Abstract
An 82-year-old female, with left femoral neck fracture was scheduled for left hip hemiarthroplasty, under spinal anaesthesia. She had been suffering from diabetes, hypertension, lung cancer and was previously treated with IV aminophylline for respiratory insufficiency. She was given spinal anaesthesia with 10 mg of 0.5% hyperbaric bupivacaine, and T6 sensory block level was established. After 10 minutes, her blood pressure dropped to 80/60 mmHg, so intravenous ephedrine was given. At that moment, multifocal atrial tachycardia (MAT) appeared on electrocardiogram (ECG). Intravenous infusion of phenylephrine and procainamide was given and conversion of MAT to sinus rhythm was successfully achieved. We report a case of MAT after spinal anaesthesia, in a patient with respiratory insufficiency previously treated with IV aminophylline, which was successfully treated by intravenous infusion of phenylephrine and procainamide.
Go to : 
The term multifocal atrial tachycardia (MAT) was first used in 1968, but this rhythm has been described previously by names such as chaotic atrial tachycardia, chaotic atrial rhythm and repetitive paroxysmal MAT. The prevalence rate of MAT is 0.05-0.32% and the average age of occurrence is 72 years. MAT is commonly observed in elderly people with underlying illnesses like chronic obstructive lung disease or congestive heart failure and is strongly associated with aminophylline use [1]. The authors of this study conducted experiments in elderly patients in whom intravenous aminophylline was used for the purpose of treating respiratory failure. It was observed that after aminophylline was used intravenously along with spinal anaesthesia, hypotension and MAT developed at the same time and, after an intravenous injection of phenylephrine and procainamide, these conditions returned to normal. This experience based upon the experiments is reported here along with literature reviews.
An 82-year-old female patient with a left femoral neck fracture was scheduled for left hip hemiarthroplasty. She had been under treatment for diabetes and hypertension for 10 years and, 2 years ago lung cancer had been detected but was conducted without any treatment. Before the operation, the patient complained of difficulty in breathing, however she went through the operation without much difficulty. During physical examination, on auscultation of the respiratory system, wheezes were detected in both the lungs.
Preoperative blood tests revealed C-reactive protein (CRP) of 9.7 mg/dl, White Blood Cell count (WBC) of 16,100/mcl, Sodium (Na+) level of 132 mEq/L, Potassium (K+) 5.5 mEq/L, Chloride (Cl-) 98 mEq/L, Calcium (Ca2+) 8.9 mg/dl. On ECG, the patient's heart rate was normal with a heart rate of 83 beats/min, and on echocardiogram left ventricular ejection fraction was 74%, showing mild pulmonary valve regurgitation. On chest X-ray, 7 metastatic nodules of 9 cms each in size were. Arterial blood gas analysis showed pH of 7.42, PaCO2 of 24.5 mmHg, PaO2 of 53.9 mmHg and, Oxygen saturation level of 88%, which was considered as hypoxemia. The patient was injected intravenously with aminophylline 250 mg diluted in 500 ml 5% dextrose normal saline to run at 20 ml/hr. The intravenous injection of aminophylline was discontinued before she went into the operating room. The patient was taking formoterol ventolin nebulizer whenever she suffered from shortness of breath.
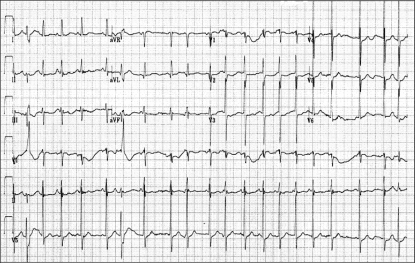
Upon arrival in the operating room, the patient's heart rate was 105 beats/min, blood pressure was 140/80 mmHg, oxygen saturation level was 92%, at which point the oxygen mask was put on. The oxygen saturation level was maintained above 98%. Patient was placed in the right lateral decubitus position when 10 mg of 0.5% hyperbaric bupivacaine and fentanyl 10 µg were injected directly into the subarachnoid space at the L4/L5 vertebral level. After 10 minutes, the sensory block was at the sixth thoracic segmental level. Blood pressure was continuously monitored in the left wrist through the 20 G radial artery catheter. 10 minutes after spinal anaesthesia, blood pressure decreased from 140/80 mmHg to 80/50 mmHg and heart rate increased from 105 beats/min to 130-140 beats/min. We considered this as reflex tachycardia following hypotension. In order to increase the blood pressure 4 mg ephedrine was injected intravenously. Immediately MAT developed, so 12-lead ECG was performed (Fig. 1). Esmolol 10 mg was intravenously administration; used to decrease the heart rate, but the heart rate did not decrease; MAT was continuous and, systolic blood pressure was between 60-80 mmHg. The patient did not complain of anything particularly difficult. At this time arterial blood gas analysis was performed and it showed a pH of 7.42, PaCO2 of 27 mmHg, PaO2 of 109 mmHg and, oxygen saturation level of 99%. In order to compensate for the decreased vascular resistance due to spinal anaesthesia, infusion of norepinephrine 8 mg diluted in 500 ml of 0.9% saline solution to run at the rate of 20 ml/hr was given and increased blood pressure was 190/140 mmHg or more and arrhythmia was worsen. After, discontinuing norepinephrine infusion, systolic blood pressure decreased again and was between 60-80 mmHg.
In order to correct this severe hypotension which is the risk factor of MAT, pure α-receptors agonist, phenylephrine 10 mg in 500 ml 0.9% saline solution was given intravenously to run at 30 ml/hr, and was slowly increased to 180 ml/hr. The systolic blood pressure also increased slowly from 60-80 mmHg to 100 mmHg. However, after the correction of hypotension and MAT were not improved. Because of persistent arrhythmia lasting for more than 1 hour, surgery could not be started and therefore other medications such as antiarrhythmics were considered. To lower the excitability of the heart, 100 mg procainamide without any α-receptor blocking effects was diluted in 40 ml 0.9% saline solution to run at 50 ml/hr intravenously, was started. After 10 minutes of intravenous procainamide infusion, conversion to sinus rhythm was achieved and, procainamide was given at the rate of 10 ml/hr until the heart rate decreased gradually to 90 beats/minute. Soon after the operation was begun and it ended after an hour. In the recovery room, procainamide was infused at a rate of 10 ml/hr for a period of one hour. Phenylephrine dose was also injected intravenously and, the rate of infusion was gradually decreased after a period of two hours. In the recovery room, aminophylline blood level measured was 21 µg/dl. On ECG, the patient showed a normal sinus rhythm with a heart rate of 83 beats/ minute and was discharged after 7 days.
Go to : 
ECG features of MAT include a heart rate greater than 100 beats/min, three or more different forms of P waves and, irregular P-P intervals [2]. The mechanism of MAT is thought to be a triggered activity. The risk factors for MAT are: theophylline toxicity, catecholamine excess, hypoxemia, acidosis and electrolyte imbalance. Intracellular calcium overload by various mechanisms like catecholamine excess, acidosis, hypoxemia, phosphodiesterase inhibition promoting the delay, resulting in delayed afterdepolarization are postulated in the development of MAT. MAT can also develop postoperatively while recovering from a surgery or during postoperative infections like postoperative pneumonia, atelectasis and, pulmonary embolism.
In this case, the cause of MAT initially was, thought to be hypoxia caused by the acute exacerbation of chronic respiratory failure. This patient with lung cancer had experienced respiratory failure due to chronic obstructive pulmonary disease (COPD) which was in a severe stage and wheezes were detected in both the lungs. In patients with MAT, COPD is the most commonly associated cardiopulmonary illness. Chronic obstructive pulmonary disease are the most common conditions in MAT patients [3]. Hypoxemia is common in patients with MAT, and hypoxemia stimulates the production of catecholamines which promotes the development of MAT [3,4]. In the morning of operation, the patient was hypoxemic and her arterial blood gas analysis showed an oxygen saturation level of 88%, PaO2 of 53.9 mmHg. However on pulse oxymetry in the operating room, oxygen saturation level was 92% and improvement of hypoxemia was seen with this increase in the oxygen saturation level. Thus, it is difficult to adjudge hypoxemia as the main cause of MAT.
The second cause of MAT was thought to be the use of aminophylline and β-receptor agonist which were given to the patient before the operation. The patient was given formoterol (long acting β2-receptor agonist) oral administration, salbutamol sulfate inhaler, and other aminophylline treatments which were continued until the morning of the surgery. Aminophylline considered a positive chronotrope increases the heart rate, and the dose of aminophylline increases with an increase in the heart rate [5]. This enhances the atrial automaticity and intracardiac conduction which increase the chances of MAT, atrial fibrillation, supraventricular tachycardia, ventricular tachycardia and so on [6]. Levine [7] reported that MAT was observed in 16 patients during theophylline use and, after theophylline use was discontinued MAT disappeared. Again after aminophylline treatment was restarted in 5 patients, they showed a recurrence of MAT. Also since, elderly patients eliminate aminophylline more slowly than younger patients, it leads to toxicity due to the high aminophylline blood levels. Weinberger and Hendeles [8] reported that serum aminophylline concentration of 20 µg/dl will show side effects in more than 28% of the children, and 67% of the adults. However, if a beta receptor agonist is used when the serum aminophylline concentration level is 5-10 µg/dl, this level is also enough to give side effects [9].
The third cause of MAT was thought to be the spinal anaesthesia given for surgery which lead to hypotension. Upon arrival in the operating room, the heart rate was 105 beats/min due to aminophylline, β-receptor agonist, hypoxemia and, excess catecholamine production in response to pain. 10 minutes after spinal anaesthesia, blood pressure decreased from 140/70 mmHg to 80/50 mmHg. After the patient suffered with the left hip fracture, she went into a hypovolemic state due to loss of appetite, pain and, blood loss. However, the blood pressure was maintained because of the acute pain but after spinal anaesthesia, blood pressure dropped significantly and severe hypotension developed. Reflex tachycardia and hypotension developed. In order to raise the blood pressure, ephedrine (β-receptor agonist) 4 mg intravenous injection was given and MAT developed suddenly. In the state of reflex tachycardia, triggered activity from use of the β-receptor agonist have been caused. Braun et al. [10] has stated that for treating hypotension developing after spinal anaesthesia, catecholamine injection can increase the pulmonary vascular resistance which is also likely to cause pulmonary heart failure. Therefore in patients with the risk factor of developing pulmonary hypertension due to hypoxemia, the use of vasopressin was recommended to correct the hypotension developing after spinal anaesthesia.
The fourth cause of MAT was thought to be the diabetic autonomic neuropathy. In this case, although there is no evidence that the patient was suffering from diabetic autonomic neuropathy before surgery, however within 2 years after the onset of diabetes, dysfunction develops in the autonomic nervous system and dysfunction of cardiovascular regulation can develop in patients without a clinically significant dysfunction in the autonomic nervous system. In diabetic patients, because baroreflex is disrupted after the induction of anaesthesia and thus cannot compensate for sudden changes in vascular resistance, leading to hypotension. In addition parasympathetic nervous system disorders are observed in many diabetic patients and, the dominance of the sympathetic nervous system causes tachycardia in sympathetic nerve endings decreasing the reabsorption of norepinephrine and, therefore the catecholamine receptors showed hypersensitivity [11]. The case of a patient with disrupted baroreflex can cause hypotension with tachycardia due to sympathetic dominance and, ephedrine (β-receptor agonist) injection can cause excess catechcolamine production leading to MAT.
Treatment of MAT involves the correction of the precipitating factors. MAT is most often transient and by treating the underlying conditions like hypoxemia, electrolyte imbalance, congestive heart failure and, chronic obstructive pulmonary disease, there is a better chance of resolving MAT naturally. When aminophylline and β-receptor agonist are used in combination, the quantity of the drugs must be reduced or they should be totally discontinued, as these drugs increase the catecholamine production which causes the triggered activity.
If MAT or the cardiovascular instability continues even after adjusting and treating the causes, antiarrhythmic treatment can be considered. The β-receptor antagonist as the antiarrhythmic treatment of MAT should be considered as the first-line therapy. However, β-receptor antagonist can causes bronchial spasms, hypotension and therefore they have a limited use. Next, use of high-dose magnesium (Mg2+) may be considered. Mg2+ is an antagonist of Ca2+ in the myocyte and by suppressing Ca2+ influx, it inhibits intracellular Ca2+ overload which is useful in inhibiting the delay afterdepolarization. Use of Mg2+ in patients must be done with caution as side effects such as renal failure, headache, skin rash and, hypotension can develop. Verapamil may cause hypotension, but hypoxic pulmonary vasoconstriction can aggravate the hypoxemia. Mechanism of action of metoprolol, verapamil, magnesium, is not by suppression of atrioventricular conduction (AV conduction) and other cycles, but by suppression of the atrial ectopic beat thereby decreasing the ventricular rate. Patients with MAT were injected with flecainide [12], ibutilide [13] and the inhibition mechanism of afterdepolarization which is thought to interfere with the arrhythmia was studied. Digoxin does not help in converting to normal sinus rhythm as decreasing the AV conduction has no effect on the slow down of MAT. MAT is not responsive to electric cardioversion. This is a main difference between MAT and atrial fibrillation. Hence, MAT erroneously diagnosed as atrial fibrillation should be treated with more caution.
In this case, phenylephrine was used as a pure α-receptor agonist and was not used for increasing the heart rate. For patients with respiratory failure being treated with intravenous injection of aminophylline and β-receptor agonist, must be treated carefully by decreasing the dose of β-receptor agonist when treating hypotension after spinal anaesthesia. As an alternative treatment, pure α-receptors agonist such as phenylephrine or vasopressin without any catecholamines should be considered for use. In many cases, there was disappearance of MAT on ECG as aminophylline levels decreased over time. Plasma half life of aminophylline is approximately 8 hours, but it is different in each person, and serum half life is increased and clearance is decreased in the elderly patients. In this case since MAT lasted for more than 1 hour, antiarrhythmics were considered as an alternative treatment option in order to start the operation. Nonselective β-receptor antagonist can cause bronchial spasms and hence were not given. High dose Mg2+ treatment was not given since the patients Mg2+ levels were not low and there can be side effects in the elderly patients due to decreased Mg2+ excretion. Amiodarone and verapamil can cause hypotension and hence were not given. They are not given with the selected class 1a procainamide to suppress the excitability of the heart. Procainamide decreases the threshold of abnormal automaticity in the ectopic site by increasing the threshold of the atria ventricles and, the Purkinje fibers thereby suppressing the excitability of the heart. Procainamide's major active metabolite, N-acetyl procainamide, a strong class III antiarrhythmic, which has an inhibitory action on K+ channel by increasing the action potential period and refractory period and by increasing the suppression of the excitability of the heart [14].
If β2-receptor agonist and aminophylline are being given in combination during spinal anaesthesia, hydration must be prepared well in advance to reduce the chances of development of hypotension. Also, phenylephrine or vasopressin given as a support is effective in preventing cardiac excitability due to hypotension and reflex tachycardia. If diabetes is associated with disrupted baroreflex, more severe hypotension can develop. Also, parasympathetic nervous system may be disordered, and there may be sympathetic hypersensitivity to the tachycardia, and arrhythmias may respond during haemodynamic monitoring and intra operative haemodynamic instability. Therefore, it is necessary to be prepared for prevention of MAT and use of antiarrhythmics may be considered helpful in case of continuation of MAT.
Go to : 
References
2. Sessler CN, Cohen MD. Cardiac arrhythmias during theophylline toxicity. A prospective continuous electrocardiographic study. Chest. 1990; 98:672–678. PMID: 2394145.
3. Arsura EL, Solar M, Lefkin AS, Scher DL, Tessler S. Metoprolol in the treatment of multifocal atrial tachycardia. Crit Care Med. 1987; 15:591–594. PMID: 3568727.

4. Adamantidis MM, Caron JF, Dupuis BA. Triggered activity induced by combined mild hypoxia and acidosis in guinea-pig Purkinje fibers. J Mol Cell Cardiol. 1986; 18:1287–1299. PMID: 2434659.

5. Lee JH, Choi YH, Choi SK, Kim DS, Yoo WS. Effect of fenoterol and aminophylline on the incidence of cardiac arrhythmia. Korean J Intern Med. 1988; 35:811–820.
6. Vestal RE, Eiriksson CE Jr, Musser B, Ozaki LK, Halter JB. Effect of intravenous aminophylline on plasma levels of catecholamines and related cardiovascular and metabolic responses in man. Circulation. 1983; 67:162–171. PMID: 6336606.

7. Levine JH, Michael JR, Guarnieri T. Multifocal atrial tachycardia: a toxic effect of theophylline. Lancet. 1985; 1:12–14. PMID: 2856947.

8. Weinberger M, Hendeles L. Slow-release theophylline rationale and basis for product selection. N Engl J Med. 1983; 308:760–764. PMID: 6828122.

9. Wolfe JD, Tashkin DP, Calvarese B, Simmons M. Bronchodilator effects of terbutaline and aminophylline alone and in combination in asthmatic patients. N Engl J Med. 1978; 298:363–367. PMID: 340945.

10. Braun EB, Palin CA, Hogue CW. Vasopressin during spinal anesthesia in a patient with primary pulmonary hypertension treated with intravenous epoprostenol. Anesth Analg. 2004; 99:36–37. PMID: 15281498.

11. Dejgaard A, Andersen P, Hvidberg A, Hilsted J. Cardiovascular, metabolic, and hormonal responses to noradrenaline in diabetic patients with autonomic neuropathy. Diabet Med. 1996; 13:983–989. PMID: 8946158.

12. Barranco F, Sanchez M, Rodriguez J, Guerrero M. Efficacy of flecainide in patients with supraventricular arrhythmias and respiratory insufficiency. Intensive Care Med. 1994; 20:42–44. PMID: 8163757.

13. Pierce WJ, McGroary K. Multifocal atrial tachycardia and ibutilide. Am J Geriatr Cardiol. 2001; 10:193–195. PMID: 11455238.

14. Komeichi K, Tohse N, Nakaya H, Shimizu M, Zhu MY, Kanno M. Effects of N-acetyl procainamide and sotalol on ion currents in isolatedguinea-pig ventricular myocytes. Eur J Pharmacol. 1990; 187:313–322. PMID: 1705889.
Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download