Abstract
Background
A decreased lumbosacral subarachnoidal space volume is a major factor in the cephalad intrathecal spread of local anesthetics in term parturients and their subarachnoidal space is decreased due to the compressive effect of huge uteri. Therefore, they show a higher level of sensory block and hypotensive episodes. The purpose of this study is to investigate whether the symphysis-fundal height (SFH) correlates with the highest sensory level and the amount of ephedrine administered under spinal anesthesia.
Methods
Fifty-two uncomplicated parturients who consented to spinal anesthesia for elective cesarean section were studied. The SFH of all parturients had been measured just before the spinal anesthesia administered by one person. Hyperbaric bupivacaine with fentanyl 20 µg, was administered for spinal anesthesia. The amount of 0.5% bupivacaine was adjusted according to the patient's height and weight. The level of sensory block and the amounts of ephedrine to treat hypotension, nausea and vomiting were assessed. Linear regression and correlation analysis were applied to analyze the data.
Spinal anesthesia is one of the most preferred anesthetic methods during Cesarean section since it provides easy and rapid induction, effective sensory and motor block and has little effect on the fetus [1]. However, in a parturient woman, the lumbosacral subarachnoidal space volume is decreased as the inferior vena cava is pressed by the hypertrophic uterus and plexus venosus collateral circulation is developed in the epidural space. Because of this, the amount of cerebrospinal fluid is decreased in the lumbosacral area and the small dose of administrated local anesthetic moves mainly to the cranial cavity; consequently, the incidents of high spinal anesthesia and hypotension increase [2,3]. In order to reduce the risk of high spinal anesthesia, studies have been conducted regarding factors that affect the level of anesthesia, such as height, weight and body mass index (BMI), but the roles of these factors are controversial. Norris [4] reported that height, weight and BMI are not related to the level of spinal anesthesia during Cesarean section. However, in a recent study, Harten et al. [5] reported that when the local anesthetic dose is administrated considering the height and weight of parturient women, hypotension incidents are reduced compared to the cases reported using a fixed dose. However, we have observed that a considerable number of incidents of hypotension, nausea and vomiting were found, even in the cases where the local anesthetic dose was administrated under consideration of the height and weight of the parturient women who were supposed to undergo Cesarean section. In this study, therefore, we investigated whether the symphysis-fundal height (SFH) is related to the sensory block level, the ephedrine dose according to incidence of hypotension, nausea, and vomiting.
The study subjects were 52 parturient women whose American Society of Anesthesiologist physical status class was Class 1 or Class 2, among patients in the 38th to 42nd week of pregnancy who were supposed to undergo Cesarean section. The pregnant women who had contraindication for spinal anesthesia, e.g., those who displayed gestational hypertension, placenta previa, twin pregnancy, uterine myoma, oligohydramnios or hydramnion; those whose weight was less than 50 kg or more than 100 kg; those whose height was less than 140 cm or more than 180 cm; and those who were converted to general anesthesia due to insufficient spinal anesthesia, were excluded from the study. All the study patients were given an explanation about the purpose of the study prior to anesthesia, and they consented to the study. The study was permitted by the Institutional Review Board of the hospital.
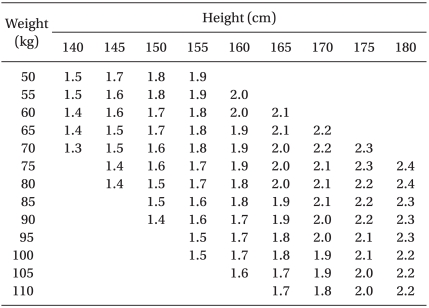
For all the parturient women, an automated noninvasive blood pressure device was installed on the right arm and a pulse oximetry and electrocardiograph were installed on the left arm prior to spinal anesthesia, in order to record blood pressure and heart rate. The initially measured blood pressure and heart rate were defined as the resting blood pressure and resting heart rate. During the intravenous injection of Hartmann crystalloid solution (15 ml/kg), the SFH was measured by a single person who palpated the edge of the uterine fundus from the superior edge of the pubic symphysis of the pregnant women, who were in the spine position on a table that was adjusted to be horizontal (Fig. 1). The height was not revealed to the anesthetist. Following 20 minutes of intravenous injection of the Hartmann crystalloid solution, the parturient women were converted to the right lateral recumbent position. Dural puncture was performed with a 26 G Quincke needle in a midline approach after disinfecting the puncture area between the L3-L4 lumbar vertebrae. After checking the cerebrospinal fluid outflow, the drug was injected at the rate of 0.1 ml/sec without changing the direction of the bevel. Regarding the dose of the drug, fentanyl 20 µg was mixed with the hyperbaric 0.5% bupivacaine (Bupivacaine HCl®, Myungmoon Pharmaceuticals, Korea) dose (Table 1) that was determined by considering the height and weight of the patients, as suggested by Harten et al. [5], and the mixture was injected. Immediately after injecting the drug, the patients took the spine position and the uterus was transposed to the left by tilting the table by 15° to the left, in order to prevent supine hypotensive syndrome. For the sensory nerve block, a cold feeling examination was performed with an alcohol swab every one minute, from the umbilicus and epigastric region to the center of the neck along the midline of the parturient women, until the height did not change any more; this was done to determine the maximum sensory blockade level. After completing the drug injection through the subarachnoid space, the blood pressure was measured every 2 minutes. When the systolic blood pressure dropped below 100 mmHg, or decreased by more than 20% of the resting blood pressure, or when the parturient women complained of nausea and vomiting, ephedrine (Ephedrine HCl®, Daewon Pharmaceuticals, Korea) (4 mg) was intravenously injected. When the blood pressure drop continued after the blood pressure measurement in 2-minute intervals, the same dose was repeatedly injected. Oxygen was supplied at the rate of 5 l/min through the face mask to all the parturient women. The operation was initiated after adjusting the table to be horizontal when the maximum sensory blockade level of the spinal anesthesia was T6 or higher and the blood pressure and heart rate of the parturient women became stable. Intravenous injection of fentanyl (80 µg) was carried out when the patients complained of visceral pain during the operation or the spinal anesthesia was converted to general anesthesia when the injection was considered inappropriate. The weight of the newborn baby was recorded after the delivery. The side effects such as hypotension, nausea and vomiting, respiratory depression or pruritus were observed and recorded.
All the measurements were presented as "mean ± standard deviation" and the SAS® Enterprise Guide fourth edition was used. Correlation analysis was performed to find the correlations among the SFH, ephedrine dose, and the maximum sensory blockade level.
The correlation between the SFH and the administrated ephedrine dose and the correlation between the weight of the fetus and the administrated ephedrine dose were also investigated. The regression equations (y = ax + b) were obtained for the SFH, the administrated ephedrine dose, and the weight of the fetus, respectively, by using the linear regression method, and the coefficients of determination (r2) were compared.
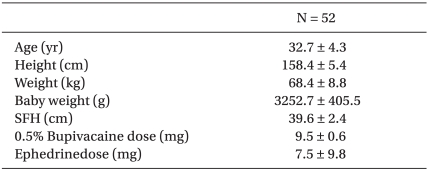
The subjects for this study were 52 parturient women within the age range of 32.7 ± 4.3, the weight of 68.4 ± 8.8 kg, and the height of 158.4 ± 5.4 cm. The weight of the fetuses was 3252.7 ± 405.5 g; the SFH of the parturient women was 39.6 ± 2.4 cm; the hyperbaric 0.5% bupivacaine dose that was injected during the spinal anesthesia was 9.5 ± 0.6 mg; and the ephedrine dose administrated after the spinal anesthesia was 7.5 ± 9.8 mg (Table 2).
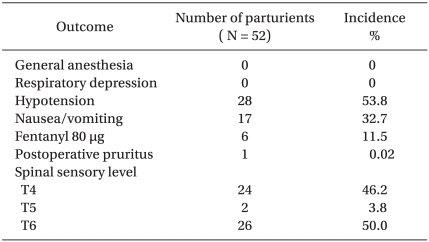
The maximum sensory blockade level of the spinal anesthesia was T4 for 24 patients, T5 for 2 patients, and T6 for 26 patients. None of the parturient women in the supine position showed supine hypotensive syndrome before the spinal anesthesia for Cesarean section and there was no case which required converting to general anesthesia due to inappropriate spinal anesthesia. Ephedrine was injected to treat the hypotension, nausea and vomiting after the spinal anesthesia in 28 of the 52 cases (53.8%), and of the 28 cases, nausea and vomiting accompanied 17 of them. In 6 out of the 52 cases (11.5%), fentanyl was additionally administrated for visceral pain. None of the parturient women complained of respiratory depression after the spinal anesthesia or of nausea and vomiting in the postoperative recovery room. However, pruritus occurred in 1 out of the 52 parturient women (0.02%) (Table 3).
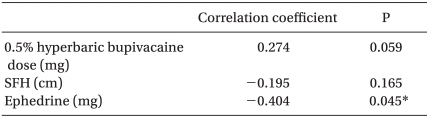
The correlation analysis result showed that the correlation coefficient between the maximum sensory blockade level and the SFH was - 0.195 and the significance test of the correlation coefficient showed that the P value was 0.165, which means the correlation was not significant. However, as the maximum sensory blockade level increased, the administrated ephedrine dose increased and showed significance (P value 0.045) (Table 4).
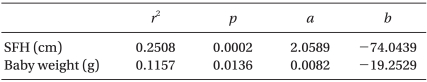
A significant correlation was found between the ephedrine dose and the SFH when hypotension, nausea and vomiting occurred after the spinal anesthesia (Fig. 2). In addition, a significant correlation was found between the administrated ephedrine dose and the weight of the fetus (Fig. 3). The SFH was more strongly correlated with the administrated ephedrine dose than the weight of the fetus, which was described by the coefficient of determination of the SFH, (25%) (Table 5).
Factors that affect the anesthesia level of spinal anesthesia include the properties of cerebrospinal fluid, characteristics of the patient, the injection method and the properties of the local anesthetic. Among these factors, the height of the patient has been recognized as a factor that is strongly related to the diffusion of local anesthesia in the subarachnoid space, and many anesthetists actually carry out spinal anesthesia using different doses of local anesthetic depending on the height of the patients. There are many studies regarding whether the height and weight of parturient women who undergo Cesarean section are correlated with the level of anesthesia. Norris [4,6] reported that no correlation was found among the height and weight and the level of anesthesia when spinal anesthesia with 0.75% hyperbaric bupivacaine was used for parturient women. Hartwell et al. [7] also reported that when spinal anesthesia was performed with 0.75% hyperbaric bupivacaine, no correlation was found between the height and the level of spinal anesthesia, but a correlation was found between the length of the spine and the level of anesthesia. It is known that one of the causes of high spinal anesthesia, in addition to the height and weight of the parturient women, is that the lumbosacral subarachnoidal space volume is decreased as the plexus venosus collateral circulation is developed in the epidural space by the hypertrophic uterus [2,3]. Thus, we conducted this study considering that the SFH, which is an objective indicator of the uterus size measurement, may reasonably be a factor influencing high spinal anesthesia.
Hallworth et al. [8] reported that the specific gravity of a local anesthetic and the body position, significantly affect the occurrence of hypotension during spinal anesthesia in parturient women. To exclude the effect of the specific gravity of local anesthetic and the body position in this study, we employed one specific gravity and one kind of local anesthetic, and the body position of the parturient women was maintained as horizontal, except when it was tilted to the left by 15° to prevent supine hypotensive syndrome immediately after the spinal anesthesia [9].
The amount of fluid administrated in advance should be considered as a factor that can affect the maximum sensory blockade level and occurrence of hypotension. Shin et al. [10] reported that the crystalloid solution rapidly injected before the spinal anesthesia converted the flow of the cerebrospinal fluid to the direction of the lumbar region and consequently decreased the diffusion of the local anesthesia toward the cephalic region. In order to exclude difference in the maximum sensory blockade level and the hypotension incidents resulting from the amount of fluid administrated in advance, the Hartmann crystalloid solution (15 ml/kg) was injected for 20 minutes prior to the anesthesia, in the same manner, to all the target parturient women in this study, and the blood pressure measured after the injection was considered as the reference value. Tuominen et al. [11] reported that the injection rate of 0.5% plain bupivacaine affected the diffusion of the local anesthetic in spinal anesthesia. In this study, we injected the drug in all the parturient women at the rate of 0.1 ml/sec, to exclude differences in the level of the spinal anesthesia caused by the injection rate.
Danelli et al. [12] studied the optimum dose of 0.5% hyperbaric bupivacaine for the Cesarean section of parturient women and reported that a dose of ~9.5-10.5 mg was effective for 95% of the parturient women. They also reported that 10 mg was the minimum dose to maintain appropriate anesthesia, but hypotension was found in 65% of the patients in the case. In this study, the dose of the local anesthetic was determined using the table suggested by Harten et al. [5] in order to exclude the variations by height and weight. Since Lee et al. [13] reported that hypotension was reduced when administering the ephedrine dose suggested by Harten et al. [5] in comparison to administering a fixed dose to Korean parturient women, we thought that the method of Harten et al. [5], that considers the height and weight of the parturient women for spinal anesthesia, might be more appropriate.
Oh and Hong [14] reported that the addition of fentanyl could reduce the dose of the local anesthesia and hypotension incidents, while providing appropriate anesthesia for the operation. Although we applied the local anesthetic dose suggested by Harten et al. [5] in this study, we used fentanyl (20 µg), whereas diamorphine (0.4 mg) was used in the study of Harten et al. [5]. The average bupivacaine dose used was about 9.5 mg, which was 0.5 mg less than the dose used by Danelli et al. [12]. Ephedrine was administrated in 53.8% of the cases, which was similar to 56.8% in the study of Harten et al. [5].
Hypotension is the most common side effect found at the anesthesia region after Cesarean section. The causes of nausea and vomiting include cerebral ischemia by blood pressure drop, hyperfunction of the vagus nerve, intraoperative intestine traction, and preanesthetic administration. When hypotension, nausea, and vomiting occurred after the spinal anesthesia in this study, ephedrine was administrated to treat the nausea and vomiting accompanying hypotension. In the study of Kol et al. [15], it was reported that the incident of hypotension, as well as the incident of nausea and vomiting, was effectively reduced in the group of parturient women to whom ephedrine was administrated during the spinal anesthesia for Cesarean section. Since all nausea and vomiting cases were accompanied by hypotension, blood pressure drop was presumably the cause of the nausea and vomiting that took place after the spinal anesthesia and during the operation.
Higuchi et al. [3] reported that the density and volume of the cerebrospinal fluid affects the diffusion of local anesthetic during spinal anesthesia. They also reported that the sensory blockade level was elevated and the duration of motor blockade action was shortened as the cerebrospinal fluid was less. In the case of parturient women, the diffusion of local anesthetic toward the direction of the cranial cavity can be enhanced by pressure on the inferior vena cava by the hypertrophic uterus, shrinkage of the subarachnoid space by the expansion of the lumbar vein and vertebral artery around the spinal cavity, and the reduction of cerebrospinal fluid [2,3]. The SFH was measured in this study to calculate the actual size of the uterus, and was done by doctors in the obstetrics and gynecology department. To exclude the variations resulting from measurement by different individuals, one single examiner measured the SFH and the data were not provided to the anesthetist. However, contrary to our expectation, the SFH did not show a significant correlation with the maximum sensory blockade level in this study. Kim et al. [16] also reported that the SFH and the cerebrospinal pressure were not significantly correlated with the sensory blockade level. In this study, however, it was found that the weight of the fetus and the SFH were significantly correlated with the amount of ephedrine administrated for hypotension. In particular, it was found that the SFH was more strongly correlated with the amount of administrated ephedrine than with the weight of the fetus. This may be because the amount of ephedrine administrated for hypotension after the spinal anesthesia was increased as the SFH was higher, since the aortic vein was more strongly pressed when the SFH was higher. In this study, the table was tilted by 15° to the left to prevent supine hypotensive syndrome, but according to Bravema [17], there are some cases where the wedge under the right hip should be heightened by about 30° if the uterus is large, because of plural pregnancy or hydramnion. Hence, in the case of a large uterus, careful attention needs to be paid to prevent hypotension, by avoiding the aortic vein pressure. In addition, research needs to be conducted to study the degree of aortic vein pressure according to the size of the uterus.
Although a hypertrophic uterus is usually because of the fetus, except in the cases of hydramnion, uterine myoma, or uterine anomaly, the size of the uterus may vary depending on the amount of amniotic fluid. Thus, the determination coefficient of the weight of the newborn baby is smaller than that of the SFH. In this study, the SFH was more strongly correlated with the amount of ephedrine administrated for hypotension than with the weight of the newborn baby.
In conclusion, although the SFH was not correlated with the maximum sensory blockade during the spinal anesthesia for Cesarean section, it was correlated with the amount of ephedrine administrated for hypotension, which may be correlated with the aortic vein pressure. Increasing the gradient of the left anterior region of the uterus is also needed to prevent hypotension if the size of the uterus is large.
References
1. Birnbach DJ, Brown IM. Miller RD, editor. Anesthesia for obstetrics. Miller's Anesthesia. 2005. 6th ed. Philadelphia: Elsevier/Churchill Livingstone;p. 2324.

2. Jawan B, Lee JH, Chong ZK, Chang CS. Spread of spinal anaesthesia for caesarean section in singleton and twin pregnancies. Br J Anaesth. 1993; 70:639–641. PMID: 8329257.

3. Higuchi H, Hirata J, Adachi Y, Kazama T. Influence of lumbosacral cerebrospinal fluid density, velocity, and volume on extent and duration of plain bupivacaine spinal anesthesia. Anesthesiology. 2004; 100:106–114. PMID: 14695731.

4. Norris MC. Patient variables and the subarachnoid spread of hyperbaric bupivacaine in the term parturient. Anesthesiology. 1990; 72:478–482. PMID: 2310028.

5. Harten JM, Boyne I, Hannah P, Varveris D, Brown A. Effects of a height and weight adjusted dose of local anaesthetic for spinal anaesthesia for elective Caesarean section. Anaesthesia. 2005; 60:348–353. PMID: 15766337.

6. Norris MC. Height, weight, and the spread of subarachnoid hyperbaric bupivacaine in the term parturient. Anesth Analg. 1988; 67:555–558. PMID: 3377210.

7. Hartwell BL, Aglio LS, Hauch MA, Datta S. Vertebral column length and spread of hyperbaric subarachnoid bupivacaine in the term parturient. Reg Anesth. 1991; 16:17–19. PMID: 2007099.
8. Hallworth SP, Fernando R, Columb MO, Stocks GM. The effect of posture and baricity on the spread of intrathecal bupivacaine for elective cesarean delivery. Anesth Analg. 2005; 100:1159–1165. PMID: 15781538.

9. Birnbach DJ, Brown IM. Miller RD, editor. Anesthesia for obstetrics. Miller's Anesthesia. 2005. 6th ed. Philadelpia: Elsevier/Churchill Livingstone;p. 2308–2309.

10. Shin BS, Ko JS, Gwak MS, Yang M, Kim CS, Hahm TS, et al. The effects of prehydration on the properties of cerebrospinal fluid and the spread of isobaric spinal anesthetic drug. Anesth Analg. 2008; 106:1002–1007. PMID: 18292453.

11. Tuominen M, Pitkänen M, Rosenberg PH. Effect of speed of injection of 0.5% plain bupivacaine on the spread of spinal anaesthesia. Br J Anaesth. 1992; 69:148–149. PMID: 1389816.

12. Danelli G, Zangrillo A, Nucera D, Giorgi E, Fanelli G, Senatore R, et al. The minimum effective dose of 0.5% hyperbaric spinal bupivacaine for cesarean section. Minerva Anestesiol. 2001; 67:573–577. PMID: 11602876.
13. Lee C, Son Y, Yoon JS, Cheong YK, Kim MS. Effects of adjusted dose of local anesthetic considered patient's characteristics for spinal anesthesia for elective cesarean section. Korean J Anesthesiol. 2005; 49:641–645.
14. Oh JI, Hong JY. Clinical effects of low-dose bupivacaine with fentanyl for cesarean section. J Korean Soc Obstet Anesth. 2005; 8:14–18.
15. Kol IO, Kaygusuz K, Gursoy S, Cetin A, Kahramanoglu Z, Ozkan F, et al. The effects of intravenous ephedrine during spinal anesthesia for cesarean delivery: a randomized controlled trial. J Korean Med Sci. 2009; 24:883–888. PMID: 19794988.

16. Kim EJ, Lee JH, Ban JS, Min BW. Patient variables influencing the sensory blockade level of spinal anesthesia using hyperbaric bupivacaine in term parturients. Korean J Anesthesiol. 2003; 45:627–631.

17. Braveman FR. Hines RL, editor. Obstetric and Gynecologic Anesthesia: the requisites in Anesthesiology. 2006. Connecticut: Churchill Livingstone;p. 62.
Fig. 2
Relationship between total administered dose of ephedrine and symphysis-fundal height (SFH) after spinal anesthesia in 52 term parturients. It shows that regression coefficient is 2.06 and P value is 0.0002.
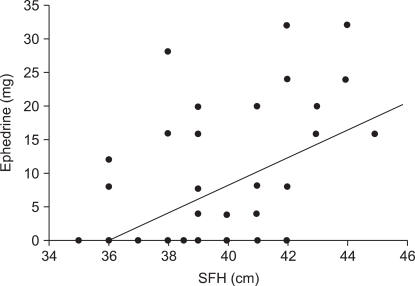
Fig. 3
Relationship between total administered dose of ephedrine and baby weight after spinal anesthesia in 52 term parturients. Illustrates that regression coefficient is 0.0082 and P value is 0.0136.
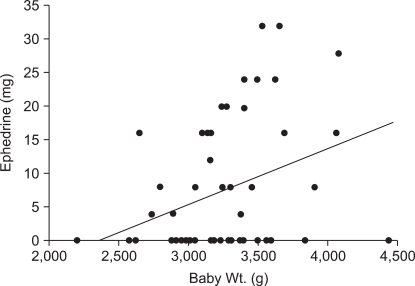
Table 1
Adjusted Dose Regimen for 0.5% Hyperbaric Bupivacaine when Used for Spinal Anesthesia for Cesarean Section (ml)




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download