Abstract
Background
Respiratory dynamics may be monitored and evaluated indirectly by measuring the peak inspiratory pressure and plateau pressure. In this study, the respiratory dynamics of patients undergoing spinal surgery using a Jackson surgical table were observed with a device after converting their position from supine to prone. The effects of the dynamic compliance and airway resistance were observed from the changes in peak inspiratory pressure and plateau.
Methods
Twenty five patients were selected as subjects scheduled to undergo lumbar spine surgery. After intubation, the patients were ventilated mechanically with a tidal volume of 10 ml/kg and a respiration rate of 10/min. Anesthesia was maintained with sevoflurane 1.5%, nitrous oxide 2 L/min and oxygen 2 L/min. The peak inspiratory pressure, plateau pressure, resistance, compliance, arterial oxygen tension, carbon dioxide tension, heart rate and arterial blood pressure were measured at 10 minutes after the induction of anesthesia. These parameters were measured again 10 minutes after placing the patient in the prone position.
With the recent developments in surgical maneuvers and the increase in demand for noninvasive treatments, there have been an growing number of procedures that involve changes in body positioning and laparatomy. Patients under general anesthesia who undergo the above may experience biological changes due to the effects of these positional changes on the cardiovascular and respiratory system. Therefore, patients who undergo changes in body positioning require monitoring of the cardiovascular and respiratory systems. In controlled ventilation using modern anesthetic monitoring devices, the peak inspiratory pressure (PIP) and plateau pressure (Pplat) can be measured by a monitor, and the respiratory dynamics can be monitored and evaluated indirectly. When the amount of gas that expands the lungs is constant, the increase in PIP is considered to be the state when the airway resistance (Raw) increases, when pulmonary compliance decreases, or when both occur simultaneously [1].
In general anesthesia using muscle relaxants, moving the patient from the supine to prone position while using a mechanical ventilator for controlled ventilation affects the patient's respiratory dynamics and vital signs. Owing to the pressure on the abdomen, the internal organs push the diaphragm towards the direction of the head. In addition, the weight of the trunk decreases the diameter of the chest. With such movement limitations, the respiratory compliance decreases by 20-30% and the PIP increases. Therefore, the increase in PIP in the prone position has been attributed to the decrease in respiratory compliance [2-4].
On the other hand, some studies employed surgical tables with abdomen rolls to allow for the free movement of the abdomen. Therefore, the prone position rather than the supine position has been reported to improve the respiratory dynamic changes. Pelosi et al. [5] reported that the prone position during general anesthesia improves the lung volume and oxygenation without significantly altering the respiratory, pulmonary, or chest wall compliance. In addition, Palmon et al. [6] stated that the prone position using a Jackson surgical table does not significantly change the PIP or pulmonary compliance in patients with a normal weight. The use of a Jackson surgical table rather than a Wilson surgical table or a chest roll causes the least change in PIP and pulmonary compliance in patients with both normal and abnormal weights.
In this study, the increase in PIP was monitored using a patient monitoring device when changes in body positioning to the prone position were made using a Jackson surgical table. The authors also made the assumption that the change in PIP affects the pulmonary compliance and Raw. Patients scheduled to undergo spinal surgery using a Jackson surgical table were moved from the supine to the prone position to observe the effects of the PIP and Pplat on the dynamic compliance (Cdyn) and Raw using a respiratory dynamics monitoring device.
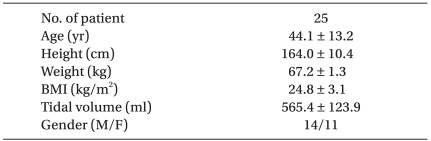
After gaining the approval of the ethics committee, the study was performed on 25 American Society of Anesthesiologists' physical status class I & II male and female adult patients, aged 20-65 years, who were scheduled to undergo surgery under general anesthesia for lumbar disc herniation or spinal stenosis. They agreed to participate after having being explained the study and after they had asked questions. Patients were excluded if they had a history of abnormalities in the cardiovascular system or respiratory system, or if they had spinal disorders that had caused changes to the respiratory system, such as scoliosis, lordosis, kyphosis and ankylosing spondylitis. There were 25 patients with a mean age and body mass index of 44.1 ± 13.2 years and 24.8 ± 3.1 kg/m2, respectively (Table 1).
All patients were fasted from midnight before surgery. On the day of surgery, midazolam 2 mg and glycopyrrolate 0.2 mg were administered IM, and famotidine 20 mg was administered IV 30 minutes before arriving into the OR. On the operating table a patient monitoring device (24c Omnicare®, Hewlett Packard, Houston, TX, USA) was used for continuous monitoring of the electrocardiography, heart rate and oxygen saturation. In all patients, proper mask ventilation was confirmed if the patient lost consciousness after the IV administration of propofol when anesthesia was induced. Rocuronium 0.8 mg/kg was administered IV for adequate muscle relaxation. Muscle relaxation was confirmed 2 minutes after administering rocuronium IV. Intubation was then performed using a wire-reinforced tube, 8.0 mm in diameter for males and 7.5 mm in diameter for females. After confirming by auscultation that the breath sounds of both lungs were the same, the intubation tube was fixed at the depth of 23-24 cm for males and 21-22 cm for females. Before starting the procedure, anesthesia was maintained by O2 2 L/min, N2O 2 L/min, and sevoflurane 1.5 vol%. Mechanical ventilation was set at a constant pace of a tidal volume 10 ml/kg and a respiration rate of 10 bpm. In the radial artery, a 20 gauge arterial catheter was placed to allow continuous measurements of the arterial blood pressure and for arterial blood sampling. After the required 10 minutes after endotracheal intubation to allow the vital signs to stabilize and for the changes in pulmonary compliance and pulmonary resistance to return to the state before airway irritation [7], a respiratory dynamics monitoring device (Ventcheck®, Novametrix Medical System, Wallingford, CT, USA) was connected to the end of the endotracheal tube to measure the PIP, Pplat, Raw, and Cdyn. All values were measured 3 times, and the median value was used for further analysis. The arterial PaO2 and PaCO2 were measured by arterial analysis, and the blood pressure and heart rate were monitored. All patients used a Jackson surgical table for the prone position. This was done using the method proposed by Smith [8], which involved supporting the upper chest and abdomen by a roll and allowing for free movement of the abdomen. The head was kept in the neutral position by placing it on a horse-shoe shaped head rest. After confirming that the fixed position of the tubes of the patient in the prone position did not change, the breath sounds of both lungs were confirmed by auscultation to be the same. After the patient was stabilized for 10 minutes, the respiratory dynamics were measured using the same methods as in the supine position and compared. All measurements are reported as the mean ± SD. Data analysis was performed by SPSS (version 12.0, SPSS inc., Chicago, IL, USA) using a paired t-test. A P value < 0.05 was considered significant.
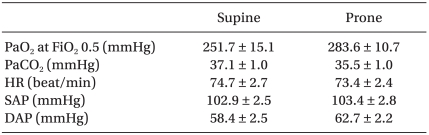
When changing the body positioning of the patient from the supine position to the prone position, the mean arterial PaO2 increased from 251.7 ± 15.1 mmHg to 283.6 ± 10.7 mmHg. The mean PaCO2 decreased from 37.1 ± 1.0 mmHg to 35.5 ± 1.0 mmHg. However, the differences in both parameters were not statistically significant. There were no significant changes in the systolic and diastolic blood pressure or the heart rate (Table 2).
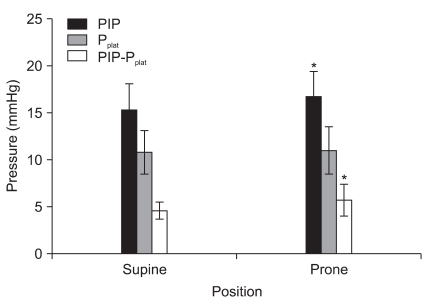
The PIP significantly increased (15.3 ± 2.8 mmHg vs. 16.7 ± 2.7 mmHg, P < 0.05) but there were no significant changes in the Pplat (10.8 ± 2.3 mmHg vs. 11 ± 2.5 mmHg, P > 0.05). In addition, the difference between the PIP and Pplat increased significantly (4.6 ± 0.9 mmHg vs. 5.7 ± 1.7 mmHg, P < 0.05, Fig. 1).
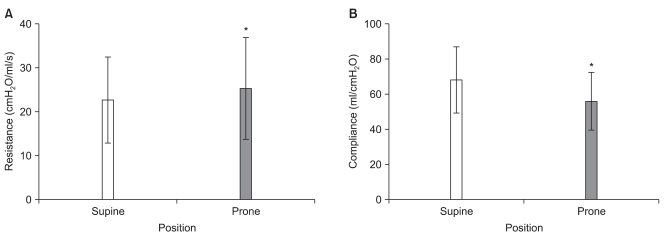
Raw increased significantly when the body positioning was changed in a similar manner as the difference between the PIP and Pplat increased significantly (22.7 ± 9.8 cmH2O/ml/s vs. 25.3 ± 11.6 cmH2O/ml/s, P < 0.05). However, Cdyn significantly decreased (68.2 ± 18.8 ml/cmH2O vs. 56.2 ± 16.5 ml/cmH2O, P < 0.05, Fig. 2).
These results revealed an increase in PIP but not in the Pplat. The Pplat was measured at the state when the gas flow was blocked. The difference between the PIP and Pplat is the pressure needed to overcome Raw. Therefore a constant Pplat with an increase in PIP indicates an increase in Raw [9]. These results revealed a decrease in Cdyn. Cdyn is affected by the inspiratory gas flow, Raw and the equilibrium between the proximal tip and distal end of the airway [10]. A decrease in Cdyn occurs in cases of an increase in Raw or a decrease in pulmonary and thoracic elasticity [11]. Therefore, the increase in PIP was attributed to the increase in Raw or decrease in Cdyn.
According to previous studies on the prone position, abdominal movement is limited when the abdomen is pressed and the internal organs push the diaphragm in the direction of the head [2-4]. Moreover, the weight of the trunk reduces the diameter of the chest wall and limits movement, which reduces the respiratory compliance by 20-30%. Therefore, the increase in PIP is believed to be due to a decrease in pulmonary compliance. In contrast, if the patient is positioned where the upper chest and pelvis are supported allowing for the free movement of the abdomen, as Smith [8] suggested, it would produce less restriction of the chest wall than other body positioning apparatuses. Moreover, Cho et al. [12] stated that there are no significant changes in respiratory or pulmonary compliance as the patient's position was changed from the supine to the prone position. This is because compared to other body positioning apparatuses, the Jackson table does not press the upper abdomen but allows free movement of the abdomen, and has the least effect on the respiratory system. In this study, the patients were moved to the prone position using a Jackson table, so the cause for the increase in PIP does not appear to be due to the effects of a decrease in pulmonary compliance but from an increase in Raw.
A variety of reasons can lead to an increase in Raw. The increase in Raw may be due to a problem with the endotracheal tube, such as kinking of the tube or overexpansion of the air-cuff, or it may be due to an obstruction of the airway by secretions, blood and other objects [13]. The increase in Raw after placing the patient in the prone position was attributed primarily to airway secretion. In such cases, the cause for the increase in Raw is likely to be an endotracheal tube obstruction, airway obstruction due to mucus, or bronchospasm, which can be improved if the secretion is removed. There are reported cases where patients in the prone position repeatedly had obstructed endotracheal tubes due to a secretion in the lung or blood drainage due to the force of gravity [14-16]. Baydur et al. [17] also stated that the increase in respiratory and pulmonary resistance occurs from the accumulation of airway secretion with time. This study is limited in that it made observations after only a short period of 10 minutes after the changing the body position. To confirm the cause, measurements of the Raw should be carried out after a longer time has passed since taking up the prone position.
The other cause can be considered to be a decrease in the chest wall elasticity. Pelosi et al. [5] stated that moving the patient into the prone position compared to the supine position increases the respiratory resistance by 20%. This 20% increase in respiratory resistance is believed to be due to a decrease in thoracic elasticity because the tidal volume is maintained at a constant rate. In addition, Cho et al. [12] explained that the increase in chest wall compliance occurs when the apparatus used to support the upper chest in the body positioning changes presses the upper chest, which can explain the increase in Raw.
Considering the increase in Raw due to kinking of the endotracheal tube, most procedures with the patient in the prone position use a wire-reinforced tube to minimize kinking. Kil and Bishop [18] reported that kinking of the endotracheal tube leads to turbulent flow, which increases the airway pressure and resistance. The wall of a wire-reinforced tube is rough compared to a polyvinyl chloride tube and creates friction with air particles, which causes turbulent flow and increases the resistance. In the prone position, a wire-reinforced tube is used to prevent kinking of the endotracheal tube but the neutral position of the head causes the endotracheal tube to curve instead of straighten. This also may cause an increase in Raw.
The total respiratory resistance is proportional to PIP - Pplat and inversely proportional to the inspiratory flow rate [19]. In this study, the inspiratory flow rate was kept at a constant rate. Hence, an increase in Raw increased the difference between the PIP and Pplat. In addition, Cdyn can be found by dividing the tidal volume by PIP. Thus, the increase in Cdyn can be explained as an increase in Raw.
Backofen and Schauble [20] and Yokoyama et al. [21] reported that changing the patient to the prone position decreases the cardiac index (24.4% and 17.2%) and increases the total systemic vascular resistance. The decrease in cardiac index is due to a decrease in venous circulation from venostasis in the leg and an increase in thoracic pressure. However, the change in blood pressure is not commonly the result of an increase in total systemic vascular resistance due to activation of the sympathetic nervous system following a decrease in cardiac output [22]. These results also showed no significant changes in blood pressure or heart rate in either the supine or prone position.
The prone position for patients with acute respiratory failure is well-known for improving hypoxia and aiding in the correction of V/Q mismatching [23]. On the other hand, only a few studies have examined the changes in oxygenation and V/Q matching under general anesthesia. Lumb and Nunn [24] reported that the prone position for normal, conscious patients increases their functional residual capacity. Pelosi et al. [5] stated that changing to the prone position under general anesthesia increases the functional residual capacity and PaO2. Previously, pulmonary blood flow was more in the dependent area than in the independent area [25]. However, magnetic resonance imaging measurements in recent animal studies showed that the pulmonary blood flow moves towards an independent area of the back regardless of the change to the prone position [26,27]. This was explained as being due to the structurally low pulmonary vascular resistance of the lung's side towards the back rather than the effects of gravity on pulmonary blood flow. In the prone position, the structural characteristics of the airway and pulmonary vein, rather than the effects of ventilation or gravity, allows for better ventilation in the back area. When changing from the supine to prone position, such an increase in lung volume and improvement in the V/Q matching are known to improve oxygenation [4]. In the present study, PaO2 and PaCO2 differed from the mean values but the changes were not significant. The values were taken 10 minutes after changing to the prone position but these values should have been taken after a longer time had passed.
In conclusion, when changing the patient from the supine to prone position, the PIP can increase even when pressure on the abdomen is minimized using a Jackson surgical table. This is not only because of the decrease in pulmonary and chest wall compliance but also from the effects of the increase in Raw. Therefore, the increase in PIP on patient monitoring should not be attributed only to a decrease in compliance caused by the prone position, but also to an increase in Raw caused by the drainage of secretive fluids due to gravity from the change in body position, as well as to the location and kinking of the endotracheal tube.
References
1. Kim BS. Anesthesia and pain management. 2009. 2nd ed. Seoul: Elservier Korea;p. 929–973.
2. Warner MA. Barash PG, Cullen BF, Stoelting RK, editors. Patient positioning. Clinical Anesthesia. 2006. 5th ed. Philadelphia: Lippincott-Raven Publishers;p. 657–661.
3. Lynch S, Brand L, Levy A. Changes in lung thorax compliance during orthopedic surgery. Anesthesiology. 1959; 20:278–282. PMID: 13650210.

4. Manna EM, Ibraheim OA, Samarkandi AH, Alotaibi WM, Elwatidy SM. The effect of prone position on respiratory mechanics during spinal surgery. Middle East J Anesthesiol. 2005; 18:623–630. PMID: 16381267.
5. Pelosi P, Croci M, Calappi E, Cerisara M, Mulazzi D, Vicardi P, et al. The prone positioning during general anesthesia minimally affects respiratory mechanics while improving functional residual capacity and increasing oxygen tension. Anesth Analg. 1995; 80:955–960. PMID: 7726438.

6. Palmon SC, Kirsch JR, Depper JA, Toung TJ. The effect of the prone position on pulmonary mechanics is frame-dependent. Anesth Analg. 1998; 87:1175–1180. PMID: 9806704.

7. Dohi S, Gold MI. Pulmonary mechanics during general anaesthesia. The influence of mechanical irritation on the airway. Br J Anaesth. 1979; 51:205–214. PMID: 435343.
8. Smith RH. One solution to the problem of the prone position for surgical procedures. Anesth Analg. 1974; 53:221–224. PMID: 4856130.

9. Bigatello LM, Davignon KR, Stelfox HT. Respiratory mechanics and ventilator waveforms in the patient with acute lung injury. Respir Care. 2005; 50:235–245. PMID: 15691393.
10. Lu Q, Vieira SR, Richecoeur J, Puybasset L, Kalfon P, Coriat P, et al. A simple automated method for measuring pressure-volume curves during mechanical ventilation. Am J Respir Crit Care Med. 1999; 159:275–282. PMID: 9872850.

11. Kárason S, Søndergaard S, Lundin S, Wiklund J, Stenqvist O. A new method for non-invasive, manoeuvre-free determination of "static" pressure-volume curves during dynamic/therapeutic mechanical ventilation. Acta Anaesthesiol Scand. 2000; 44:578–585. PMID: 10786746.

12. Cho SY, Noh GJ, Yeom JH, Shin WJ, Kim YC, Kim KH, et al. The effect of prone position on pulmonary compliances by anesthesia duration. Korean J Anesthesiol. 2000; 38:997–1001.

13. Szekely SM, Webb RK, Williamson JA, Russell WJ. The Australian Incident Monitoring Study. Problems related to the endotracheal tube: an analysis of 2000 incident reports. Anaesth Intensive Care. 1993; 21:611–616. PMID: 8273884.
14. Grimmett WG, Poh J. Clearance of an obstructed endotracheal tube with an arterial embolectomy catheter with the patient in the prone position. Anaesth Intensive Care. 1998; 26:579–581. PMID: 9807616.

15. Lin JA, Wong CS, Cherng CH. Unexpected blood clot-induced acute airway obstruction in a patient with inactive pulmonary tuberculosis during lumbar spine surgery in the prone position: a case report. Acta Anaesthesiol Taiwan. 2005; 43:93–97. PMID: 16060404.
16. Son JS, Kim JH, Lim HS, Ko SH. Acute obstruction of an endotracheal tube due to large mucous plug: removed using flexible fiberoptic bronchoscopy: a case report. Korean J Anesthesiol. 2005; 49:694–697.

17. Baydur A, Sassoon CS, Stiles CM. Partitioning of respiratory mechanics in young adults: effects of duration of anesthesia. Am Rev Respir Dis. 1987; 135:165–172. PMID: 3800144.
18. Kil HK, Bishop MJ. Head position and oral vs nasal route as factors determining endotracheal tube resistance. Chest. 1994; 105:1794–1797. PMID: 8205879.
19. Tobin MJ. Principles and practice of mechanical ventilation. 2006. 2nd ed. New York: McgRaw-Hill;p. 976–984.
20. Backofen JE, Schauble JF. Hemodynamic changes with prone position during general anesthesia. Anesth Analg. 1985; 64:194.
21. Yokoyama M, Ueda W, Hirakawa M, Yamamoto H. Hemodynamic effect of the prone position during anesthesia. Acta Anaesthesiol Scand. 1991; 35:741–744. PMID: 1763593.

22. Wadsworth R, Anderton JM, Vohra A. The effect of four different surgical prone positions on cardiovascular parameters in healthy volunteers. Anaesthesia. 1996; 51:819–822. PMID: 8882241.

23. Pelosi P, Brazzi L, Gattinoni L. Prone position in acute respiratory distress syndrome. Eur Respir J. 2002; 20:1017–1028. PMID: 12412699.

24. Lumb AB, Nunn JF. Respiratory function and ribcage contribution to ventilation in body positions commonly used during anesthesia. Anesth Analg. 1991; 73:422–426. PMID: 1897767.

25. Kaneko K, Milic-Emili J, Dolovich MB, Dawson A, Bates DV. Regional distribution of ventilation and perfusion as a function of body position. J Appl Physiol. 1966; 21:767–777. PMID: 5912746.

26. Glenny RW, Lamm WJ, Albert RK, Robertson HT. Gravity is a minor determinant of pulmonary blood flow distribution. J Appl Physiol. 1991; 71:620–629. PMID: 1938736.

27. Prisk GK, Yamada K, Henderson AC, Arai TJ, Levin DL, Buxton RB, et al. Pulmonary perfusion in the prone and supine postures in the normal human lung. J Appl Physiol. 2007; 103:883–894. PMID: 17569767.

Fig. 1
Change in peak inspiratory pressure (PIP), plateau airway pressure (Pplat) and PIP - Pplat when moving from the supine to prone position. *P < 0.05 versus the supine position.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download