Introduction
Laparoscopic surgery has greatly developed recently and is becoming a standard surgical procedure because of its important advantages, namely less tissue trauma, decreased postoperative pain, as well as a shorter hospital stay with minimized postoperative morbidity and mortality. In gynecologic surgery, laparoscopic operations usually require a steep Trendelenburg position and artificial pneumoperitoneum with carbon dioxide (CO
2) insufflation. In the steep Trendelenburg position, intracranial pressure (ICP) increases due to increased venous pressure, which hinders cerebral venous drainage with a consequential increase in the cerebral blood volume (CBV) and cerebrospinal fluid (CSF) volume [
1,
2]. The pneumoperitoneum with CO
2 also elevates ICP because increased abdominal pressure obstructs venous return from the lumbar venous plexus [
3], and increased cerebral blood flow (CBF) due to an increase in arterial partial pressure of carbon dioxide (PaCO
2) and catecholamine release independent of PaCO
2 [
4].
Near-infrared spectroscopy (NIRS) cerebral oximetry allows continuous and noninvasive monitoring of regional cerebral oxygen saturation (rSO
2). Cerebral oxygen saturation reflects the balance between cerebral oxygen supply and demand and it is affected by changes in blood oxygenation, CBF, hemoglobin (Hb) content, and cerebral metabolic rate of oxygen (CMRO
2) [
5]. A number of clinical studies and case reports have demonstrated the ability of cerebral oximetry monitoring to detect changes in CBF and cerebral ischemia [
6-
8]. In a recent study in patients with subarachnoid hemorrhage, episodes of angiographic cerebral vasospasm were strongly associated with a reduction in the ipsilateral NIRS signal [
6]. NIRS can be a valuable tool for detection of cerebral ischemia during carotid endarterectomy (CEA) [
7]. Furthermore, a significant correlation between rSO
2 values immediately after declamping and changes in CBF was found, and can be used for detecting patients at risk of developing post-CEA hyperperfusion syndrome [
8]. The use of NIRS in laparoscopic surgery in the Trendelenburg position has been studied, but results have been equivocal. Lee et al. [
9] reported that rSO
2 declined significantly in the Trendelenburg position during gynecological laparoscopic surgery under isoflurane anesthesia. They reported that it was caused by a reduction in cerebral perfusion pressure (CPP) as a result of an increase in ICP, CBF, and CBV. In contrast, some studies [
10,
11] demonstrated that with inhaled anesthetics rSO
2 was increased during abdominal surgery in the Trendelenburg position and this was, ironically, explained by increased CBF and CBV.
It is well known that anesthetic agents have variable effects on cerebral hemodynamics and ICP. Consequently, the choice of maintenance anesthetic could be important in laparoscopic surgery in order to minimize adverse cerebrovascular responses. Inhaled anesthetics have a dual effect on the cerebral vasculature. In low concentrations halothane, isoflurane, and sevoflurane constrict cerebral vessels secondary to suppression of CMRO
2. With increasing concentration, the direct vasodilatory effect of inhaled anesthetics turns dominant, leading to high CBF and CBV and to elevated ICP. However, propofol reduces CMRO
2, CBF, CBV, and ICP in a dose-dependent manner [
12]. Several studies have demonstrated that the reduction in CBF is larger than the reduction in CMRO
2, which suggests that propofol may have direct cerebral vasoconstricting activity [
13], which might lead to a decrease in cerebral perfusion and a decrease in the CBF/CMRO
2 ratio. In situations where there is an increased ICP, such as a brain tumor, inhaled anesthetics had a significantly higher CBF/CMRO
2 ratio or jugular venous oxygen saturation (SjO
2) compared with propofol [
14-
16]. Since laparoscopic surgery in the Trendelenburg position also elevates CBF, CBV and ICP, we hypothesized that, during sevoflurane anesthesia, rSO
2 is more favorable compared with propofol anesthesia during laparoscopic surgery in the Trendelenburg position.
Materials and Methods
Patient selection
The study was performed on patients who were undergoing gynecological laparoscopic surgery under general anesthesia. Thirty two adult women between 18 and 60 years old with an American Society of Anesthesiologists physical status of I or II were enrolled. Exclusion criteria were as follows: a history of any cerebrovascular disease, poorly controlled hypertension, or obesity (body mass index >30). Ethical approval for the study was given by the Institutional Review Board of our Hospital and all patients were given written informed consent before enrollment.
Study protocol
In this study, two groups were identified according to the method of general anesthesia, one with sevoflurane and remifentanil, and the other with total intravenous anesthesia using target controlled infusion (TCI) of propofol and remifentanil. Randomization was done by two independent anesthesiologists using 32 opaque sealed envelopes, 16 for each group, indicating patient group assignment and describing the anesthetic protocol. The patients and anesthesiologists involved in data collection and analysis of results, were not aware of group assignments.
All patients received 3 mg of midazolam and 0.2 mg of glycopyrrolate intramuscularly 30 min before surgery. Standard monitoring and bispectral index (BIS; Bispectral Index™, Aspect Modical System Inc., Norwood, MA, USA) monitoring were done. Before induction of anesthesia, a 20 G radial artery catheter was inserted for continuous arterial pressure monitoring and arterial blood gas analysis. For rSO2 measurement, sensors for cerebral oximetry were placed bilaterally above the eyebrow on the right and left sides of the forehead before induction of anesthesia. The rSO2 value was continuously monitored using NIRS (INVOS 5100; Somanetics Corp., Troy, Michigan, USA). The values for each side were averaged.
In the sevoflurane group, general anesthesia was induced with 1.5 mg/kg of propofol, 8 vol% of sevoflurane and continuous remifentanil infusion using TCI (Orchestra® with Base Primea, Fresenius Kabi, France) to reach 2 ng/ml for the target effect site concentration. In the propofol group, anesthesia was induced with continuous propofol and remifentanil infusion by TCI to reach 4 µg/ml and 2 ng/ml of target effect site concentration, respectively. Once the BIS was stable between 40 and 50, 0.8 mg/kg of rocuronium was used to facilitate tracheal intubation. Anesthesia was maintained by a mixture of oxygen and air with a fixed FiO2 of 0.5, and mechanical ventilation was adjusted to maintain an end tidal CO2 tension (ETCO2) of 30 to 35 mmHg throughout the surgery.
The BIS was used to guide administration of sevoflurane and propofol. The BIS target range during maintenance was 40 to 50. Clinical signs of inadequate anesthesia were treated with increasing or decreasing the inspired concentration of sevoflurane or the target effect site concentration of propofol. Mean arterial pressure (MAP) and heart rate (HR) were used to guide the administration of remifentanil. Both variables were maintained within 20% of baseline, if hypotension (MAP < 60 mmHg) or bradycardia (HR < 45 beats/min) persisted more than 5 min, the patient was treated with ephedrine 10 mg or atropine 0.5 mg. A case was excluded if the patient was given ephedrine or atropine more than three times.
After induction of general anesthesia, patients were positioned in the low lithotomy position and the abdominal cavity was insufflated with CO2 gas pressure set to 15 mmHg. Patients were then placed in the Trendelenburg position of 20° during surgery. MAP, HR, oxygen saturation (SpO2), rSO2, ETCO2, endtidal sevoflurane tension (ETsevo), effect site concentration of propofol, esophageal temperature, Hb, arterial oxygen partial pressure (PaO2), and arterial CO2 partial pressure (PaCO2) were recorded at 10 min after induction in the neutral position (Tpre), 10 min after the insufflation of the abdomen with CO2 in the Trendelenburg position (Tpt) and 10 min after desufflation of the abdomen in the neutral position (Tpost).
Any complications, including nausea, vomiting, headache, blurred vision, or neurologic deficits were recorded in the recovery room 60 min after the operation. Duration of anesthesia, operation, and Pneumoperitoneum-Trendelenburg time (P-T time), total dose of remifentanil given in the operating room, blood loss, urine output, and IV fluid volume were also recorded.
Cerebral oxygen desaturation was defined as an rSO2 value < 75% of the baseline value, or an rSO2 value < 50%. In the event of such a decrease in rSO2, the following algorithm was followed: normotension was ensured; the patient's neck was checked for changes in position or the presence of external factors that may have caused arterial or venous obstruction. If the decrease in rSO2 was refractory to all the above measures, 100% oxygen was administered and no further intervention was performed.
Statistical analysis
Data are expressed as mean ± standard deviation (SD). Demographic variables, duration of surgery and anesthesia, P-T time, the total doses of remifentanil given in the operating room, blood loss, urine output, and IV fluid volume between the groups were compared using unpaired student t-tests. Hemodynamic variables, rSO
2, BIS, blood gas were analyzed using two-way ANOVA with repeated measurement (intergroup comparisons) and one-way ANOVA with repeated measurement (intragroup comparisons). For analysis of rSO
2, univariate two-way analysis of covariance (ANCOVA) was done with MAP and ETCO
2 as the covariates. Post hoc analysis was performed with the Bonferroni/Dunn correction. The Chi square test was used to compare the incidence of intraoperative cerebral oxygen desaturation and complications. The level of statistical significance was set at P < 0.05. To calculate sample size, we used the mean and standard deviation (SD) of the first 5 patients in each group at Tpt time point. The mean rSO
2 (SD) were 78.0% (6.6) and 70.0% (7.2) in the sevoflurane and propofol groups, respectively. With a type I error of 0.05 and a type II error of 0.2, the required sample size was 13 patients in each group. We assumed a dropout rate of 20%, so 32 patients were recruited. Data were analyzed using StatView version 5.0 (SAS, Chicago, IL). Sample size was determined by "G power" (the software is available and free from the web site:
http://www.psycho.uni-duesseldorf.de/aap/projects/gpower/index.html).
Results
A total of 32 patients were enrolled. Five patients were excluded: in the sevoflurane group, the surgical method was changed to laparotomy in two patients and failure to control PaCO2 in one patient; in the propofol group, cerebral oxygen desaturation occurred in two patients.
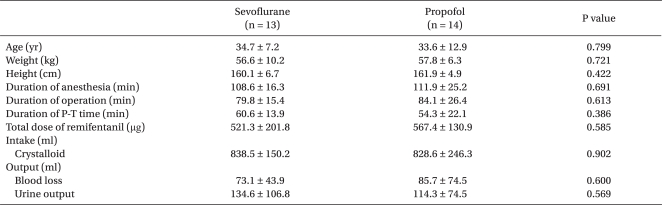
Demographic variables are shown in
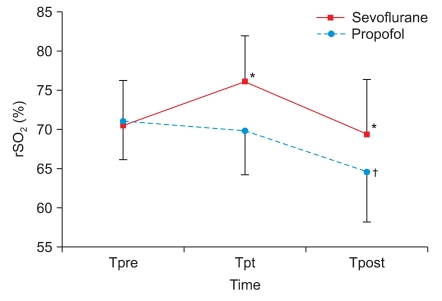
Table 1. There was no significant difference in demographic variables between the two groups. The change in rSO
2 is shown in
Fig. 1. There was a significant difference between the two groups in rSO
2 (P = 0.027 with ANOVA, P = 0.021 with ANCOVA). At Tpt, the rSO
2 value was 76.3 ± 5.9% for the sevoflurane group and 69.4 ± 5.8% for the propofol group. At Tpost, the rSO
2 value was 69.5 ± 7.1% in the sevoflurane group and 63.8 ± 6.6% in the propofol group. The rSO
2 values at Tpt and Tpost were significantly higher in the sevoflurane group compared with the propofol group (P = 0.015 at Tpt, P = 0.048 at Tpost). In the sevoflurane group, the change in rSO
2 was statistically significant by ANOVA (P = 0.028) but was not significant with ANCOVA (P = 0.957). Similarly, in the propofol group, the change in rSO
2 was statistically significant with ANOVA (P = 0.020) but was not significant with ANCOVA (P = 0.350). In the sevoflurane group, rSO
2 at Tpt was higher than at Tpre but the difference was not significant (P = 0.028, Bonferroni/Dunn correction). In the propofol group, rSO
2 at Tpost was significantly lower than at Tpre (P = 0.013).
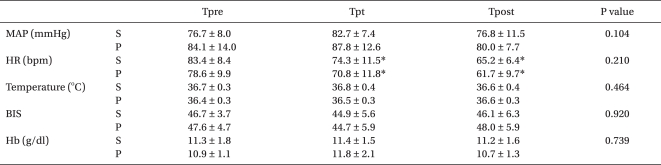
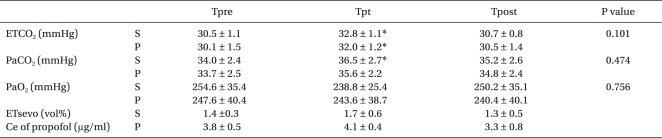
There was no significant difference in hemodynamic variables, BIS values, temperature, Hb, and blood gas analysis between the two groups (
Table 2 and
3). MAP, temperature, BIS values, Hb, and PaO
2 remained constant throughout the study. However, ETCO
2 was significantly higher at Tpt than at Tpre in both groups (P = 0.042 for the sevoflurane group, P = 0.032 for the propofol group). PaCO
2 showed a similar pattern to ETCO
2 - it was significantly higher at Tpt than at Tpre (P = 0.011) in the sevoflurane group, whereas it was not significant in the propofol group.
The incidence of complications was significantly higher in the sevoflurane group compared with the propofol group (46.2% vs 7.1%, P = 0.021); 6 patients complained of nausea in the sevoflurane group and 1 patient complained of headache in the propofol group. Two cases of cerebral oxygen desaturation occurred between Tpt and Tpost in the propofol group (14.3%, P = 0.157), but they did not have any complications postoperatively.
Discussion
This study demonstrated that sevoflurane anesthesia provides a significantly higher rSO2 value after CO2 pneumoperitoneum and surgery in the Trendelenburg position compared with propofol anesthesia. In the sevoflurane group, rSO2 increased after the CO2 pneumoperitoneum and the Trendelenburg position and then gradually decreased to a value close to the baseline. In the propofol group, rSO2 value did not change significantly after CO2 pneumoperitoneum and the Trendelenburg position. It decreased gradually over time, even after desufflation of the abdomen in the neutral position, and finally became significantly lower than the baseline value.
To the best of our knowledge, this is the first attempt to compare the effect of sevoflurane and propofol on cerebral oxygenation with CO
2 pneumoperitoneum and the Trendelenburg position. However, it is well known that patients with an increased ICP, such as patients with a brain tumor, respond to inhaled anesthetics such as sevoflurane with a significantly higher CBF/CMRO
2 ratio and SjO
2 compared than they do after propofol [
14-
16]. Mielck et al. [
14] reported that 1 MAC sevoflurane reduced CBF and CMRO
2 by approximately 38% and 47% respectively, compared with the awake state in cardiac patients. Vandesteene et al. [
15] found that propofol at infusion rates of 6 and 12 mg/kg/h decreased CBF by 28% and 39% respectively, and CMRO
2 by 5% and 22%, respectively. Taken together, the CBF/CMRO
2 ratio can be maintained during sevoflurane based anesthesia but reduced during propofol anesthesia. SjO
2 reflects the global CBF/CMRO
2 ratio and some studies showed results compatible with the studies we mentioned above. Muñoz et al. [
16] reported that mean SjO
2 values at a PaCO
2 of 29 mmHg were 56% and 50% under sevoflurane and propofol anesthesia, respectively. The incidence of "SjO
2 less than 50%" was higher under propofol anesthesia compared with sevoflurane anesthesia (60% vs. 20%). Their result is compatible with this study which found that there were 2 cases of cerebral oxygen desaturation in the propofol group. An imaging study also demonstrated that both anesthetic agents caused a global reduction of regional CBF, but the effect was greater for propofol than for sevoflurane [
17].
Park et al. [
10] and Kalmar et al. [
18] reported that rSO
2 increased with steep Trendelenburg positioning and pneumoperitoneum under general anesthesia with inhaled anesthetics because of increased PaCO
2, MAP and catecholamine release. Their results were similar to results in this study. In each group, the change in rSO
2 was statistically significant using one way ANOVA. But the significance disappeared when the covariates (MAP and ETCO
2) were introduced. However, between the two groups, the change in rSO
2 was significantly different even with ANCOVA. This means that propofol and sevoflurane have different effects on rSO
2 in pneumoperitoneum and the Trendelenburg position independent of MAP and ETCO
2.
Among factors that affect cerebral oxygenation, we could maintain blood oxygenation and Hb content constant by providing a fixed FiO
2 and monitoring PaO
2 and Hb with arterial blood gas analysis. We could also assume that CMRO
2 was constant during the study period because BIS (between 40 and 50) was used to guide administration of sevoflurane and propofol. Alkire [
19] reported that BIS correlated linearly with the magnitude of the cerebral metabolic reduction caused by propofol and isoflurane anesthesia and that it was mathematically quantifiable, and they found that sevoflurane's effect on CMRO
2 is very similar to that of isoflurane. Kaisti et al. [
17] also reported that sevoflurane reduced regional CBF less than propofol but regional CMRO
2 to an extent similar to propofol at the same BIS level. In this study, rSO
2 was mainly affected by CBF. The differences in CBF between sevoflurane and propofol should be taken into consideration, as suggested by the equation: CBF = CPP/Cerebral vascular resistance (CVR) = (MAP - ICP)/CVR.
In normal subjects, the initial increases in CBV do not result in a significant elevation in ICP because there is latitude for compensatory adjustments by other intracranial compartments such as a translocation of venous blood and cerebrospinal fluid (CSF) to extracerebral vessels and the spinal CSF space, respectively. CBF velocity increases during CO
2 pneumoperitoneum in response to increased PaCO
2. When normocapnia is maintained, pneumoperitoneum combined with the Trendelenburg position does not induce harmful changes in intracranial dynamics [
20]. However, when intracranial compliance is reduced, an increase in CBV can cause herniation or reduce CPP sufficiently to cause ischemia. Also, passive engorgement of the cerebral venous system as a result of the Trendelenburg position, compression of the jugular vein, or high intrathoracic pressure can have dramatic effects on ICP. In this study, rSO
2 increased initially with CO
2 pneumoperitoneum and Trendelenburg position, and gradually decreased with sevoflurane anesthesia. This can be assumed to occur for the situations we mentioned above. One is that rSO
2 initially increased and returned to baseline by compensatory adjustment such as translocation of venous blood. Another is probably due to a decreased CPP as ICP and CBV increase. Kalmar et al. [
18] demonstrated that CPP increased significantly after institution of the steep Trendelenburg position, and remained well above what is considered to be the lower limit for autoregulation of CBF during the whole procedure. So we can assume that the reason rSO
2 initially increased and returned to the baseline value in the sevoflurane group is mainly due to a compensatory adjustment rather than decreased CPP.
Interestingly, in the propofol group, there was no elevation in rSO
2 after assuming the Trendelenburg position and creating pneumoperitoneum in this study. A previous study [
21] demonstrated that a significantly higher CPP was found in the propofol group compared with the isoflurane and sevoflurane groups in patients with cerebral tumors. Then CBF must be higher in the propofol group and rSO
2 has to be as well. It is true only when they have the same pressure-flow curve of cerebral autoregulation and cerebrovascular resistance. Dose-dependent cerebral vasodilation of volatile anesthetics results in attenuation of autoregulatory capacity which means that the autoregulatory plateau becomes a positive slope. Also, both the upper and lower thresholds are shifted to the left [
22]. In acute intracranial hypertension, upper and lower limits of the autoregulatory plateau were shifted to the left and the autoregulatory plateau narrowed, because the shift of the upper limit was more pronounced than that of the lower limit [
23]. Although a recent study [
24] reported no change in CBF velocity in response to phenylephrine-induced increases in MAP during anesthesia with 1.5 MAC sevoflurane, a low dose of sevoflurane may cause a small positive slope, whereas propofol may not [
25]. We assume that a slight increase of CPP resulted in a greater increase of CBF induced by the positive pressure-flow curve in the sevoflurane group. In contrast, though CPP was higher in the propofol group, the plateau pressure-flow curve caused CBF to remain unchanged. An explanation for the rSO
2 value at Tpost in the propofol group, which was significantly lower than the baseline value, remains elusive. A previous study [
13] suggested that propofol might have direct cerebral vasoconstricting activity, which might lead to a decrease in CBF. Intact CBF autoregulation and cerebral vasoconstricting activity of propofol might cause rSO
2 to decrease during the pneumoperitoneum in the Trendelenburg position and even after desufflation of the abdomen in the neutral position.
This study has several limitations. First, although NIRS is a continuous, noninvasive monitor used to evaluate the adequacy of regional cerebral oxygenation, this technique measures only regional oxygenation of the frontal cortex [
5]. Therefore, changes in rSO
2 do not imply cerebral global oxygenation. And NIRS measures oxyhemoglobin in the entire tissue bed, which means that it is unable to distinguish between arterial and venous saturation [
26]. Second, we did not measure the velocity of the middle cerebral artery for the CBF autoregulation test which might be a key mechanism in this study. Further studies are needed to determine whether sevoflurane and propofol alter CBF autoregulation during laparoscopic surgery. Third, we measured postoperative complications, such as nausea, vomiting, headache, blurred vision, and neurologic deficits that might indicate increased ICP or cerebral hypoperfusion. Although the incidence of complications was significantly higher in the sevoflurane group, which showed conflicting results with rSO
2 values, all complications in the sevoflurane group were nausea. However, it is well known that PONV occur more frequently in sevoflurane anesthesia than in propofol anesthesia [
27]. It is difficult to determine whether the nausea was a simple PONV or a complication of increased ICP.
In summary, the propofol group showed significantly lower rSO2 values than the sevoflurane group in gynecological laparoscopic surgery not only during pneumoperitoneum in the Trendelenburg position but also after desufflation of the abdomen in the neutral position. Moreover, since cases of cerebral oxygen desaturtaion occurred only in the propofol group (n = 2), the possibility of cerebral oxygen desaturation should not be overlooked during propofol anesthesia even after desufflation of the abdomen in the neutral position.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download