Abstract
Pneumocephalus is a condition which usually results from head trauma. It has been known that iatrogenic pneumocephalus can occur as a complication of positive pressure mask ventilation during induction of anesthesia or ventilatory care for head trauma patients. We report a case of mask ventilation during anesthesia induction in a 50-year-old male patient with head trauma. Initial pneumocephalus associated with cerebrospinal fluid leakage was diagnosed immediate following head injury involving facial sinuses. He was managed with emergent lumbar drainage and supportive care. Pneumocephalus recurred following positive pressure mask ventilation (PPMV) during anesthesia induction for surgery on the right arm. Recurred pneumocephalus was managed with high flow oxygen and supportive care. Anesthesiologists should be aware of pneumocephalus as a potential complication of PPMV in head trauma patients, even after resolution of previous pneumocephalus.
Go to : 
Pneumocephalus is defined as the presence of air in the cranial cavity. The usual causes of pneumocephalus are traumatic facial fractures involving the ethmoidal or frontal sinuses [1]. Untreated pneumocephalus can progress to tension pneumocephalus, manifested as severe headache, dizziness, nerve palsy, mental changes and even seizure, therefore urgent diagnosis and treatment are mandatory. Rare causes of pnuemocephalus have been reported as a complication of positive airway pressure mask ventilation (PPMV) [2]. Positive pressure in the upper airway can force air into the skull through any openings of the facial bone.
We report a case of recurred pneumocephalus after PPMV for anesthesia induction for combined arm fracture in a head trauma patient. We highlight the importance of preventing pneumocephalus as a complication of PPMV in patients with facial bone trauma.
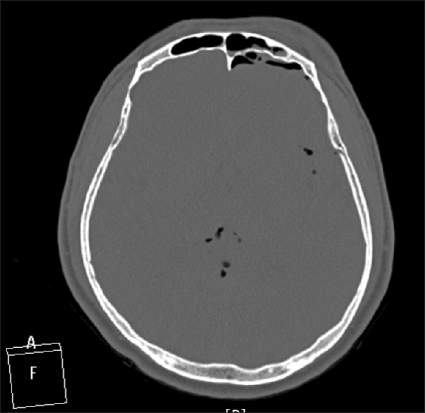
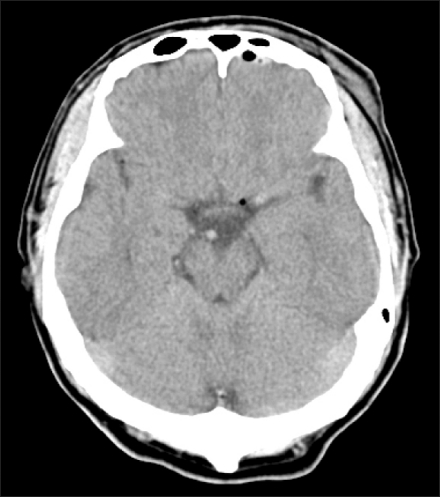
A 50-year-old, 168 cm, 68 kg man without significant past medical history, was admitted to emergency room following a slip-down accident. On admission, the patient was alert and complained of moderate headache and dizziness. Cerebrospinal fluid (CSF) rhinorrhea and the left periorbital swelling were noted. Neurologic examination confirmed a Glasgow coma scale (GCS) of 15, and the pupils were symmetrical and reactive. Emergent skull X-ray series, facial computerized tomography (CT) and forearm X-ray revealed fracture of the frontal sinus, skull base, and right distal radius fracture. Computed tomography (CT) of the brain showed multiple small subdural pneumocephalus (Fig. 1). Emergent lumbar drainage was performed to manage CSF rhinorrhea and empirical prophylactic antibiotic treatment was given. Pneumocephalus subsided spontaneously within 7 days as confirmed by repeat CT scan (Fig. 2). With conservative treatment the patient's post-traumatic symptoms improved gradually in the surgical intensive care unit.
At post-trauma 8 days, following trauma, the patient underwent orthopedic surgery for distal radius fracture under general anesthesia. Preoperative laboratory findings were unremarkable. Intramuscular glycopyrrolate 0.2 mg was administered as premedication. Standard monitoring including BIS (A-2000 BIS XP: Aspect Medical System Inc. Natick, MA, USA) was applied before anesthesia induction. Anesthesia was induced with intravenous thiopental 300 mg and 0.5 µg/kg/min remifentanil infusion. Endotracheal intubation was performed after administering 50 mg rocuronium injection with 100% oxygen mask ventilation for 3 min without any difficulties. Anesthesia was maintained with oxygen (2 L/min)-air (2 L/min)-sevoflurane (1-1.5 vol%), continuous infusion of 0.125-0.5 µg/kg/min remifentanil and 10-15 mg/h of rocuronium. Tidal volume and respiratory rate were adjusted to maintain end-tidal carbon dioxide tension at 30-35 mmHg. The 3-hour operation was uneventful. Following surgery, the patient was extubated in the operation room after gaining consciousness and spontaneous ventilation. He was then transferred to the post-anesthesia care unit where he recovered fully without complications.
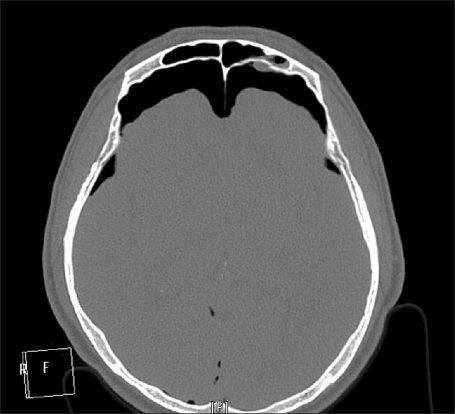
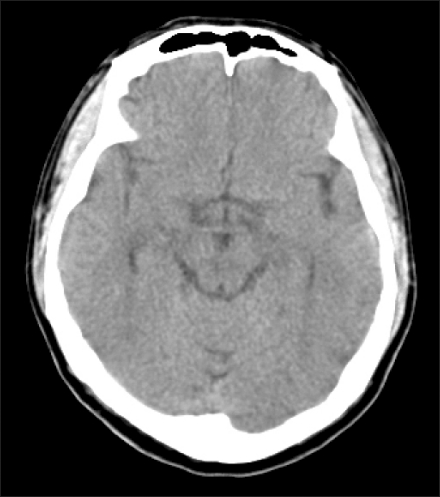
Ten hours later, the patient complained of severe, increasing, headache and exhibited abrupt deterioration in mental state. In view of his clinical aggravation, tension pneumocephalus was suspected. Neurologic examination demonstrated a GCS 11 and emergent brain CT showed large quantity of both frontal and right occipital pneumocephalus (Fig. 3). PPMV during anesthesia induction was suspected to be the cause of recurred pneumocephalus. High flow (8 L/min) oxygen via a partial non-rebreathing mask was administered in conjunction with supportive care for 2 days. The condition of the patient improved gradually and his GCS subsequently normalized. The last CT (Fig. 4) performed 16 days following the operation revealed complete resolution of pneumocephalus. No infectious neuromeningeal complications occurred during hospitalization, and the patient was discharged at post-trauma day 32.
Go to : 
Intracranial pneumocephalus is sterile accumulation of air within the cranial cavity. It develops mostly from acute and subacute complications of head trauma, or as late complications during the recovery phase of head injury. Subarachnoid or subdural air accumulation is the most common form of pneumocephalus, and intracerebral pneumocephalus can occur albeit rarely. Intracranial air is accumulated as a result of communications between paranasal sinuses, mastoid air cells and the cranial fossa, associated with dural tear. The other mechanism of air penetration is a ball-valve effect like sudden increase of nasopharyngeal pressure, such as during coughing and sneezing, forcing air into the cranial cavity which subsequently remained trapped [3]. Injuries of the paranasal sinuses, which are closely contiguous to bony structures, the dura mater and the brain frequently accompany head traumas. Frontal pneumocephalus is the most common type of pneumocephalus. 75-90% of pneumocephalus are posttraumatic and the incidence of pneumocephalus secondary to head injury range from 0.5% to 13.2% [3,4]. Other causes include facial tumors that eroded through the skull, gas-forming bacterial infections, paranasal sinusitis and neurosurgical and facial procedures [5].
Pneumocephalus is mostly asymptomatic and self-limiting, because gas is not irritating to the surrounding brain. Intracerebral pneumocephalus have usually become sizable when it is confirmed by simple skull x-ray or brain CT. The clinical manifestations of pneumocephalus include headaches, dizziness, cranial nerve palsies. Tension pneumocephalus caused by large amounts air can evoke sudden or insidious mass effects capable of shifting midline structures, causing major neurological deficits. Therefore, tension pneumocephalus needs prompt diagnosis and management to avoid permanent neurological damage.
There have been many cases of iatrogenic or barotrauma-related pneumocephalus [2,6]. Representable iatrogenic pneumocephalus are related to positive pressure ventilation in the upper airway, such as nasal continuous positive airway pressure, face mask ventilation and even nasal oxygen cannulae [7]. It is well known that positive airway pressure can result in pneumothorax, pneumomediastinum and subcutaneous emphysema [8]. It is difficult to predict which head trauma patients who do not initially develop pneumocephalus will experience iatrogenic pnemocephalus during positive pressure oxygen therapies. The mechanism of air delivered via manually operated mask tracking into the cranial cavities appears to be identical to that in traumatic pneumocephalus [2]. Because CSF leakage is usually a result of osteomeningeal fistula, CSF rhinorrhea is commonly associated with pneumocephaus, as demonstrated in this patient. His initial primary pneumocephalus accompanied by rhinorrhea was completely subsided following lumbar drainage and general supportive care, but post-anesthetic secondary pneumocephalus probably developed during anesthesia induction using PPMV. Therefore, avoidance of excessive positive pressure during mask ventilation is recommended to prevent pneumocephalus.
Because most mild pneumocephalus usually recover spontaneously within one week, its management includes strict bed rest in the semi-fowler position, analgesia and antibiotics. Prevention of intracranial pressure elevation by avoiding the Valsalva maneuvers, coughing, sneezing, nose blowing, and excessive physical activities is important to avoid pneumocephalus aggravation [6]. Because severe headache, personality change, disorientation, and mass effect associated with midline structure shift are the symptoms and signs of tension pneumocephalus, emergent surgical procedures, such as subdural drainage to decrease intracranial pressure, should be considered immediately after confirming the diagnosis with X-rays or brain CT [9]. When the patient experienced severe headache and became rapidly lethargic, analgesia, antibiotic and high flow, high FiO2 oxygen via a partial non-rebreathing reservoired mask were administered under a presumed diagnosis of impending tension pneumocephalus. The management principle is as follows: high FiO2 oxygen reduces blood and brain tissue nitrogen concentration, thereby increases the nitrogen concentration gradient that promotes pneumocephalus gas absorption [10].
To avoid tension pneumocephalus in head trauma patients, LMA or tracheostomy tube intubation can be applied with rapid sequence induction using fast onset muscle relaxants without PPMV [11]. In addition, anesthesiologists should be aware of potential complications caused by low intracranial pressure during anesthesia in head trauma patients. In theory, hypotension, hypovolemia, excessive hypercapnia and head-up position during anesthesia can reduce intracranial pressure that facilitates air influx through open osteomeningeal fistulae secondary to head trauma, causing pneumocephalus.
In conclusion, anesthesiologists and surgeons should be aware of pneumocephalus as a potential complication during positive pressure mask ventilation for facial trauma, secondary to air invasion through osteomeningeal fistulae. Close monitoring for pneumocephalus development should be mandatory following general anesthesia or during respiratory care with continuous positive airway pressure in head trauma patients.
Go to : 
Notes
This was presented at the 86th Annual Scientific Meeting of the Korean Society of Anesthesiologists, 2009, International Convention Center, Jeju, Korea.
Go to : 
References
1. Mendelsohn DB, Hertzanu Y. Intracerebral pneumatoceles following facial trauma: CT findings. Radiology. 1985; 154:115–118. PMID: 3964928.

2. Dacosta A, Billard JL, Gery P, Vermesch R, Bertrand M, Bertrand JC. Posttraumatic intracerebral pneumatocele after ventilation with a mask: case report. J Trauma. 1994; 36:255–257. PMID: 8114148.
3. Orebaugh SL, Margolis JH. Post-traumatic intracerebral pneumatocele: case report. J Trauma. 1990; 30:1577–1580. PMID: 2258975.
4. Lewin W. Cerebrospinal fluid rhinorrhea in nonmissile head injuries. Clin Neurosurg. 1964; 12:237–252. PMID: 5865043.

5. Davis DH, Laws ER Jr, McDonald TJ, Salassa JR, Phillips LH 2nd. Intraventricular tension pneumocephalus as a complication of paranasal sinus surgery: case report. Neurosurgery. 1981; 8:574–576. PMID: 7266798.
6. Jarjour NN, Wilson P. Pneumocephalus associated with nasal continuous positive airway pressure in a patient with sleep apnea syndrome. Chest. 1989; 96:1425–1426. PMID: 2684559.

7. O'Brien BJ, Rosenfeld JV, Elder JE. Tension pneumo-orbitus and pneumocephalus induced by a nasal oxygen cannula: report on two paediatric cases. J Paediatr Child Health. 2000; 36:511–514. PMID: 11036813.
8. Kramer NR, Fine MD, McRae RG, Millman RP. Unusual complication of nasal CPAP: subcutaneous emphysema following facial trauma. Sleep. 1997; 20:895–897. PMID: 9415951.
10. Dexter F, Reasoner DK. Theoretical assessment of normobaric oxygen therapy to treat pneumocephalus. Anesthesiology. 1996; 84:442–447. PMID: 8602677.

11. Hatcher IS, Stack CG. Pneumocephalus complicating general anaesthesia in a nine-year-old child. Paediatr Anaesth. 1999; 9:265–267. PMID: 10320609.

Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download