. Moreover, it has β-adrenergic effects like tachycardia and supraventricular arrhythmia at high doses [5].
There have been some studies about the subarachnoid injection of epinephrine or phenylephrine together with the main local anesthetics to prolong the duration of spinal anesthesia. These drugs decrease neural blood flow and this delays the absorption of the anesthetics, which prolongs the duration of their effects. The exact mechanism hasn't been clearly explained, but it has been suggested that these drugs decrease spinal blood flow and the excretion of local anesthetic [6,7].
Two recent studies reported that intravenous injection of phenylephrine lowered the level of sensory blockade for patients who received spinal anesthesia for cesarean section [2,3]. Yet there have been no studies about the effect of phenylephrine injection in non-obstetric surgeries. We demonstrated that the highest level of sensory blockade constantly showed a meaningful difference between the 2 groups of patients who were undergoing urologic surgery, as T4 in the control group was higher than T8 in the phenylephrine group.
The physical characteristics of the CSF such as the volume and density are important factors for the spread of local anesthetics during spinal anesthesia. Carpenter et al. reported a correlation between the lumbosacral CSF volume and the peak sensory block level using magnetic resonance imaging (MRI) [8]. Schiffer et al. [9] reported that the CSF density is an important factor that influences the peak sensory block level of spinal anesthesia.
Two previous studies have shown that intravenous injection of phenylephrine compared with intravenous injection of ephedrine can decrease the rostral spread of intrathecal local anesthetics. Cooper et al. [2] explained that this is due to the character of phenylephrine to elevate the venous tone. Phenylephrine increases the right atrial pressure during spinal anesthesia and this would increase the intracranial pressure and cause a considerable amount of CSF to shift from the cranial cavity to the vertebral canal. Another explanation is that phenylephrine may constrict engorged lumbar epidural veins and thereby lower the pressure of the epidural space and reduce the spread of intrathecal local anesthetics [3].
In our study, it is possible that the elevated intracranial pressure by phenylephrine leads to preventing cephalad migration of CSF and this limits the height of the sensory blockade by increasing the lumbosacral CSF volume. However, non-obstetric patients don't have vasodilatation of epidural veins as compared with that of obstetric patients, so there might be some difference of the effect of phenylephrine in non-obstetric patients.
In addition, the motion of the CSF might be an important factor that influences the block level of spinal anesthesia. The spread of intrathecal drugs is initially influenced by bulk displacement, the injection currents, gravity and the baricity and then by diffusion through the cerebrospinal fluid and into the central nervous system. Diffusion of an intrathecal anesthetic drug, which is affected by CSF movement, is thought to have a major effect on its intrathecal spread [10]. The advances of dynamic MRI have enabled visualization and quantitation of the CSF flow dynamics and this has contributed to our understanding of the origin of CSF pulsation and its relation to the pulsatile blood flow. Recent MRI observations have shown that CSF is not static, but rather, it vigorously oscillates with arterial pulsations [11].
Using cardiac gated, phase-contrast, cine, high resolution MRI, Higuchi et al. [12] reported that the velocity of the CSF influenced the extent and duration of spinal anesthesia. In an observational study about CSF motion after prehydration, which delayed the time to reach the peak sensory block level during clinical spinal anesthesia, and decreased CSF pulsation in healthy volunteers [13]. The hemodynamic changes influence CSF pulsation. The hemodynamic effects of prehydration can influence CSF motion and flow, and it may influence the intrathecal spread of local anesthetics.
Similarly, the vasoconstriction of spinal vessels may affects spinal CSF flow and the CSF pulsations at the lumbar level, which may contribute to a decrease in the cephalic spread of sensory block with using spinal anesthetic drugs. But there have been no studies on the influence of spinal anesthesia on the CSF flow. Further studies on the CSF flow alteration after spinal anesthesia and phenylephrine infusion will be helpful.
The systolic BP, diastolic BP and heart rate were similar in both groups before and after the induction of spinal anesthesia. But there were 2 patients in C group who needed ephedrine injection for hypotension. It is thought that prehydration might prevent severe hypotension in these patients. Many clinicians have recommended the administration of fluids before spinal anesthesia to reduce the incidence and severity of hypotension, but its effect are controversial [14,15]. There have been several studies that reported there was no role for preemptive hydration before spinal anesthesia, and especially for non-obstetric elective surgeries in elderly patients and in hypotensive patients, and these patients should be treated with boluses of vasopressors [16]. Therefore, it could be useful to inject phenylephrine to certain patients, and especially patients with cardiovascular disease and aged patients who should not be hydrated with excessive fluid. Phenylephrine injection could reduce these kinds of complications and prevent unexpected high levels of blockade and hypotension.
This study went on only for the first 20 minutes of spinal anesthesia and the block level of spinal anesthesia might not have been the peak block level. We cannot exclude the possibility that the differences of block levels resulted from the delay of time to reach the peak sensory block level.
In conclusion, phenylephrine injection could be a factor that affects the level of sensory blockade, yet further studies on this are certainly called for.
References
1. Kleinman W, Mikhail M. Morgan GE, Mikhail M, Murray MJ, editors. Spinal, epidural & caudal blocks. Clinical anesthesiology. 2005. 4th ed. New York: McGraw-Hill press;p. 290.
2. Cooper DW, Jeyaraj L, Hynd R, Thompson R, Meek T, Ryall DM, et al. Evidence that intravenous vasopressors can affect rostral spread of spinal anesthesia in pregnancy. Anesthesiology. 2004; 101:28–33. PMID: 15220768.

3. Ngan Kee WD, Lee A, Khaw KS, Ng FF, Karmakar MK, Gin T. A randomized double-blinded comparison of phenylephrine and ephedrine infusion combinations to maintain blood pressure during spinal anesthesia for cesarean delivery: the effects on fetal acid-base status and hemodynamic control. Anesth Analg. 2008; 107:1295–1302. PMID: 18806043.

4. Greene NM. Distribution of local anethetc solutions within the subarachnoid space. Anesth Analg. 1985; 64:715–730. PMID: 3893222.
5. Collins VJ. Physiologic and pharmacologic bases of anesthesia. 1996. Pennsylvania: Williams & Wilkins press;p. 737.
6. Caldwell C, Nielsen C, Baltz T, Taylor P, Helton B, Butler P. Comparison of high-dose epinephrine and phenylephrine in spinal anesthesia with tetracaine. Anesthesiology. 1985; 62:804–807. PMID: 4003805.

7. Sakura S, Sumi M, Sakaguchi Y, Saito Y, Kosaka Y, Drasner K. The addition of phenylephrine contributes to the development of transient neurologic symptoms after spinal anesthesia with 0.5% tetracaine. Anesthesiology. 1997; 87:771–778. PMID: 9357877.

8. Carpenter RL, Hogan QH, Liu SS, Crane B, Moore J. Lumbosacral cerebrospinal fluid volume is the primary determinant of sensory block extent and duration during spinal anesthesia. Anesthesiology. 1998; 89:24–29. PMID: 9667290.

9. Schiffer E, Van Gessel E, Fournier R, Weber A, Gamulin Z. Cerebrospinal fuid density influences extent of plain bupivacaine spinal anesthesia. Anesthesiology. 2002; 96:1325–1330. PMID: 12170043.
10. Hocking G, Wildsmith JA. Intrathecal drug spread. Br J Anaesth. 2004; 93:568–578. PMID: 15220175.

11. Henry-Feugeas MC, Idy-Peretti I, Baledent O, Poncelet-Didon A, Zannoli G, Bittoun J, et al. Origin of subarachnoid cerebrospinal fluid pulsations: a phase-contrast MR analysis. Magn Reson Imaging. 2000; 18:387–395. PMID: 10788715.
12. Higuchi H, Hirata J, Adachi Y, Kazama T. Influence of lumbosacral cerebrospinal fluid density, velocity, and volume on extent and duration of plain bupivacaine spinal anesthesia. Anesthesiology. 2004; 100:106–114. PMID: 14695731.

13. Shin BS, Ko JS, Gwak MS, Yang M, Kim CS, Hahm TS, et al. The effects of prehydration on the properties of cerebrospinal fluid and the spread of isobaric spinal anesthetic drug. Anesth Analg. 2008; 106:1002–1007. PMID: 18292453.

14. Morgan PJ, Halpern SH, Tarshis J. The effects of an increase of central blood volume before spinal anesthesia for cesarean delivery: a qualitative systematic review. Anesth Analg. 2001; 92:997–1005. PMID: 11273939.

15. Rout CC, Akoojee SS, Rocke DA, Gouws E. Rapid administration of crystalloid preload does not decrease the incidence of hypotension after spinal anaesthesia for elective caesarean section. Br J Anaesth. 1992; 68:394–397. PMID: 1642918.

16. Buggy D, Higgins P, Moran C, O'Brien D, O'Donovan F, McCarroll M. Prevention of spinal anesthesia-induced hypotension in the elderly: comparison between preanesthetic administration of crystalloids, colloids, and no prehydration. Anesth Analg. 1997; 84:106–110. PMID: 8989009.
Fig. 1
Upper dermatome blocked to cold sensation at 5, 10 and 20 min postspinal for the control group (white bars) and the phenylephrine group (gray bars). Data are expressed as median (interquartile range). There was a difference between the groups at 5, 10 min and at 20 min postspinal (Mann-Whitney U test). *P < 0.001 vs control
group.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download