Abstract
Background
Since 2009, database construction of anesthesia-related adverse events has been initiated through the legislation committee of the Korean Society of Anesthesiologists (KSA), based on expert consultation referrals provided by police departments, civil courts, and criminal courts.
Methods
This study was a retrospective descriptive analysis of expert consultation referrals on surgical anesthesia-related cases between December 2008 and July 2010.
Results
During the given period, 46 surgical anesthesia-related cases were referred to the KSA legislation committee for expert consultation. Because six cases were excluded due to insufficient data, 40 cases were included in the final analysis. Of 40 cases, 29 (72.5%) resulted in death. Respiratory events were most common in both surviving/disabled and dead patients (36.4 vs. 51.7%, respectively; P > 0.05). Overall, respiratory depression due to the drugs used for monitored anesthesia care (MAC) was the most common specific mechanism (25%), in which all but one case (profound brain damage) resulted in death. In all of these cases, surgeons or physicians provided MAC without the help of anesthesiologists.
Conclusions
Overall, the most common damaging mechanism was related to respiratory depression due to sedatives or anesthetics used for MAC. Almost all MAC injury cases are believed to be preventable with the use of additional or better monitoring and an effective response to initial physiological derangement. Thus, it is essential to establish practical MAC guidelines and adhere to these guidelines strictly to reduce the occurrence of severe anesthesia-related adverse outcomes.
Over the last decade, there has been a tremendous increase in claims for medical negligence in our country. The number of annual malpractice lawsuits (civil suits other than criminal suits) has set new highs year after year, up from 1,000 in 2003. In the law, negligence is defined as a breach of duty to practice to the standard of care expected and which causes substantial injury to a patient [1].
As John Powell (US geologist, 1834-1902) said that the only real mistake is the one from which we learn nothing, it is a profession's responsibility to investigate adverse events, learn from them, and develop strategies to reduce their occurrence. A useful method to accomplish this is to investigate data provided in closed malpractice claims.
In the United States, this method was initiated by the American Society of Anesthesiologists Closed Claims Project (ASA-CCP) in 1985. The ASA-CCP has conducted annual reviews of anesthesia-related malpractice claims for 35 participating insurance carriers [2]. Hundreds of volunteer anesthesiologists reviewed case files and recorded findings using a standard data collection form [3]. To date, the ASA-CCP database contains the data for 8,954 claims [4], representing events occurring since 1962. Although the Korean Society of Anesthesiologists (KSA) started much later than the ASA, the KSA legislation committee was instituted in 2009 and has constructed a database using a standard data collection form. Unlike the closed-claims case files of the ASA-CCP, our data were obtained from expert consultation referrals on anesthesia-related issues, which were usually requested by the police departments, civil or criminal courts, or district health care centers, via the Korean Medical Association (KMA).
This study is the first report of the KSA legislation committee, in which we analyzed all surgical anesthesia cases (not including data related to the pain clinic) between December 2008 and October 2010.
Since 1994, the KSA has offered expert consultation service to police departments, civil or criminal courts, and district health care centers regarding anesthesia-related issues. A single legislation director was responsible for all these consultations before the legislation committee was constituted in July 2009. However, since the first constitution of the legislation committee, five members of the committee have reviewed case files and recorded findings using a standard data collection form as well as replying to each consultation referral. Although our committee was constituted in the middle of the 54th KSA term (December 2008-October 2010), the initial 20 case files of this term were incorporated into the database.
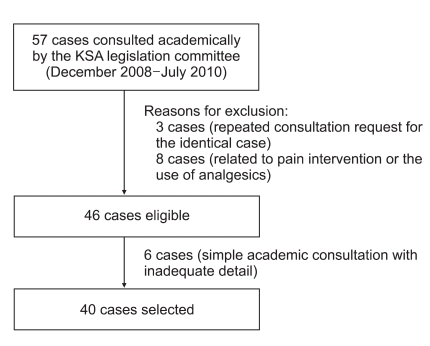
Between December 2008 and July 2010, 57 cases were referred to the KSA legislation committee for academic consultation. Of these cases, non-anesthetic cases and those arising in the pain clinic were excluded. Although 46 cases were eligible for analysis, six cases were excluded because of insufficient data to reconstruct the basic sequence of events or the nature of the injury. Finally, a total of 40 cases were included in the analysis (Fig. 1).
In each case, both office and hospital records were reviewed, as well as the testimony of the personnel involved. When available, autopsy reports were reviewed to confirm medical diagnoses and identify specific causation. Thereafter, the reviewers completed a standardized form to record information about patient characteristics, type of surgical procedure, anesthesia characteristics (type of anesthesia, anesthesia provider, drugs used, and intraoperative monitoring), timing and sequence of damaging events, outcomes, and a narrative summary for each case.
For the purposes of the analysis, outcomes were grouped into two categories: 'surviving/disabled' and 'dead'. The surviving/disabled group included a wide range of severity, from temporarily disabling to profound hypoxic brain damage. In cases of brain damage followed by death within 72 h, death was considered the outcome. Damaging events (the primary mechanism causing the injury) [5] were grouped into broad categories based on the physiological system or anesthesia technique implicated in the injury: respiratory system events, cardiovascular events, nervous events, allergic or adverse drug reactions, equipment problems, hepatic events, renal events, and thermal events [5]. For further analysis, the major damaging event categories were subcategorized into more specific areas, many of which are self-explanatory. Levels of intraoperative monitoring were classified into four grades (grade I, no monitoring; grade II, pulse oximetry ± noninvasive blood pressure; grade III, grade II + EKG; grade IV, grade III + capnography).
Categorical variables are described as numbers (%) and were compared using Pearson χ2-tests with a continuity correction or Fisher's exact tests, where applicable. The SPSS 13.0 package (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Statistical significance was defined as P < 0.05.
Of 40 surgical anesthesia cases, 29 (72.5%) resulted in death. As patient ages were widely distributed (range, 1-85-years), both surviving/disabled and dead patients showed a similar age distribution. The majority of patients were classified as ASA status I or II, with only three dead patients categorized as class III. Additionally, no difference existed in gender, anesthesia provider, types of anesthesia or hospital, or intraoperative monitoring level between surviving/disabled and dead patients (Table 1).
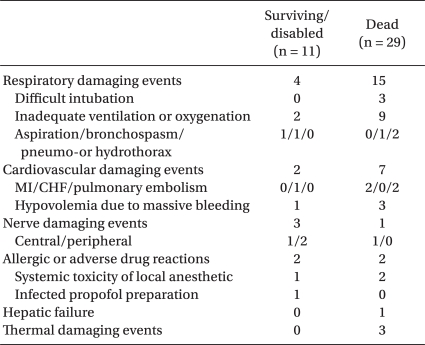
A respiratory event was the most common damaging event in both surviving/disabled and dead patients (36.4 vs. 51.7%, respectively; P > 0.05). In both groups, most respiratory damaging events (11/19, 57.9%) were related to inadequate ventilation or oxygenation. Three cases of "cannot ventilate/cannot intubate" situations, due to a difficult airway, and two cases of a pneumothorax or hydrothorax during central venous catheterization occurred only in dead patients (Table 2).
The percentage of death outcomes attributable to a cardiovascular event was 24.1% (7/29) (Table 2). In both groups, four cases of nerve damaging events were observed. More specifically, they were attributable to cauda equina syndrome after spinal anesthesia (one case), generalized seizure after spinal anesthesia (one case), and permanent brachial plexopathy after axillary block (two cases). Of thermal damaging events, two cases of malignant hyperthermia and one case of profound hypothermia were observed, all resulted in death.
In the order of frequency of cases, orthopedics (42.5%) was the most common department, and plastic surgery (17.5%) and general surgery (12.5%) were the next two (Fig. 2). More than one-third (35%) of incidents developed during anesthetic induction. Additionally, maintenance of anesthesia and recovery from anesthesia (emergence in operating room and at postanesthetic care unit) were similarly dangerous periods (30% vs. 25%, respectively; Fig. 3).
The police, prosecutors, and judges rely on expert opinions in most civil and criminal cases related to medical issues to judge potential medical negligence. As members of the medical community, patient advocates, and private citizens, anesthesiologists have ethical and professional obligations to assist the authorities in the administration of justice. Thus, the KSA has continued to reply these expert consultation referrals in a conscientious manner.
A single legislation director was responsible for all consultations before the constitution of the legislation committee. However, in July 2009, the legislation committee was first constituted to ensure the validity and impartiality of consistent consultation replies consistently and to share the heavy workload by establishing a five-member peer review system. Moreover, our committee is aimed at constructing the database from consultation referrals using a standard data collection form for further scientific research and academic activities. The KSA legislation committee prepared their first analysis report regarding surgical anesthesia between December 2008 and October 2010 and demonstrated several noteworthy findings from the analysis.
A respiratory event, which included both airway and pulmonary problems, represented the most frequent damaging event in both surviving/disabled and dead patients. These findings were consistent with those of studies in the US [5,6] and a previous Kwon study [7] in our country. In particular, the most common specific mechanism of these events (7 of 19 respiratory damaging events, 36.8%) was related to respiratory depression due to an absolute or relative overdose of sedatives or anesthetics during monitored anesthesia care (MAC). In all of these cases, surgeons or physicians provided MAC without the help of anesthesiologists. As a result, all but one case (profound brain damage) resulted in death. According to Bhananker et al. [2], who compared 121 MAC with 1,519 general anesthesia claims, the severity of injury for MAC claims was similar to that for general anesthesia claims, with a similar proportion of death and permanent brain damage. The reality in our country is that anesthesiologists have not been in charge of most MAC cases because of extremely low (roughly one-third) medical insurance fees versus those for general anesthesia. As the actual figure is believed to be larger than those sued, the government should adjust the MAC medical insurance fee to a realistic level.
Another remarkable finding was that three cases of 19 respiratory damaging events (15.8%) were attributed to difficult intubation, all of which led to death. Kwon, the former KSA legislative director, analyzed 145 cases of expert anesthesia-related consultation referrals between 1994 and 2006 and reported that five cases were attributable to difficult intubation [8]. Thus, the occurrence of major brain damage and death from difficult intubation has not decreased despite improved monitoring, devices, and equipment, when compared with that period. These major morbidities or mortalities attributable to difficult intubation could be reduced by careful preoperative airway assessment and strict adherence to practical guidelines for the management of a difficult airway [9,10]. The last updated ASA practical guidelines for managing a difficult airway were published in 1995 [10]. In fact, Peterson et al. [11] found that difficult airway claims associated with death or brain damage during induction decreased from 62% to 35% after publication of the ASA guidelines.
The use of MAC as the technique of choice for a variety of invasive or noninvasive procedures is increasing. However, given an Anesthesiology editorial [12] published in 2006 under the title, "MAC should stand for maximum anesthesia caution, not minimal anesthesiology care," potentially serious complications in association with MAC are well-known. One closed-claims analysis [2] suggested that claims associated with MAC showed a high degree of patient injury and a liability profile similar to claims associated with general anesthesia. In that study, the most common sources of injury during MAC were severe respiratory depression, resulting in death or brain damage, associated with the drugs used for sedation. Similarly, in this analysis, seven of ten MAC cases resulted in death or profound brain damage due to respiratory depression. Damaging events of the remaining three cases were systemic toxicity due to local anesthetics used concurrently (two cases) and septicemia from infected propofol-normal saline mixing solution (one case).
Most MAC cases are for simple or superficial operations that are regularly performed in a routine fashion in relatively healthy patients (ASA I or II patients). In this analysis, all patients were classified as ASA I or II (eight patients, ASA I; two, ASA II). Moreover, propofol and midazolam, the two most commonly used drugs in MAC cases, have safer pharmacokinetics than other sedatives and anesthetics. As such, they are considered to require simple, low-risk anesthesia care. Thus, a preoperative evaluation, such as a physical examination and preoperative laboratory tests, are often omitted, and intraoperative monitoring may be easily limited. Some practitioners explain the intraoperative experience to their patients as being similar to "taking a nap at a spa" and do not wish to upset their patients or drive them away to a competitor with the used of many preoperative evaluation procedures [12].
In this analysis, no preoperative laboratory tests were performed in half of the cases. In one case, no intraoperative monitoring was used. In half of the cases, pulse oximeter was the only monitoring instrument during the entire procedure. Despite patient safety benefits offered by pulse oximetry, an in-depth examination revealed that pulse oximetry was ineffective in some cases because the practitioner did not properly apply (inappropriate alarm setting or audible pulse tone off) or observe the results during the critical period. Because a practitioner cannot continuously observe oximetric values, vigilance necessitates an audible alarm or pulse tone that changes if oxygen saturation values decline.
Following general anesthesia, MAC was the second most common anesthetic technique leading to adverse outcomes in this analysis. The injury severity of MAC cases was comparable to general anesthesia cases, with 70% and 76.2% of the MAC and general anesthesia cases causing death, respectively. Furthermore, almost all injuries due to MAC in our database review were presumed to be preventable, with the use of additional or better monitoring and effective responses to adverse occurrences. Thus, MAC providers need to be aware of the risk of serious respiratory depression, and that continuous monitoring of ventilation and oxygenation, adequate resuscitation equipment, and constant vigilance are mandatory.
The most obvious difference between the previous report of Kwon [7] and our study was a marked decrease in obstetric anesthesia-related cases. While at least 18 cases (obstetric and gynecologic anesthesia-related cases were not described individually) occurred in the field of obstetric anesthesia in the former study, obstetric anesthesia-related cases were absent in this study. In our analysis, two cases of obstetrics and gynecology department (OB/GYN) occurred during dilation and curettage and gynecologic surgery. Although the relatively short evaluation period of this study may have affected the results, they may be primarily due to a combination of a decrease in the actual occurrence of obstetric anesthesiarelated adverse events and a decrease in the number of lawsuit cases (even if the occurrence of actual cases did not decrease).
However, the most likely explanation for these results is that our country has had the lowest birthrate in the world for the last decade. During this period, the birthrate decreased from an average of 1.45 babies per woman in 1998 to 1.08 babies per woman in 2008 [13]. Another possible explanation may be the local OB/GYN clinic's growing reluctance to deliver babies. As a result, most deliveries are performed in large specialized OB/GYN hospitals, general hospitals, and university hospitals. When compared with a local OB/GYN clinic, these hospitals maintain superior faculty, equipment, and systems for patient safety, thereby reducing the occurrence of adverse events. Moreover, if anesthesia-related morbidity or mortality developed, these hospitals may have greater ability to settle out of court than a local OB/GYN clinic. In contrast to our country's results, ASA-CCP closed-claims studies [14,15] have shown that even though the proportion of obstetric claims associated with maternal death decreased from pre-1990 and 1990 or later, the overall incidences of obstetric anesthesia-related claims remained unchanged during these periods (12% vs. 13%, respectively).
As an introduction to understanding our data, several major limitations must be recognized. Most important is that we cannot derive information about the actual incidence of adverse events and total numbers of anesthesia cases in specific situations. For any given time period, we only see expert consultation referrals of anesthesia-related issues from police departments, civil or criminal courts, and district health care centers via the KMA. The vast majority of injured patients do not file claims. Thus, these inherent limitations make it impossible to provide any numeric estimates of the risk for specific clinical situations. Second, the data were collected from in a retrospective manner directly from participant, and the database only has information that the reviewers could obtain from police or prosecutor records. The incompleteness of specific detailed information regarding the sequence of events or mechanism of injury makes this analysis weaker than prospectively collected data. Third, bias should also be expected in the original medical records and other case documentations, because the preparer could not be impartial [16].
However, the usefulness of this database research is evident. Prospective clinical studies may be very expensive and ethically impossible for extremely rare and fatal events, such as anesthesia-related death. A comprehensive review of expert consultation referrals and their attached references offer an alternative and concentrated data source to examine possible causes, precipitating events, and outcomes in the field of anesthesia. The insights gained from analyzing these data will continue to provide important contributions toward ensuring patient safety.
In summary, respiratory events represented the most frequent damaging event in both surviving/disabled and dead patients. More specifically, the most common mechanism for these events was related to respiratory depression due to sedatives or anesthetics used for MAC. Almost all injuries attributable to MAC were presumed to be preventable with additional or better monitoring and providing effective responses to adverse occurrences. Thus, it can be concluded that there is room for further reductions in the occurrence of severe anesthesia-related adverse outcomes by establishing practical guidelines for MAC and ensuring strict adherence to these guidelines.
References
1. Brazier M. Brazier M, editor. Medical negligence. Patients and the Law. 1992. 1st ed. Medicine: Penguin Books;p. 112–139.
2. Bhananker SM, Posner KL, Cheney FW, Caplan RA, Lee LA, Domino KB. Injury and liability associated with monitored anesthesia care: a closed claims analysis. Anesthesiology. 2006; 104:228–234. PMID: 16436839.
3. Cheney FW. The American Society of Anesthesiologists Closed Claims Project: what have we learned, how has it affected practice, and how will it affect practice in the future. Anesthesiology. 1999; 91:552–556. PMID: 10443619.
4. American Society of Anesthesiologists Closed Claims Project. Available from http://depts.washington.edu/asaccp/ASA/index.
5. Cheney FW, Posner KL, Lee LA, Caplan RA, Domino KB. Trends in anesthesia-related death and brain damage: a closed claims analysis. Anesthesiology. 2006; 105:1081–1086. PMID: 17122570.
6. Caplan RA, Posner KL, Ward RJ, Cheney FW. Adverse respiratory events in anesthesia: a closed claims analysis. Anesthesiology. 1990; 72:828–833. PMID: 2339799.

7. Kwon MI. The analysis of 137 anesthesia-related adverse outcome cases in Korea. Korean J Anesthesiol. 2004; 46:83–90.

8. Kwon MI. The types of medical accidents and strategies for prevention: focused in medical accidents occurred in anesthetic and surgical fields. Korean J Anesthesiol. 2007; 53:555–564.
9. Henderson JJ, Popat MT, Latto IP, Pearce AC. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia. 2004; 59:675–694. PMID: 15200543.
10. American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003; 98:1269–1277. PMID: 12717151.
11. Peterson GN, Domino KB, Caplan RA, Posner KL, Lee LA, Cheney FW. Management of difficult airway: a closed claims analysis. Anesthesiology. 2005; 103:33–39. PMID: 15983454.
12. Hug CC Jr. MAC should stand for Maximum Anesthesia Caution, not Minimal Anesthesiology Care. Anesthesiology. 2006; 104:221–223. PMID: 16436837.

13. Korean Social trends 2009. Statistical Research Institute. Available from http://sri.kostat.go.kr/sri/paper/paperAction.do?method=view&p_idx=187&catgrp=ksri&catid1=ksri01&catid2=ksri01c.
14. Chadwick HS, Posner K, Caplan RA, Ward RJ, Cheney FW. A comparison of obstetric and nonobstetric anesthesia malpractice claims. Anesthesiology. 1991; 74:242–249. PMID: 1990900.

15. Davies JM, Posner KL, Lee LA, Cheney FW, Domino KM. Liability associated obstetric anesthesia: a closed claims analysis. Anesthesiology. 2009; 110:131–139. PMID: 19104180.
16. Jordan LM, Kremer M, Crawforth K, Shott S. Data-driven practice improvement: the AANA Foundation closed malpractice claims study. AANA J. 2001; 69:301–311. PMID: 11759368.
Fig. 2
Analysis of involved clinical departments. PS: plastic surgery, OS: orthopedic surgery, GS: general surgery, IM: internal medicine. Others include thoracic surgery, urology, otorhinolaryngology, and dermatology. Numbers in parentheses indicate the number of cases.
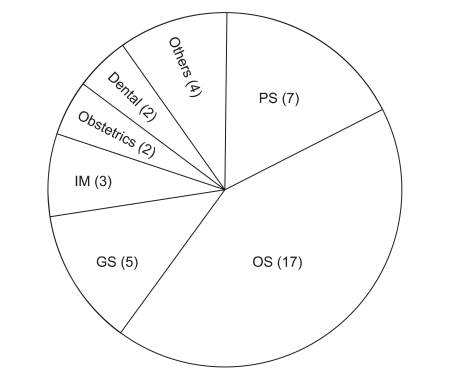
Fig. 3
Analysis of the timing of damaging events. PACU: postanesthetic care unit. Numbers in parentheses indicate the number of cases.
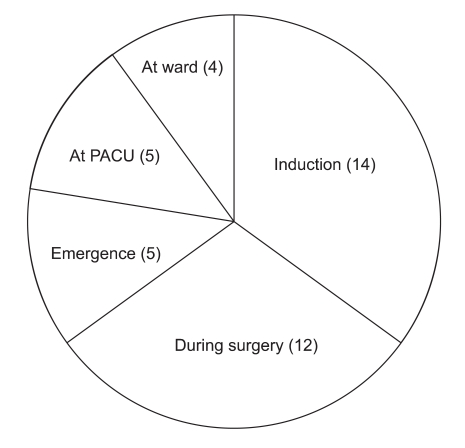
Table 1
General Data for Surviving/Disabled and Dead Patients
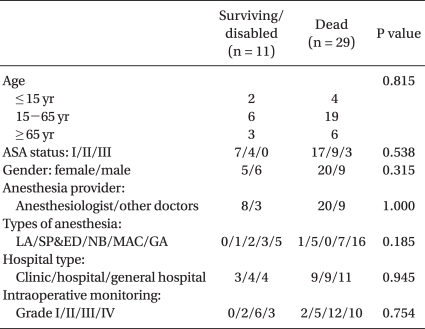
Values are expressed as numbers of cases. LA: local anesthesia, SP: spinal anesthesia, ED: epidural anesthesia, MAC: monitored anesthesia care, GA: general anesthesia. Intraoperative monitoring; grade I: no monitoring; grade II: pulse oximetry ± non-invasive blood pressure; grade III: grade II + EKG, grade IV: grade III + capnography.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download