Abstract
Background
There is a legal obligation to explain the procedure and use of epidural analgesia in labor primarily due to the possibility of potential risks and associated complications. The present study details on the survey carried out to ascertain the current status of obtaining informed consent (IC) for explaining the epidural analgesia in labor.
Methods
The present study is based on a survey through a telephone questionnaire that covered all the hospitals in Korea where the anesthesiologists' belonged to and are registered with Korean Society of Anesthesiologists. The questionnaire included questions pertaining to administration of epidural analgesia to a parturient, information on different steps of obtaining an IC, whether patient status was evaluated, when the consent was obtained, and the reasons behind, if the consent had not being given.
Results
A total of 1,434 respondents took part in the survey, with a response rate of 97% (1,434/1,467). One hundred seventy-four hospitals had conducted epidural analgesia on the parturient. The overall rate of obtaining IC for epidural analgesia during labor was 85%, of which only 13% was conducted by anesthesiologists. The rate of evaluating preoperative patient status was 74%, of which 45% was conducted by anesthesiologists. Almost all of the consent was obtained prior to the procedure.
Law and enforcements governing health and medical practices are being revised and upgraded pertaining to different geographical locations. It is therefore necessary to investigate the influence of social standards that determine the formulation of legislative acts. Since medical treatment always contains an element of risk, it is essential to completely explain the process who is undergoing this treatment regimen or procedure. Ideally, all aspects -the benefits, side effects and risks of medical treatment should be explained prior to obtaining consent for the treatment. This explanation and consent is what is called "the obligation of explanation". The following precedent is found in the Korean Supreme Court: "when clinicians plan to perform surgery or a procedure that has a high risk of inducing a poor outcome, they must explain, to patients or their legal representative, the pertinent medical information-whatever is considered to be necessary in view of the current medical standards-including the clinical symptoms of a disease and the content/benefits/risks of a treatment." This is an obligation prior to establishing a treatment contract or as a prerequisite to obtaining consent for a surgery except in emergent patients or those in urgent need of medical attention. Clinicians are obliged to explain the benefits and risks of the planned medical treatment and allow the patient to choose a proper treatment [1], while the clinician would just aid in the decision making. However, the obligation of explanation is not yet imparted in the Korean laws. Statutes related to this obligation include Article 24 of the medical law (instruction of medical care), Article 5 of the bioethical right of self determination, Article 12 of the health medical basic law (right of self determination regarding health medical services) and Article 9 of the law of emergency medical care (explanation of emergency medical treatment). Since there are no laws that are directly enacted for the obligation of explanation, the importance of such an obligation is now discussed in order to clarify and provide an insight during the revision of the medical law in 2007, which unfortunately did not pass the legislation. As there are no regulations that explicitly require the obligation of explanation, therefore, its detailed process and the effect of obtaining consent are not found in the Korean laws.
Previous published studies in the Korean literature have indicated that explanation of and consent for anesthesia have not been found in many cases or have been included only partly in written or verbal consent for surgery [2,3]. Although previous studies in the English-language literature have demonstrated that anesthesiologists have reached a consensus of opinion in obtaining consent for anesthesia [4], there has been no completely acceptable description in the consenting procedure and appropriate method for obtaining consent.
Amongst the methods for analgesia in labor, epidural insertion is relatively effective and safe in parturients and their fetus, which is widely used in current clinical practice. Epidural analgesia is exclusively performed in the Department of Anesthesiology and Pain Medicine. The safety of both parturients and their fetus should be simultaneously considered, and a detailed explanation of the whole process of epidural analgesia and information about the likely complications must be provided. However, it is noted that in some hospitals, no consent is obtained or consent is obtained only after a simple description of the analgesia. Unlike consent for planned analgesia, it is unclear whether anesthesiologists can properly explain the epidural analgesia to parturients during labor and obtain consent for it [5-7].
Considering that, parturients in labor are similar to emergent patients and they may not correctly understand the explanation of epidural analgesia, it is necessary to determine how to explain the procedure in order to properly obtain consent for it. Although the obligation of explanation cannot be necessarily fulfilled only by obtaining consent, we attempted to evaluate the frequency of performing this obligation. In addition, although obtaining consent does not always represent the complete explanation, this study was conducted to utilize the obtaining of consent as an objective indicator for the performance of successful explanation.
As of 2009, anesthesiologists working in 1,467 nationwide hospitals were enrolled in the registry of the Korean Society of Anesthesiology. Telephonic interviews were performed on one or more anesthesiologists by using the questionnaire method. The interviews were conducted by a single investigator with the same questionnaire and in the same tone of voice for each interview. First, the interviewees were asked whether they had performed epidural analgesia. If yes, they were asked about the type and size of their hospitals; if no, they were asked for the reason why they did not perform the analgesia. In cases where they reported having performed epidural analgesia, they were asked whether they obtained consent for it. If yes, they were asked about their affiliation and the timing of obtaining consent; if no, they were asked about the reason why they did not obtain consent. Third, they were asked about their performance of preoperative evaluation of patient status. If yes, they were asked as to who performed the evaluation and about their affiliation. The data was expressed as percentage, and descriptive statistics were performed.
Of the 1,467 hospitals, 1,434 responded (response rate, 97%). Of the 1,434 hospitals, 174 had performed epidural analgesia. Of the 174 hospitals, 58 were university hospital (58/68, 85%), 33 belonged to a general hospital (34/253, 13%), and 83 were private hospitals (83/1,107, 8%). Hospitals where epidural analgesia was performed were classified as follows: 83 hospitals with ≤100 beds (47%), 35 hospitals with 101 ≤ beds <500 (20%), 46 hospitals with 501 ≤ beds ≤ 1,000 (26%), and 11 hospitals >1,000 beds (Table 1). The size of the hospitals where epidural analgesia was not performed were excluded from the study because the responses were not clear. The reasons enumerated for not performing epidural analgesia in these hospitals were: 1) the absence of the Department of Obstetrics; 2) no parturients to treat; and 3) no patients who wanted analgesia due to participation in pain clinic.
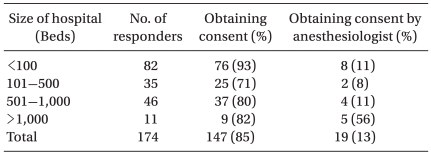
Consent for epidural analgesia was obtained by 147 hospitals (85%) and not obtained by 27 hospitals (15%). Of these 147 hospitals, consent was obtained at the Department of Anesthesiology in 19 hospitals (13%) and at the Department of Obstetrics in 128 hospitals (87%). According to hospital type, consent was obtained in 44 university hospitals (76%), 27 general hospitals (82%) and 76 private hospitals (92%) (Table 2). According to hospital size, consent was most commonly obtained in hospitals with <100 beds (76/82, 93%), and it was obtained most commonly at the Department of Anesthesiology in hospitals with >1,000 beds (5/9, 56%) (Table 3). Consent was obtained by labor room nurses or assistant nurses other than obstetricians in 22 of 128 hospitals where it was obtained at the Department of Obstetrics.
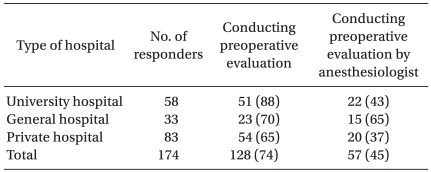
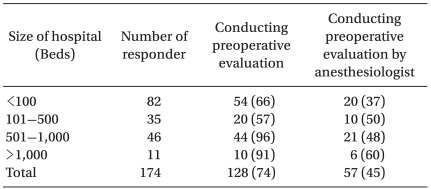
Preoperative evaluation of patient status including blood coagulation tests was performed in 128 (74%) of 174 hospitals. Of these 128 hospitals, this evaluation was performed at the Department of Anesthesiology and Pain Medicine in 57 hospitals (45%) (Table 4). This evaluation was most commonly performed in university hospitals (51/58, 88%) and at the Department of Anesthesiology and Pain Medicine in general hospitals (65%) (Table 4). It was most commonly performed in hospitals with >500 beds (54/57, 95%) and at the Department of Anethesiology and Pain Medicine in hospitals with >100 beds (37/74, 50%) (Table 5). As for the timing of obtaining consent, 28 hospitals obtained consent before epidural insertion, whereas 1 hospital obtained it after epidural insertion.
The top three reasons for not obtaining written consent were: 1) they had a small number of patients (main cause); 2) they had no well established protocol for obtaining consent; and 3) they thought that verbal consent was sufficient.
This study found that the rate of obtaining consent was 85%, suggesting that hospitals obtain consent as evidence to indicate that they undertake the obligation of explanation. However, only 13% of the consenting procedures were conducted by clinicians at the Department of Anesthesiology and Pain Medicine. This means that surgeons usually explain the benefits, side effects and risks of anesthesia while they are obtaining the consent for surgery [2]. The following case is a precedent of the Korean Supreme Court regarding medical professionals in charge of explanation: medical professionals who are obliged to explain the treatment procedure should be principally clinicians in charge but can be those not in charge under special conditions [8]. Based on this precedent, medical professionals who perform the consent process for anesthesia or epidural insertion can be clinicians who are not in charge. A previous study reported that 25% of anesthesiologists think that consent can be obtained by surgeons, which may be attributed to a low rate of obtaining consent by anesthesiologists [2]. In our study, it was found that only 13% of anesthesiologists explained epidural insertion (Table 2 and 3). Since the consent process was performed by labor room nurses or assistant nurses in some hospitals, it should be determined whether they can be included in the category of clinicians not in charge as indicated in the aforementioned precedent if they are allowed to undertake this procedure then they should be sufficiently trained. In addition, when considering the following precedent that provided the obligation of explanation of side effects with low incidences, it should be determined whether obstetricians can sufficiently provide information about the likely complications and side effects of epidural insertion: clinicians cannot be released from the obligation of explanation on the basis that complications and sequelae occur occasionally, and in cases where sequelae and complications typically occur or are irreversible and serious, they should explain them to patients despite rare occurrence [9].
In this study, it was found that the rate of obtaining consent was highest in private hospitals with ≤100 beds. The reason for this may be explained by the fact that obstetricians explain the procedure for epidural analgesia as well as the labor process following which they obtain consent. This result is consistent with a high rate of obtaining consent in university hospitals with ≥1,000 beds. In other words, since in university hospitals, work assignment between anesthesiologists and obstetricians is relatively clear, the rate of obtaining consent will be decreased if the consent is not obtained by anesthesiologists.
In this study, preoperative evaluation of patient status was performed in 74% of hospitals, and it was conducted by anesthesiologists in only 45% of hospitals where epidural analgesia was performed. It is estimated that since clinical pathology equipment is required for the preoperative evaluation such as blood coagulation tests, preoperative evaluation might more frequently be conducted in such hospitals. Likewise, in this study, it was shown that the preoperative evaluation was more commonly conducted in university hospitals and in those with >100 beds. Although the exact reason was not clearly elucidated, it is postulated that most of the consenting procedures were performed by obstetricians, whereas preoperative evaluation was mainly performed by anesthesiologists. Furthermore, since medical dispute currently tends to increase and preoperative evaluation aids in the determination of the exact causes of complications such as femoral neuropathy that can be induced by either labor or epidural insertion, the preoperative evaluation by anesthesiologists is mandatory [10].
In this study, only 29 anesthesiologists reported the timing of obtaining consent. This implies that most anesthesiologists did not know its exact timing because most of the consenting procedures for epidural insertion were performed by obstetricians.
Based on the result that most respondents (28/29, 97%) obtained consent before the procedure, there is a consensus of opinion between obstetricians and anesthesiologists that consent should be obtained before the procedure. Although there was only 1 hospital that reported it to occur, obtaining consent after the procedure may be an actual situation because most parturients complain of severe labor pain. In cases where labor progresses rapidly or parturients report an abrupt onset of labor pain, it is controversial whether consent can be appropriately obtained [5-7]. When considering the judgment of the court that clinicians can be released from the obligation of explanation to emergent patients or those under special conditions, it is reasonable to assume that consenting procedure can be performed after labor in parturients with an abrupt onset of labor pain [1]. In addition, much debate and research are needed to reach a complete agreement concerning the definition of emergent situations and proper methods for explaining the procedure under urgent situations [11]. Thus, it's important to discuss the proper level of consent for epidural insertion that parturients want. It is conceivable that severe labor pain may affect the ability to understand the explanation of the procedure and risks of epidural insertion and that the parturients do not want to be informed of extremely rare complications such as death from permanent nerve damage and the side effects of the procedure [5,12]. However, in the English-language literature, it has been reported that most partrients want to be informed of the complete procedure and life-threatening complications [13]. It has been demonstrated that parturients are more capable of recalling information during labor by using written consent than by using verbal consent, regardless of the degree of pain, the educational level of parturients and a combined use of other analgestics during the procedure [14]. In addition, based on the precedent of the Korean Supreme Court that clinicians cannot be released from the obligation of explanation because the complications or sequelae are extremely rare, and in cases where these complications and sequelae typically occur after the procedure, the level of explanation should be determined [9].
Of hospitals that did not obtain consent, those which reported that verbal consent was sufficient appeared to understand medical laws and the decision criteria of the court to some extent. However, it is desirable to obtain a more objective consent by using a written form. In hospitals reporting a small number of parturients or insufficient establishment of the protocol, the current decision criteria of the court and efficacy of the procedure in their hospitals should be considered.
Taken together, written consent for epidural insertion was obtained in 85% of hospitals, mostly by obstetricians (87%), and 22 (12%) of the hospitals obtained consent by labor room nurses or assistant nurses. Preoperative evaluation of patient status was performed in 74% of hospitals. Consent was mainly obtained before the procedure (only 1 hospital obtained consent after the procedure). Although the obligation of explanation is not yet legislated, it is likely that explanation of and consent for the procedure are being performed at a relatively high level in the current situation where the decision of the court and general recognition are needed during medical treatment. Further studies on consent by a legal representative, consent after the procedure, explanation of the procedure by nurses/assistant nurses, the content of explanation and consent process are needed to guarantee the selection right of parturients and to improve the efficacy of the procedure.
Acknowledgements
We really appreciate all the responders and Suji Yang who had sincerely surveyed all the questionnaire with telephone.
Notes
References
1. The content of clinicians' obligation of explanation and compensation cases due to its violation. Supreme Court of South Korea (95da49608). Delivered on July 22, 1997.
2. Sim JY, Kim D, Lee JR, Ahn W. Survey of the informed consent for the anesthesia practice in Korea. Korean J Anesthesiol. 2005; 48:117–123.

3. Koo GH, Jung YH. Examination to anesthetic informed consent. Korean J Anesthesiol. 2007; 52:179–186.

4. White SM, Baldwin TJ. Consent for anaesthesia. Anaesthesia. 2003; 58:760–774. PMID: 12859468.
5. Pattee C, Ballantyne M, Milne B. Epidural analgesia for labour and delivery: informed consent issues. Can J Anaesth. 1997; 44:918–923. PMID: 9305553.

6. Paech M. "Just put it!" in Consent for epidural analgesia in labour. Anaesth Intensive Care. 2006; 34:147–149. PMID: 16617634.

7. Rosen M. "Just put it!" in Consent for epidural analgesia in labour. Anaesth Intensive Care. 2006; 34:519–520. PMID: 16917999.

8. Supreme Court of South Korea (99da10479). The content of clinicians' obligation of explanation and the legality of explanation by clinicians who are in charge of the corresponding surgery but not in charge of treatment. Delivered on September 3, 1999.
9. The legality of releasing clinicians from the obligation of explanation in cases that have a low possibility of the risks for sequelae/side effects. Supreme Court of South Korea (94da3421). Delivered on January 20, 1995.
10. Choi SP, Oh BM, Ahn W. Bilateral femoral neuropathy after vaginal delivery: a case report. Korean J Anesthesiol. 2009; 57:228–232.
11. Yun SY. A survey on the concepts of informed consent among emergency physician [Master degree thesis]. 2004. Seoul: Yonsei University.
12. Smedstad KG, Beilby W. Informed consent for epidural analgesia in labour. Can J Anaesth. 2000; 47:1055–1059. PMID: 11097533.

13. Jackson A, Henry R, Avery N, VanDenKerkhof E, Milne B. Informed consent for labour epidurals: what labouring women want to know. Can J Anaesth. 2000; 47:1068–1073. PMID: 11097535.

14. Middle JV, Wee MY. Informed consent for epidural analgesia in labour: a survey of UK practice. Anaesthesia. 2009; 64:161–164. PMID: 19143694.

Table 1
Demographic Data of Respondents
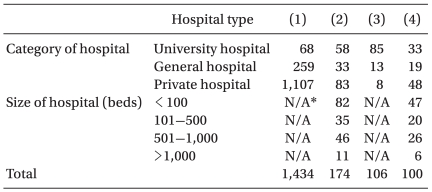
Values are the number of respondents. (1) Surveyed hospitals, (2) Hospitals which provide epidural analgesia for parturients, (3) Percentage of epidural analgesia-providing hospitals relative to the surveyed hospitals in each Categories, (4) Percentage of each hospital type relative to the 174 epidural analgesia-providing hospitals. *N/A: not available.
Table 2
The Rate of Obtaining Informed Consent for Epidural Analgesia in Labor According to Hospital Type
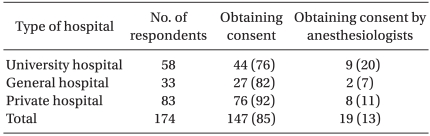
Table 3
The Rate of Obtaining Informed Consent for Epidural Analgesia in Labor According to Hospital Size




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download